The 5 Resets – by Dr. Aditi Nerurkar
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What this book isn’t: an advice to go on a relaxing meditation retreat, or something like that.
What this is: a science-based guide to what actually works.
There’s no need to be mysterious, so we’ll mention that the titular “5 resets” are:
- What matters most
- Quiet in a noisy world
- Leveraging the brain-body connection
- Coming up for air (regaining perspective)
- Bringing your best self forward
All of these are things we can easily lose sight of in the hustle and bustle of daily life, so having a system for keeping them on track can make a huge difference!
The style is personable and accessible, while providing a lot of strongly science-backed tips and tricks along the way.
Bottom line: if life gets away from you a little too often for comfort, this book can help you keep on top of things with a lot less stress.
Click here to check out “The 5 Resets”, and take control with conscious calm!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
10 Ways To Lower Blood Pressure Naturally
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Increasingly many people, especially over a certain age, are taking so many medications that it precipitates a train of other medications to deal with the side effects of the previous ones. This is neither fun nor healthy. Of course, sometimes it’s a necessity, but often it’s not, so if you’d like to avoid blood pressure meds, here are some good first-line things, as recommended by Dr. Siobhan Deshauer:
No-med options
Dr. Deshauer recommends:
- Diet: follow the DASH diet by eating whole foods, lean / plant-based proteins, and reducing salt and processed foods to lower blood pressure by 5–6 points.
- Sodium reduction: limit sodium intake to 2g/day, focusing on reducing processed foods, which account for 80% of sodium consumption.
- Increase potassium intake: eat potassium-rich foods (e.g. fruit, vegetables) to lower blood pressure by 5–7 points but consult a doctor if you have kidney issues or take certain medications.
- Exercise: engage in isometric exercises like wall squats or planks, which lower systolic pressure by up to 8 points; any exercise is beneficial.
- Weight loss: lose weight (specifically: fat) if (and only if!) carrying excess fat, as each 1 kg (2.2 lbs) excess adiposity reduction can decrease blood pressure by 1 point.
- Limit alcohol: avoid consuming more than two alcoholic drinks per day, as it raises blood pressure.
- Quit smoking: stop smoking to prevent increased blood pressure and long-term vessel damage caused by nicotine.
- Improve sleep: aim for at least 6 hours of sleep per night, ideally 7–9, and seek medical advice if you suspect sleep apnea.
- Manage stress: adopt healthy stress management strategies to avoid the indirect effects of stress on blood pressure.
- Adopt a pet: pet ownership, particularly dogs, can lower blood pressure more effectively than some medications.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Ideal Blood Pressure Numbers Explained
Take care!
Share This Post
-
HRT Side Effects & Troubleshooting
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Heather Hirsch. She’s a board-certified internist, and her clinical expertise focuses on women’s health, particularly in midlife and menopause, and its intersection with chronic diseases (ranging from things associated with sexual health, to things like osteoporosis and heart disease).
So, what does she want us to know?
HRT can be life-changingly positive, but it can be a shaky start
Hormone Replacement Therapy (HRT), and in this context she’s talking specifically about the most common kind, Menopausal Hormone Therapy (MHT), involves taking hormones that our body isn’t producing enough of.
If these are “bioidentical hormones” as used in most of the industrialized world and increasingly also in N. America, then this is by definition a supplement rather than a drug, for what it’s worth, whereas some non-bioidentical hormones (or hormone analogs, which by definition function similarly to hormones but aren’t the same thing) can function more like drugs.
We wrote a little about his previously:
Hormone Replacement Therapy: A Tale Of Two Approaches
For most people most of the time, bioidentical hormones are very much the best way to go, as they are not only more effective, but also have fewer side effects.
That said, even bioidentical hormones can have some undesired effects, so, how to deal with those?
Don’t worry; bleed happy
A reprise of (usually quite light) menstrual bleeding is the most common side effect of menopausal HRT.
This happens because estrogen affects* the uterus, leading to a build-up and shedding of the uterine lining.
*if you do not have a uterus, estrogen can effect uterine tissue. That’s not a typo—here we mean the verb “effect”, as in “cause to be”. It will not grow a new uterus, but it can cause some clumps of uterine tissue to appear; this means that it becomes possible to get endometriosis without having a uterus. This information should not be too shocking, as endometriosis is a matter of uterine tissue growing inconveniently, often in places where it shouldn’t, and sometimes quite far from the uterus (if present, or its usual location, if absent). However, the risk of this happening is far lower than if you actually have a uterus:
What you need to know about endometriosis
Back to “you have a uterus and it’s making you wish you didn’t”:
This bleeding should, however, be light. It’ll probably be oriented around a 28-day cycle even if you are taking your hormones at the same dose every day of the month, and the bleeding will probably taper off after about 6 months of this.
If the bleeding is heavier, all the time, or persists longer than 6 months, then speak to your gynecologist about it. Any of those three; it doesn’t have to be all three!
Bleeding outside of one’s normal cycle can be caused by anything from fibroids to cancer; statistically speaking it’s probably nothing too dire,but when your safety is in question, don’t bet on “probably”, and do get it checked out:
When A Period Is Very Late (i.e., Post-Menopause)
Dr. Hirsch recommends, as possible remedies to try (preferably under your gynecologist’s supervision):
- lowering your estrogen dose
- increasing your progesterone dose
- taking progesterone continuously instead of cyclically
And if you’re not taking progesterone, here’s why you might want to consider taking this important hormone that works with estrogen to do good things, and against estrogen to rein in some of estrogen’s less convenient things:
Progesterone Menopausal HRT: When, Why, And How To Benefit
(the above link contains, as well as textual information, an explanatory video from Dr. Hirsch herself)
Get the best of the breast
Calm your tits. Soothe your boobs. Destress your breasts. Hakuna your tatas. Undo the calamity beleaguering your mammaries.
Ok, more seriously…
Breast tenderness is another very common symptom when starting to take estrogen. It can worry a lot of people (à la “aagh, what is this and is it cancer!?”), but is usually nothing to worry about. But just to be sure, do also check out:
Keeping Abreast Of Your Cancer Risk: How To Triple Your Breast Cancer Survival Chances
Estrogen can cause feelings of breast fullness, soreness, nipple irritation, and sometimes lactation, but this later will be minimal—we’re talking a drop or two now and again, not anything that would feed a baby.
Basically, it happens when your body hasn’t been so accustomed to normal estrogen levels in a while, and suddenly wakes up with a jolt, saying to itself “Wait what are we doing puberty again now? I thought we did menopause? Are we pregnant? What’s going on? Ok, checking all systems!” and then may calm down not too long afterwards when it notes that everything is more or less as it should be already.
If this persists or is more than a minor inconvenience though, Dr. Hirsch recommends looking at the likely remedies of:
- Adjust estrogen (usually the cause)
- Adjust progesterone (less common)
- If it’s progesterone, changing the route of administration can ameliorate things
What if it’s not working? Is it just me?
Dr. Hirsch advises the most common reasons are simply:
- wrong formulation (e.g. animal-derived estrogen or hormone analog, instead of bioidentical)
- wrong dose (e.g. too low)
- wrong route of administration (e.g. oral vs transdermal; usually transdermal estradiol is most effective but many people do fine on oral; progesterone meanwhile is usually best as a pessary/suppository, but many people do fine on oral)
Writer’s example: in 2022 there was an estrogen shortage in my country, and while I had been on transdermal estradiol hemihydrate gel, I had to go onto oral estradiol valerate tablets for a few months, because that’s what was available. And the tablets simply did not work for me at all. I felt terrible and I have a good enough intuitive sense of my hormones to know when “something wrong is not right”, and a good enough knowledge of the pharmacology & physiology to know what’s probably happening (or not happening). And sure enough, when I got my blood test results, it was as though I’d been taking nothing. It was such a relief to get back on the gel once it became available again!
So, if something doesn’t seem to be working for you, speak up and get it fixed if at all possible.
See also: What You Should Have Been Told About Menopause Beforehand
Want to know more from Dr. Hirsch?
You might like this book of hers, which we haven’t reviewed yet, but present here for your interest:
Enjoy!
Share This Post
-
How Does One Test Acupuncture Against Placebo Anyway?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pinpointing The Usefulness Of Acupuncture
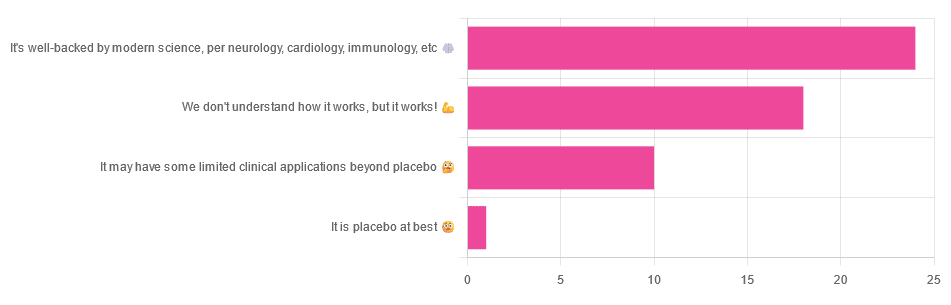
We asked you for your opinions on acupuncture, and got the above-depicted, below-described, set of answers:
- A little under half of all respondents voted for “It’s well-backed by modern science, per neurology, cardiology, immunology, etc”
- Slightly fewer respondents voted for “We don’t understand how it works, but it works!”
- A little under a fifth of respondents voted for “It may have some limited clinical applications beyond placebo”
- One (1) respondent voted for for “It’s placebo at best”
When we did a main feature about homeopathy, a couple of subscribers wrote to say that they were confused as to what homeopathy was, so this time, we’ll start with a quick definition first.
First, what is acupuncture? For the convenience of a quick definition so that we can move on to the science, let’s borrow from Wikipedia:
❝Acupuncture is a form of alternative medicine and a component of traditional Chinese medicine in which thin needles are inserted into the body.
Acupuncture is a pseudoscience; the theories and practices of TCM are not based on scientific knowledge, and it has been characterized as quackery.❞
Now, that’s not a promising start, but we will not be deterred! We will instead examine the science itself, rather than relying on tertiary sources like Wikipedia.
It’s worth noting before we move on, however, that there is vigorous debate behind the scenes of that article. The gist of the argument is:
- On one side: “Acupuncture is not pseudoscience/quackery! This has long been disproved and there are peer-reviewed research papers on the subject.”
- On the other: “Yes, but only in disreputable quack journals created specifically for that purpose”
The latter counterclaim is a) potentially a “no true Scotsman” rhetorical ploy b) potentially true regardless
Some counterclaims exhibit specific sinophobia, per “if the source is Chinese, don’t believe it”. That’s not helpful either.
Well, the waters sure are muddy. Where to begin? Let’s start with a relatively easy one:
It may have some clinical applications beyond placebo: True or False?
True! Admittedly, “may” is doing some of the heavy lifting here, but we’ll take what we can get to get us going.
One of the least controversial uses of acupuncture is to alleviate chronic pain. Dr. Vickers et al, in a study published under the auspices of JAMA (a very respectable journal, and based in the US, not China), found:
❝Acupuncture is effective for the treatment of chronic pain and is therefore a reasonable referral option. Significant differences between true and sham acupuncture indicate that acupuncture is more than a placebo.
However, these differences are relatively modest, suggesting that factors in addition to the specific effects of needling are important contributors to the therapeutic effects of acupuncture❞
Source: Acupuncture for Chronic Pain: Individual Patient Data Meta-analysis
If you’re feeling sharp today, you may be wondering how the differences are described as “significant” and “relatively modest” in the same text. That’s because these words have different meanings in academic literature:
- Significant = p<0.05, where p is the probability of the achieved results occurring randomly
- Modest = the differences between the test group and the control group were small
In other words, “significant modest differences” means “the sample sizes were large, and the test group reliably got slightly better results than placebo”
We don’t understand how it works, but it works: True or False
Broadly False. When it works, we generally have an idea how.
Placebo is, of course, the main explanation. And even in examples such as the above, how is placebo acupuncture given?
By inserting acupuncture needles off-target rather than in accord with established meridians and points (the lines and dots that, per Traditional Chinese Medicine, indicate the flow of qi, our body’s vital energy, and welling-points of such).
So, if a patient feels that needles are being inserted randomly, they may no longer have the same confidence that they aren’t in the control group receiving placebo, which could explain the “modest” difference, without there being anything “to” acupuncture beyond placebo. After all, placebo works less well if you believe you are only receiving placebo!
Indeed, a (Korean, for the record) group of researchers wrote about this—and how this confounding factor cuts both ways:
❝Given the current research evidence that sham acupuncture can exert not only the originally expected non-specific effects but also sham acupuncture-specific effects, it would be misleading to simply regard sham acupuncture as the same as placebo.
Therefore, researchers should be cautious when using the term sham acupuncture in clinical investigations.❞
Source: Sham Acupuncture Is Not Just a Placebo
It’s well-backed by modern science, per neurology, cardiology, immunology, etc: True or False?
False, for the most part.
While yes, the meridians and points of acupuncture charts broadly correspond to nerves and vasculature, there is no evidence that inserting needles into those points does anything for one’s qi, itself a concept that has not made it into Western science—as a unified concept, anyway…
Note that our bodies are indeed full of energy. Electrical energy in our nerves, chemical energy in every living cell, kinetic energy in all our moving parts. Even, to stretch the point a bit, gravitational potential energy based on our mass.
All of these things could broadly be described as qi, if we so wish. Indeed, the ki in the Japanese martial art of aikido is the latter kinds; kinetic energy and gravitational potential energy based on our mass. Same goes, therefore for the ki in kiatsu, a kind of Japanese massage, while the ki in reiki, a Japanese spiritual healing practice, is rather more mystical.
The qi in Chinese qigong is mostly about oxygen, thus indirectly chemical energy, and the electrical energy of the nerves that are receiving oxygenated blood at higher or lower levels.
On the other hand, the efficacy of the use of acupuncture for various kinds of pain is well-enough evidenced. Indeed, even the UK’s famously thrifty NHS (that certainly would not spend money on something it did not find to work) offers it as a complementary therapy for some kinds of pain:
❝Western medical acupuncture (dry needling) is the use of acupuncture following a medical diagnosis. It involves stimulating sensory nerves under the skin and in the muscles.
This results in the body producing natural substances, such as pain-relieving endorphins. It’s likely that these naturally released substances are responsible for the beneficial effects experienced with acupuncture.❞
Source: NHS | Acupuncture
Meanwhile, the NIH’s National Cancer Institute recommends it… But not as a cancer treatment.
Rather, they recommend it as a complementary therapy for pain management, and also against nausea, for which there is also evidence that it can help.
Frustratingly, while they mention that there is lots of evidence for this, they don’t actually link the studies they’re citing, or give enough information to find them. Instead, they say things like “seven randomized clinical trials found that…” and provide links that look reassuring until one finds, upon clicking on them, that it’s just a link to the definition of “randomized clinical trial”:
Source: NIH | Nactional Cancer Institute | Acupuncture (PDQ®)–Patient Version
However, doing our own searches finds many studies (mostly in specialized, potentially biased, journals such as the Journal of Acupuncture and Meridian Studies) finding significant modest outperformance of [what passes for] placebo.
Sometimes, the existence of papers with promising titles, and statements of how acupuncture might work for things other than relief of pain and nausea, hides the fact that the papers themselves do not, in fact, contain any evidence to support the hypothesis. Here’s an example:
❝The underlying mechanisms behind the benefits of acupuncture may be linked with the regulation of the hypothalamic-pituitary-gonadal (adrenal) axis and activation of the Wnt/β-catenin and OPG/RANKL/RANK signaling pathways.
In summary, strong evidence may still come from prospective and well-designed clinical trials to shed light on the potential role of acupuncture in preserving bone loss❞
Source: Acupuncture for Osteoporosis: a Review of Its Clinical and Preclinical Studies
So, here they offered a very sciencey hypothesis, and to support that hypothesis, “strong evidence may still come”.
“We must keep faith” is not usually considered evidence worthy of inclusion in a paper!
PS: the above link is just to the abstract, because the “Full Text” link offered in that abstract leads to a completely unrelated article about HIV/AIDS-related cryptococcosis, in a completely different journal, nothing to do with acupuncture or osteoporosis).
Again, this is not the kind of professionalism we expect from peer-reviewed academic journals.
Bottom line:
Acupuncture reliably performs slightly better than sham acupuncture for the management of pain, and may also help against nausea.
Beyond placebo and the stimulation of endorphin release, there is no consistently reliable evidence that is has any other discernible medical effect by any mechanism known to Western science—though there are plenty of hypotheses.
That said, absence of evidence is not evidence of absence, and the logistical difficulty of testing acupuncture against placebo makes for slow research. Maybe one day we’ll know more.
For now:
- If you find it helps you: great! Enjoy
- If you think it might help you: try it! By a licensed professional with a good reputation, please.
- If you are not inclined to having needles put in you unnecessarily: skip it! Extant science suggests that at worst, you’ll be missing out on slight relief of pain/nausea.
Take care!
Share This Post
Related Posts
-
Why You Can’t Deep Squat (And the Benefits You’re Missing)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Matt Hsu fought his own battle with chronic pain from the age of 16 in his feet, knees, hips, back, shoulders, elbows, forearms, wrists, hands, and head. Seeking answers, he’s spent a career in corrective exercise, posture alignment, structural integration, orthopedic exercise, sports medicine, and has more certifications than we care to list. In short, he knows his stuff.
Yes you can (with some work)
The deep squat, also called Asian squat, Slav squat, sitting squat, resting squat, primal squat, and various other names, is an important way of sitting that has implications for a lot of aspects of health.
Why it’s so important: it preserves the mobility of our hips, ankles, and everything in between, and maintaining especially the hip mobility makes a big difference not only to general health, but also to reducing the risk of injury. It also maintains lower body strength, making falls in older age less likely in the first place, and if falls do happen, makes injury less likely, and if injury does happen, makes the injury likely less severe.
An important misconception: there is a popular, but unfounded, belief that the ability or inability to do this is decided by genes—or if not outright decided, that at the very least Asians and Slavs have a genetic advantage. However, this is simply not true. Westerners and others can learn to do it just fine, and on the flipside, Asians and Slavs who grew up in the West may often struggle with it. The truth is, the deciding factor is lifestyle: if your culture involves sitting this way more often, you’ll be able to do it more comfortably and easily than if you’re just now trying it for the first time.
Factors that you can control: you can’t change where you grew up, but you can change how you sit down now. Achieving the squat requires repeated position practice, and the more frequently you do so (even if you just start with a few seconds and work your way up to longer periods), the better you’ll get at it. And, on the contrary, sitting in chairs weakens and shortens the muscles involved, so any time you spend sitting in chairs is working against you. There are many reasons it’s advisable to avoid sitting in chairs more than necessary, and this is one of them.
10almonds tip: a limiting factor for many people initially is ankle flexibility, which may result in one’s center of gravity being a bit far back, leading to a tendency to have to change something to avoid toppling over backwards. Rather than holding onto something immobile (e.g. furniture) in front of where you are sitting, consider simply holding an object in front of you in your hands. A book is a fine example; holding that in front of you (feel free to read the book) will shift your center of gravity forwards a bit, and will thus allow you to sit there a little longer, thus improving your strength and flexibility while you do, until you can do it without holding something in front of you. If you try with a book and you’re still prone to toppling backwards, try with something heavier, but do use the minimum weight necessary, because ultimately the counterbalance is just a crutch to get you to where you need to be.
For more visual advice on how to do it, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eat Real Food and Love It – by Kari McCloskey
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Half the battle of healthy eating is enjoying it—because once you do, it’s no longer a battle!
So that’s what this book focuses on. The author, a Registered Nutritionist, does indeed dispense nutritional advice, as you might expect, but also bids us pay attention to what nature’s foods do for us, and notice what less healthy foods take from us. She goes through these category by category, quite comprehensively, before moving on to the more “active” parts of the book.
There’s a lot about training our senses, and about taking a holistic approach to eating, as well as renewing not just our relationship with food, but also various other parts of our life that are inextricably linked to it (from sleep and exercise, to social considerations, and medical issues that healthier eating will help us to avoid or at least tame).
The style is… Joyful. Much like this reviewer, the author loves food, and it shows. She also (again much like this reviewer) cares deeply about the impact food has on her, and (for a third time: like this reviewer!) wants to share that joy and care with the reader. The priority is readability and helpfulness; scientific references are still provided wherever appropriate, though.
Bottom line: if you’d like to improve your eating but it seems like a chore, this book can help turn it into an excitingly enjoyable journey instead.
Click here to check out Eat Real Food And Love It, and eat real food and love it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Overdosing on Chemo: A Common Gene Test Could Save Hundreds of Lives Each Year
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One January morning in 2021, Carol Rosen took a standard treatment for metastatic breast cancer. Three gruesome weeks later, she died in excruciating pain from the very drug meant to prolong her life.
Rosen, a 70-year-old retired schoolteacher, passed her final days in anguish, enduring severe diarrhea and nausea and terrible sores in her mouth that kept her from eating, drinking, and, eventually, speaking. Skin peeled off her body. Her kidneys and liver failed. “Your body burns from the inside out,” said Rosen’s daughter, Lindsay Murray, of Andover, Massachusetts.
Rosen was one of more than 275,000 cancer patients in the United States who are infused each year with fluorouracil, known as 5-FU, or, as in Rosen’s case, take a nearly identical drug in pill form called capecitabine. These common types of chemotherapy are no picnic for anyone, but for patients who are deficient in an enzyme that metabolizes the drugs, they can be torturous or deadly.
Those patients essentially overdose because the drugs stay in the body for hours rather than being quickly metabolized and excreted. The drugs kill an estimated 1 in 1,000 patients who take them — hundreds each year — and severely sicken or hospitalize 1 in 50. Doctors can test for the deficiency and get results within a week — and then either switch drugs or lower the dosage if patients have a genetic variant that carries risk.
Yet a recent survey found that only 3% of U.S. oncologists routinely order the tests before dosing patients with 5-FU or capecitabine. That’s because the most widely followed U.S. cancer treatment guidelines — issued by the National Comprehensive Cancer Network — don’t recommend preemptive testing.
The FDA added new warnings about the lethal risks of 5-FU to the drug’s label on March 21 following queries from KFF Health News about its policy. However, it did not require doctors to administer the test before prescribing the chemotherapy.
The agency, whose plan to expand its oversight of laboratory testing was the subject of a House hearing, also March 21, has said it could not endorse the 5-FU toxicity tests because it’s never reviewed them.
But the FDA at present does not review most diagnostic tests, said Daniel Hertz, an associate professor at the University of Michigan College of Pharmacy. For years, with other doctors and pharmacists, he has petitioned the FDA to put a black box warning on the drug’s label urging prescribers to test for the deficiency.
“FDA has responsibility to assure that drugs are used safely and effectively,” he said. The failure to warn, he said, “is an abdication of their responsibility.”
The update is “a small step in the right direction, but not the sea change we need,” he said.
Europe Ahead on Safety
British and European Union drug authorities have recommended the testing since 2020. A small but growing number of U.S. hospital systems, professional groups, and health advocates, including the American Cancer Society, also endorse routine testing. Most U.S. insurers, private and public, will cover the tests, which Medicare reimburses for $175, although tests may cost more depending on how many variants they screen for.
In its latest guidelines on colon cancer, the Cancer Network panel noted that not everyone with a risky gene variant gets sick from the drug, and that lower dosing for patients carrying such a variant could rob them of a cure or remission. Many doctors on the panel, including the University of Colorado oncologist Wells Messersmith, have said they have never witnessed a 5-FU death.
In European hospitals, the practice is to start patients with a half- or quarter-dose of 5-FU if tests show a patient is a poor metabolizer, then raise the dose if the patient responds well to the drug. Advocates for the approach say American oncology leaders are dragging their feet unnecessarily, and harming people in the process.
“I think it’s the intransigence of people sitting on these panels, the mindset of ‘We are oncologists, drugs are our tools, we don’t want to go looking for reasons not to use our tools,’” said Gabriel Brooks, an oncologist and researcher at the Dartmouth Cancer Center.
Oncologists are accustomed to chemotherapy’s toxicity and tend to have a “no pain, no gain” attitude, he said. 5-FU has been in use since the 1950s.
Yet “anybody who’s had a patient die like this will want to test everyone,” said Robert Diasio of the Mayo Clinic, who helped carry out major studies of the genetic deficiency in 1988.
Oncologists often deploy genetic tests to match tumors in cancer patients with the expensive drugs used to shrink them. But the same can’t always be said for gene tests aimed at improving safety, said Mark Fleury, policy director at the American Cancer Society’s Cancer Action Network.
When a test can show whether a new drug is appropriate, “there are a lot more forces aligned to ensure that testing is done,” he said. “The same stakeholders and forces are not involved” with a generic like 5-FU, first approved in 1962, and costing roughly $17 for a month’s treatment.
Oncology is not the only area in medicine in which scientific advances, many of them taxpayer-funded, lag in implementation. For instance, few cardiologists test patients before they go on Plavix, a brand name for the anti-blood-clotting agent clopidogrel, although it doesn’t prevent blood clots as it’s supposed to in a quarter of the 4 million Americans prescribed it each year. In 2021, the state of Hawaii won an $834 million judgment from drugmakers it accused of falsely advertising the drug as safe and effective for Native Hawaiians, more than half of whom lack the main enzyme to process clopidogrel.
The fluoropyrimidine enzyme deficiency numbers are smaller — and people with the deficiency aren’t at severe risk if they use topical cream forms of the drug for skin cancers. Yet even a single miserable, medically caused death was meaningful to the Dana-Farber Cancer Institute, where Carol Rosen was among more than 1,000 patients treated with fluoropyrimidine in 2021.
Her daughter was grief-stricken and furious after Rosen’s death. “I wanted to sue the hospital. I wanted to sue the oncologist,” Murray said. “But I realized that wasn’t what my mom would want.”
Instead, she wrote Dana-Farber’s chief quality officer, Joe Jacobson, urging routine testing. He responded the same day, and the hospital quickly adopted a testing system that now covers more than 90% of prospective fluoropyrimidine patients. About 50 patients with risky variants were detected in the first 10 months, Jacobson said.
Dana-Farber uses a Mayo Clinic test that searches for eight potentially dangerous variants of the relevant gene. Veterans Affairs hospitals use a 11-variant test, while most others check for only four variants.
Different Tests May Be Needed for Different Ancestries
The more variants a test screens for, the better the chance of finding rarer gene forms in ethnically diverse populations. For example, different variants are responsible for the worst deficiencies in people of African and European ancestry, respectively. There are tests that scan for hundreds of variants that might slow metabolism of the drug, but they take longer and cost more.
These are bitter facts for Scott Kapoor, a Toronto-area emergency room physician whose brother, Anil Kapoor, died in February 2023 of 5-FU poisoning.
Anil Kapoor was a well-known urologist and surgeon, an outgoing speaker, researcher, clinician, and irreverent friend whose funeral drew hundreds. His death at age 58, only weeks after he was diagnosed with stage 4 colon cancer, stunned and infuriated his family.
In Ontario, where Kapoor was treated, the health system had just begun testing for four gene variants discovered in studies of mostly European populations. Anil Kapoor and his siblings, the Canadian-born children of Indian immigrants, carry a gene form that’s apparently associated with South Asian ancestry.
Scott Kapoor supports broader testing for the defect — only about half of Toronto’s inhabitants are of European descent — and argues that an antidote to fluoropyrimidine poisoning, approved by the FDA in 2015, should be on hand. However, it works only for a few days after ingestion of the drug and definitive symptoms often take longer to emerge.
Most importantly, he said, patients must be aware of the risk. “You tell them, ‘I am going to give you a drug with a 1 in 1,000 chance of killing you. You can take this test. Most patients would be, ‘I want to get that test and I’ll pay for it,’ or they’d just say, ‘Cut the dose in half.’”
Alan Venook, the University of California-San Francisco oncologist who co-chairs the panel that sets guidelines for colorectal cancers at the National Comprehensive Cancer Network, has led resistance to mandatory testing because the answers provided by the test, in his view, are often murky and could lead to undertreatment.
“If one patient is not cured, then you giveth and you taketh away,” he said. “Maybe you took it away by not giving adequate treatment.”
Instead of testing and potentially cutting a first dose of curative therapy, “I err on the latter, acknowledging they will get sick,” he said. About 25 years ago, one of his patients died of 5-FU toxicity and “I regret that dearly,” he said. “But unhelpful information may lead us in the wrong direction.”
In September, seven months after his brother’s death, Kapoor was boarding a cruise ship on the Tyrrhenian Sea near Rome when he happened to meet a woman whose husband, Atlanta municipal judge Gary Markwell, had died the year before after taking a single 5-FU dose at age 77.
“I was like … that’s exactly what happened to my brother.”
Murray senses momentum toward mandatory testing. In 2022, the Oregon Health & Science University paid $1 million to settle a suit after an overdose death.
“What’s going to break that barrier is the lawsuits, and the big institutions like Dana-Farber who are implementing programs and seeing them succeed,” she said. “I think providers are going to feel kind of bullied into a corner. They’re going to continue to hear from families and they are going to have to do something about it.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: