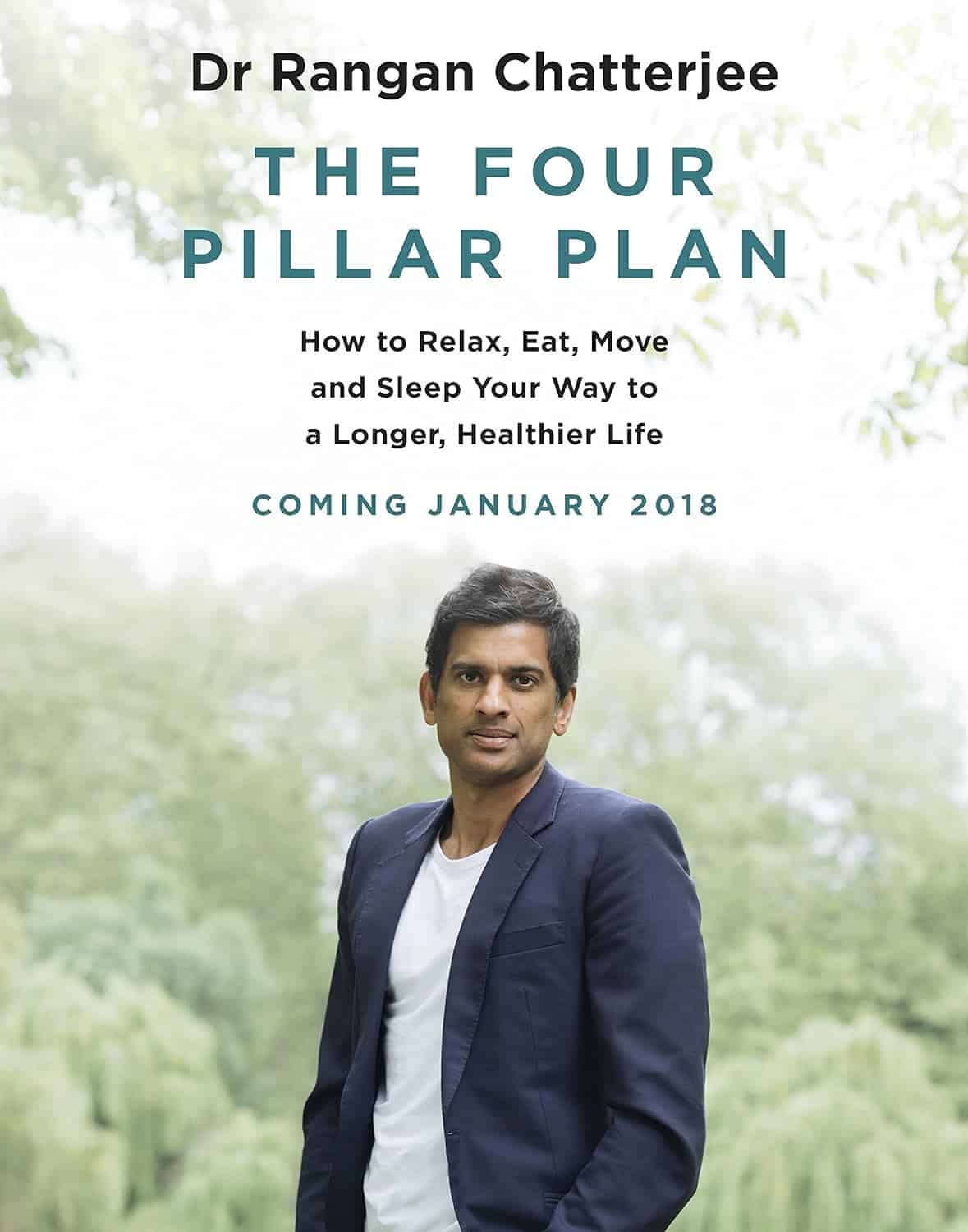
The Four Pillar Plan – by Dr. Rangan Chatterjee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Rangan Chatterjee, a medical doctor, felt frustrated with how many doctors in his field focus on treating the symptoms of disease, rather than the cause. Sometimes, of course, treating the symptom is necessary too! But neglecting the cause is a recipe for long-term woes.
What he does differently is take lifestyle as a foundation, and even that, he does differently than many authors on the topic. How so, you may wonder?
Rather than look first at exercise and diet, he starts with “relax”. His rationale is reasonable: diving straight in with marathon training or a whole new diet plan can be unsustainable without this as a foundation to fall back on.
Many sources look first at exercise (because it can be a very simple “prescription”) before diet (often more complex)… but how does one exercise well with the wrong fuel in the tank? So Dr. Chatterjee’s titular “Four Pillars” come in the following order:
- Relax
- Eat
- Move
- Sleep
He also goes for “move” rather than “exercise” as the focus here is more on minimizing time spent sitting, and thus involving a lot of much more frequent gentle activities… rather than intensive training programs and the like.
And as for sleep? Yes, that comes last because—no matter how important it is—the other things are easier to directly control. After all, one can improve conditions for sleep, but one cannot simply choose to sleep better! So with the other three things covered first, good sleep is the fourth and final thing to fall into place.
All in all, this is a great book to cut through the catch-22 problem of lifestyle factors negatively impacting each other.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Five Invitations – by Frank Ostaseski
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book covers exactly what its subtitle promises, and encourages the reader to truly live life fully, something that Ostaseski believes cannot be done in ignorance of death.
Instead, he argues from his experience of decades working at a hospice, we must be mindful of death not only to appreciate life, but also to make the right decisions in life—which means responding well to what he calls, as per the title of this book, “the five invitations”.
We will not keep them a mystery; they are:
- Don’t wait; do the important things now
- Welcome everything; push away nothing
- Bring your whole self to the experience
- Find a place in the middle of things
- Cultivate a “don’t know” mind
Note, for example, that “do the important things now” requires knowing what is important. For example, ensuring a loved one knows how you feel about them, might be more important than scratching some item off a bucket list. And “push away nothing” does mean bad things too; rather, of course try to make life better rather than worse, but accept the lessons and learnings of the bad too, and see the beauty that can be found in contrast to it. Enjoying the fullness of life without getting lost in it; carrying consciousness through the highs and lows. And yes, approaching the unknown (which means not only death, but also the large majority of life) with open-minded curiosity and wonder.
The style of the book is narrative and personal, without feeling like a collection of anecdotes, but rather, taking the reader on a journey, prompting reflection and introspection along the way.
Bottom line: if you’d like to minimize the regrets you have in life, this book is a fine choice.
Click here to check out The Five Invitations, and answer with a “yes” to the call of life!
Share This Post
-
The Alzheimer’s Gene That Varies By Race & Sex
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Alzheimer’s Gene That Varies By Race & Sex
You probably know that there are important genetic factors that increase or decrease Alzheimer’s Risk. If you’d like a quick refresher before we carry on, here are two previous articles on this topic:
- Genetic Testing: Health Benefits & Methods (about personal genomics and health, including Alzheimer’s)
- The Surprising Link Between Type 2 Diabetes & Alzheimer’s (about the APOE-ε4 allele that is implicated in both)
A Tale of Two Alleles
It has generally been understood that APOE-ε2 lowers Alzheimer’s disease risk, and APOE-ε4 increases it.
However, for reasons beyond the scope of this article, research populations for genetic testing are overwhelmingly white. If you, dear reader, are white, you may be thinking “well, I’m white, so this isn’t a problem for me”, you might still want to read on…
An extensive new study, published days ago, by Dr. Belloy et al., looked at how these correlations held out per race and sex. They found:
- The “APOE-ε2 lowers; APOE-ε4 increases” dictum held out strongest for white people.
- In the case of Hispanic people, there was only a small correlation on the APOE-ε4 side of things, and none on the APOE-ε2 side of things per se.
- East Asians also saw no correlation with regard to APOE-ε2 per se.
- But! Hispanic and East Asian people had a reduced risk of Alzheimer’s if and only if they had both APOE-ε2 and APOE-ε4.
- Black people, meanwhile, saw a slight correlation with regard to the protective effect of APOE-ε2, and as for APOE-ε4, if they had any European ancestry, increased European ancestry meant a higher increased risk factor if they had APOE-ε4. African ancestry, on the other hand, had a protective effect, proportional to the overall amount of that ancestry.
And as for sex…
- Specifically for white people with the APOE-ε3/ε4 genotype, especially in the age range of 60–70, the genetic risk for Alzheimer’s was highest in women.
If you’d like to read more and examine the data for yourself:
APOE Genotype and Alzheimer Disease Risk Across Age, Sex, and Population Ancestry
Want to reduce your Alzheimer’s risk?
We have just the thing for you:
How To Reduce Your Alzheimer’s Risk: It’s Never Too Early To Do These 11 Things
Take care!
Share This Post
-
Peas vs Broad Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing peas to broad beans, we picked the peas.
Why?
Both are great of course, but…
Looking at the macros to start with, peas have more protein and more fiber. The differences aren’t huge, but they are clear.
In terms of vitamins, peas have more of vitamins A, B1, B2, B3, B5, B6, B9, E, K, and choline (some with very large margins, some with small), while broad beans contain a little more vitamin C (the margin is quite narrow though).
When it comes to minerals, peas have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while broad beans have more sodium. So this category wasn’t close.
Adding up the win from each of the categories makes for a clear triple-win for peas.
Easy-peasy!
Want to learn more?
You might like to read:
Take care!
Share This Post
Related Posts
-
Get The Right Help For Your Pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Much Does It Hurt?
Sometimes, a medical professional will ask us to “rate your pain on a scale of 1–10”.
It can be tempting to avoid rating one’s pain too highly, because if we say “10” then where can we go from there? There is always a way to make pain worse, after all.
But that kind of thinking, however logical, is folly—from a practical point of view. Instead of risking having to give an 11 later, you have now understated your level-10 pain as a “7” and the doctor thinks “ok, I’ll give Tylenol instead of morphine”.
A more useful scale
First, know this:
Zero is not “this is the lowest level of pain I get to”.
Zero is “no pain”.
As for the rest…
- My pain is hardly noticeable.
- I have a low level of pain; I am aware of my pain only when I pay attention to it.
- My pain bothers me, but I can ignore it most of the time.
- I am constantly aware of my pain, but can continue most activities.
- I think about my pain most of the time; I cannot do some of the activities I need to do each day because of the pain.
- I think about my pain all of the time; I give up many activities because of my pain.
- I am in pain all of the time; It keeps me from doing most activities.
- My pain is so severe that it is difficult to think of anything else. Talking and listening are difficult.
- My pain is all that I can think about; I can barely move or talk because of my pain.
- I am in bed and I can’t move due to my pain; I need someone to take me to the emergency room because of my pain.
10almonds tip: are you reading this on your phone? Screenshot the above, and keep it for when you need it!
One extra thing to bear in mind…
Medical staff will be more likely to believe a pain is being overstated, on a like-for-like basis, if you are a woman, or not white, or both.
There are some efforts to compensate for this:
A new government inquiry will examine women’s pain and treatment. How and why is it different?
Some other resources of ours:
- The 7 Approaches To Pain Management ← a pain specialist discusses the options available
- Managing Chronic Pain (Realistically!) ← when there’s no quick fix, but these things can buy you some hours’ relief at least / stop the pain from getting worse in the moment
- Science-Based Alternative Pain Relief ← for when you’re maxxed out on painkillers, and need something more/different, these are the things the science says will work
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Breaking Free from Emotional Eating – Geneen Roth
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The isn’t a book about restrictive dieting, or even willpower. Rather, it’s about making the unconscious conscious, and changing your relationship with food from being one of compulsion, to one of choice, wherein you also get the choice of saying “no”.
Roth takes us through the various ways in which life seems to conspire to take consciousness away from eating, from obvious distractions such as TV, to less obvious ones, like “it doesn’t count if you’re not sitting down”. She also tackles other psychological aspects, such as those people get from parents—which can be a big factor for many.
Importantly, she teaches us that when it comes to “have your cake and eat it”, you can also, in fact, have your cake and not eat it. That’s an option too. Its mere presence in our house is not the boss of us. However, overcoming the “this then that” automatic process that goes from having to eating, is something that Roth gives quite some attention to, offering a number of reframes to make it a lot easier.
The style is friendly, conversational, pop-science, and the format dates it a little—this is very much a book formatted the way pop-science books were formatted 20–50 years ago (the book itself is from 2003, for what it’s worth). However, a lack of modern format doesn’t take away from its very valuable insights, and if anything, the older format rather promotes reading a book from cover to cover, which can be beneficial.
Bottom line: if emotional or compulsive eating is something that you’ve found tricky to overcome, then this book can help make it a lot easier.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Procrastination, and how to pay off the to-do list debt
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Procrastination, and how pay off the to-do list debt
Sometimes we procrastinate because we feel overwhelmed by the mountain of things we are supposed to be doing. If you look at your to-do list and it shows 60 overdue items, it’s little wonder if you want to bury your head in the sand!
“What difference does it make if I do one of these things now; I will still have 59 which feels as bad as having 60”
So, treat it like you might a financial debt, and make a repayment plan. Now, instead of 60 overdue items today, you have 1/day for the next 60 days, or 2/day for the next 30 days, or 3/day for the next 20 days, etc. Obviously, you may need to work out whether some are greater temporal priorities and if so, bump those to the top of the list. But don’t sweat the minutiae; your list doesn’t have to be perfectly ordered, just broadly have more urgent things to the top and less urgent things to the bottom.
Note: this repayment plan means having set repayment dates.
Up front, sit down and assign each item a specific calendar date on which you will do that thing.
This is not a deadline! It is your schedule. You’ll not try to do it sooner, and you won’t postpone it for later. You will just do that item on that date.
A productivity app like ToDoist can help with this, but paper is fine too.
What’s important here, psychologically, is that each day you’re looking not at 60 things and doing the top item; you’re just looking at today’s item (only!) and doing it.
Debt Reduction/Cancellation
Much like you might manage a financial debt, you can also look to see if any of your debts could be reduced or cancelled.
We wrote previously about the “Getting Things Done” system. It’s a very good system if you want to do that; if not, no worries, but you might at least want to borrow this one idea….
Sort your items into:
Do / Defer / Delegate / Ditch
- Do: if it can be done in under 2 minutes, do it now.
- Defer: defer the item to a specific calendar date (per the repayment plan idea we just talked about)
- Delegate: could this item be done by someone else? Get it off your plate if you reasonably can.
- Ditch: sometimes, it’s ok to realize “you know what, this isn’t that important to me anymore” and scratch it from the list.
As a last resort, consider declaring bankruptcy
Towards the end of the dot-com boom, there was a fellow who unintentionally got his 5 minutes of viral fame for “declaring email bankruptcy”.
Basically, he publicly declared that his email backlog had got so far out of hand that he would now not reply to emails from before the declaration.
He pledged to keep on top of new emails only from that point onwards; a fresh start.
We can’t comment on whether he then did, but if you need a fresh start, that can be one way to get it!
In closing…
Procrastination is not usually a matter of laziness, it’s usually a matter of overwhelm. Hopefully the above approach will help reframe things, and make things more manageable.
Sometimes procrastination is a matter of perfectionism, and not starting on tasks because we worry we won’t do them well enough, and so we get stuck in a pseudo-preparation rut. If that’s the case, our previous main feature on perfectionism may help:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: