Ideal Blood Pressure Numbers Explained
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Maybe I missed it but the study on blood pressure did it say what the 2 numbers should read ideally?❞
We linked it at the top of the article rather than including it inline, as we were short on space (and there was a chart rather than a “these two numbers” quick answer), but we have a little more space today, so:
| Category | Systolic (mm Hg) | Diastolic (mm Hg) | |
| Normal | < 120 | AND | < 80 |
| Elevated | 120 – 129 | AND | < 80 |
| Stage 1 – High Blood Pressure | 130 – 139 | OR | 80 – 89 |
| Stage 2 – High Blood Pressure | 140 or higher | OR | 90 or higher |
| Hypertensive Crisis | Above 180 | AND/OR | Above 120 |
To oversimplify for a “these two numbers” answer, under 120/80 is generally considered good, unless it is under 90/60, in which case that becomes hypotension.
Hypotension, the blood pressure being too low, means your organs may not get enough oxygen and if they don’t, they will start shutting down.
To give you an idea how serious this, this is the closed-circuit equivalent of the hypovolemic shock that occurs when someone is bleeding out onto the floor. Technically, bleeding to death also results in low blood pressure, of course, hence the similarity.
So: just a little under 120/80 is great.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Healthy Hormones And How To Hack Them
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Healthy Hormones And How To Hack Them!
Hormones are vital for far more than they tend to get credit for. Even the hormones that people think of first—testosterone and estrogen—do a lot more than just build/maintain sexual characteristics and sexual function. Without them, we’d lack energy, we’d be depressed, and we’d soon miss the general smooth-running of our bodies that we take for granted.
And that’s without getting to the many less-talked-about hormones that play a secondary sexual role or are in the same general system…
How are your prolactin levels, for example?
Unless you’re ill, taking certain medications, recently gave birth, or picked a really interesting time to read this newsletter, they’re probably normal, by the way.
But, prolactin can explain “la petite mort”, the downturn in energy and the somewhat depressed mood that many men experience after orgasm.
Otherwise, if you have too much prolactin in general, you will be sleepy and depressed.
Prolactin’s primary role? In women, it stimulates milk production when needed. In men, it plays a role in regulating mood and metabolism.
Share This Post

An apple cider vinegar drink a day? New study shows it might help weight loss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Made from fermented apples and naturally high in acetic acid, apple cider vinegar has been popular in recent years for its purported health benefits – from antibacterial properties to antioxidant effects and potential for helping manage blood sugars.
Its origins as a health tonic stretch much further back. Hippocrates used it to treat wounds, fever and skin sores.
An experimental study, released today, looks into whether apple cider vinegar could be effective for weight loss, reduce blood glucose levels and reduce blood lipids (cholesterol and triglycerides).
The results suggest it could reduce all three – but it might not be as simple as downing an apple cider vinegar drink a day.
What did they do?
A group of scientists in Lebanon did a double-blinded, randomised, clinical trial in a group of overweight and obese young people aged from 12–25 years.
Researchers randomly placed 30 participants in one of four groups. The participants were instructed to consume either 5, 10 or 15ml of apple cider vinegar diluted into 250ml of water each morning before they ate anything for 12 weeks. A control group consumed an inactive drink (a placebo) made (from lactic acid added to water) to look and taste the same.
Typically this sort of study provides high quality evidence as it can show cause and effect – that is the intervention (apple cider vinegar in this case) leads to a certain outcome. The study was also double-blinded, which means neither the participants or the scientists involved with collecting the data knew who was in which group.
So, what did they find?
After a period of three months apple cider vinegar consumption was linked with significant falls in body weight and body mass index (BMI). On average, those who drank apple cider vinegar during that period lost 6–8kg in weight and reduced their BMI by 2.7–3 points, depending on the dose. They also showed significant decreases in the waist and hip circumference.
The authors also report significant decreases in levels of blood glucose, triglycerides, and cholesterol in the apple cider groups. This finding echoes previous studies. The placebo group, who were given water with lactic acid, had much smaller decreases in weight and BMI. There were also no significant decreases in blood glucose and blood lipids.
From animal studies, it is thought the acetic acid in apple cider vinegar may affect the expression of genes involved in burning fats for energy. The new study did not explore whether this mechanism was involved in any weight loss.
Is this good news?
While the study appears promising, there are also reasons for caution.
Firstly, study participants were aged from 12 to 25, so we can’t say whether the results could apply to everyone.
The statistical methods used in the study don’t allow us to confidently say the same amount of weight loss would occur again if the study was done again.
And while the researchers kept records of the participants’ diet and exercise during the study, these were not published in the paper. This makes it difficult to determine if diet or exercise may have had an impact. We don’t know whether participants changed the amount they ate or the types of food they ate, or whether they changed their exercise levels.
The study used a placebo which they tried to make identical in appearance and taste to the active treatment. But people may still be able to determine differences. Researchers may ask participants at the end of a study to guess which group they were in to test the integrity of the placebo. Unfortunately this was not done in this study, so we can’t be certain if the participants knew or not.
Finally, the authors do not report whether anyone dropped out of the study. This could be important and influence results if people who did not lose weight quit due to lack of motivation.

Is that you mother? The enzymes in apple cider vinegar might be health-giving.
ShutterstockAny other concerns?
Apple cider vinegar is acidic and there are concerns it may erode tooth enamel. This can be a problem with any acidic beverages, including fizzy drinks, lemon water and orange juice.
To minimise the risk of acid erosion some dentists recommend the following after drinking acidic drinks:
- rinsing out your mouth with tap water afterwards
- chewing sugar-free gum afterwards to stimulate saliva production
- avoiding brushing your teeth immediately after drinking because it might damage the teeth’s softened top layer
- drink with a straw to minimise contact with the teeth.

Rinsing with water could prevent acid damaging your teeth.
ShutterstockDown the hatch?
This study provides us with some evidence of a link between apple cider vinegar and weight loss. But before health professionals can recommend this as a weight loss strategy we need bigger and better conducted studies across a wider age range.
Such research would need to be done alongside a controlled background diet and exercise across all the participants. This would provide more robust evidence that apple cider vinegar could be a useful aid for weight loss.
Still, if you don’t mind the taste of apple cider vinegar then you could try drinking some for weight loss, alongside a healthy balanced and varied dietary intake. This study does not suggest people can eat whatever they like and drink apple cider vinegar as a way to control weight.

Evangeline Mantzioris, Program Director of Nutrition and Food Sciences, Accredited Practising Dietitian, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post

Brown Rice Protein: Strengths & Weaknesses
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I had a friend mention that recent research showed Brown Rice Protein Powder can be bad for you, possibly impacting your nutrient absorption. Is this true? I’ve been using it given it’s one of the few plant-based proteins with a full essential amino acid profile!❞
Firstly: we couldn’t find anything to corroborate the “brown rice protein powder [adversely] impacts nutrient absorption” idea, but we suspect that the reason for this belief is: brown rice (not brown rice protein powder) contains phytic acid, which is something of an antinutrient, in that it indeed reduces absorption of various other nutrients.
However, two things are important to note here:
- the phytic acid is found in whole grains, not in protein isolates as found in brown rice protein powder. The protein isolates contain protein… Isolated. No phytates!
- even in the case of eating whole grain rice, the phytic acid content is greatly reduced by two things: soaking and heating (especially if those two things are combined) ← doing this the way described results in bioavailability of nutrients that’s even better than if there were just no phytic acid, albeit it requires you having the time to soak, and do so at temperature.
tl;dr = no, it’s not true, unless there truly is some groundbreaking new research we couldn’t find—it was almost certainly a case of an understandable confusion about phytic acid.
Your question does give us one other thing to mention though:
Brown rice indeed technically contains all 9 essential amino acids, but it’s very low in several of them, most notably lysine.
However, if you use our Tasty Versatile Rice Recipe, the chia seeds we added to the rice have 100x the lysine that brown rice does, and the black pepper also boosts nutrient absorption.
Because your brown rice protein powder is a rice protein powder and not simply rice, it’s possible that they’ve tweaked it to overcome rice’s amino acid deficiencies. But, if you’re looking for a plant-based protein powder that is definitely a complete protein, soy is a very good option assuming you’re not allergic to that:
Amino Acid Compositions Of Soy Protein Isolate
If you’re wondering where to get it, you can see examples of them next to each other on Amazon here:
Brown Rice Protein Powder | Soy Protein Isolate Powder
Enjoy!
Share This Post
Related Posts

In the Realm of Hungry Ghosts – by Dr. Gabor Maté
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books by Dr. Maté before, and this one’s about addiction. We’ve reviewed books about addiction before too, so what makes this one different?
Wow, is this one so different. Most books about addiction are about “beating” it. Stop drinking, quit sugar, etc. And, that’s all well and good. It is definitely good to do those things. But this one’s about understanding it, deeply. Because, as Dr. Maté makes very clear, “there, but for the grace of epigenetics and environmental factors, go we”.
Indeed, most of us will have addictions; they’re (happily) just not too problematic for most of us, being either substances that are not too harmful (e.g. coffee), or behavioral addictions that aren’t terribly impacting our lives (e.g. Dr. Maté’s compulsion to keep buying more classical music, which he then tries to hide from his wife).
The book does also cover a lot of much more serious addictions, the kind that have ruined lives, and the kind that definitely didn’t need to, if people had been given the right kind of help—instead of, all too often, they got the opposite.
Perhaps the greatest value of this book is that; understanding what creates addiction in the first place, what maintains it, and what help people actually need.
Bottom line: if you’d like more insight into the human aspect of addiction without getting remotely wishy-washy, this book is probably the best one out there.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Feel-Good Productivity – by Dr. Ali Abdaal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Rise and grind” is not a sustainable way to live. Yet for most of us, there are things we do have to do every day that we don’t necessarily do for fun. So, how to be productive with those things, and not feel like we are constantly compromising and sacrificing our time on this earth for some intrinsically trivial but extrinsically required activity that’ll be forgotten tomorrow?
And most of us do also have dreams and ambitions (and if you don’t, then what were they before life snatched them away from you?), things to work towards. So there is “carrot” for us as well as “stick”. But how to break the cycle and get more carrot and less stick, while being more productive than before?
Dr. Abdaal frames this principally in terms of neurology first, psychology next.
That when we are bored, we simply do not have the neurochemicals required to work well anyway, so addressing that first needs to be a priority. He lays out many ways of doing this, gives lots of practical tips, and brings attention to the ways it’s easy to go wrong (and how to fix those too).
The writing style isdeceptively relaxed and casual, leading the reader smoothly into understanding of each topic before moving on.
Bottom line: if you want to get more done while feeling better about it (not a tired wreck), then this is the book for you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

10almonds Tells The Tea…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s Bust Some Myths!
It’s too late after puberty, hormones won’t change xyz
While yes, many adult trans people dearly wish they’d been able to medically transition before going through the “wrong” puberty, the truth is that a lot of changes will still occur later… even to “unchangeable” things like the skeleton.
The body is remaking itself throughout life, and hormones tell it how to do that. Some parts are just quicker or slower than others. Also: the skeleton is pulled-on constantly by our muscles, and in a battle of muscle vs bone, muscle will always win over time.
Examples of this include:
- trans men building bigger bones to support their bigger muscles
- trans women getting smaller, with wider hips and a pelvic tilt
Trans people have sporting advantages
Assuming at least a year’s cross-sex hormonal treatment, there is no useful advantage to being trans when engaging in a sport. There are small advantages and disadvantages (which goes for any person’s body, really). For example:
- Trans women will tend to be taller than cis women on average…
- …but that larger frame is now being powered by smaller muscles, because they shrink much quicker than the skeleton.
- Trans men taking T are the only athletes allowed to take testosterone…
- …but they will still often be smaller than their fellow male competitors, for example.
Read: Do Trans Women Athletes Have Advantages? (A rather balanced expert overview, which does also cover trans men)
There’s a trans population explosion; it’s a social contagion epidemic!

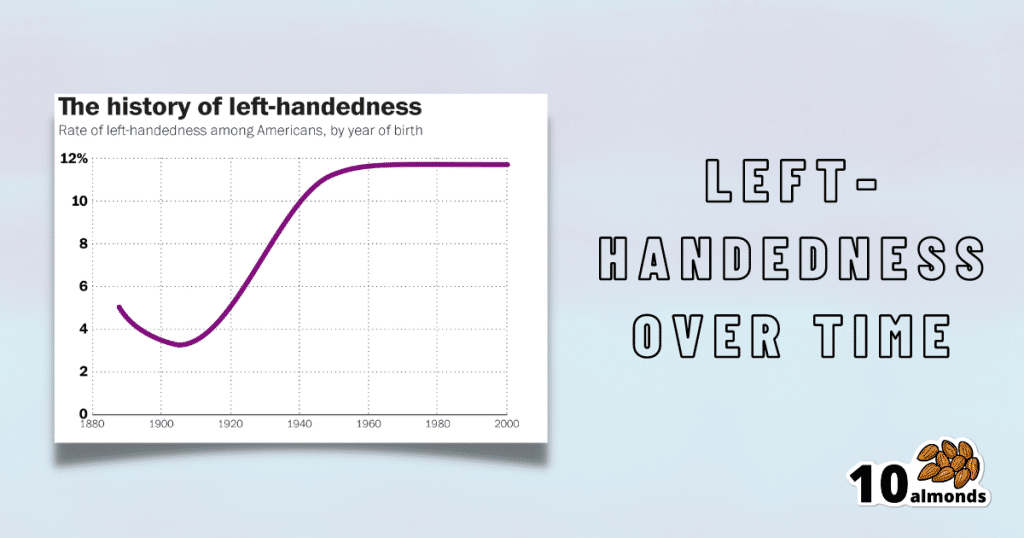
Source for figures: The Overall Rate Of Left-Handedness (Researchgate)
Left-handed people used to make up around 3% of the population… Until the 1920s, when that figure jumped sharply upwards, before plateauing at around 12% in around 1960, where it’s stayed since. What happened?! Simple, schools stopped forcing children to use their right hand.
Today, people ask for trans healthcare because they know it exists! Decades ago, it wasn’t such common knowledge.
The same explanation can be applied to other “population explosions” such as for autism and ADHD.
Fun fact: Mt. Everest was “discovered” in 1852, but scientists suspect it probably existed long before then! People whose ancestors were living on it long before 1852 also agree. Sometimes something exists for a long time, and only comes to wider public awareness later.
Transgender healthcare is too readily available, especially to children!
To believe some press outlets, you’d think:
- HRT is available from school vending machines,
- kids can get a walk-in top surgery at recess,
- and there’s an after-school sterilization club.
In reality, while availability varies from place to place, trans healthcare is heavily gatekept. Even adults have trouble getting it, often having to wait years and/or pay large sums of money… and get permission from a flock of doctors, psychologists, and the like. For those under the age of 18, it’s almost impossible in many places, even with parental support.
Puberty-blockers shouldn’t be given to teenagers, as the effects are irreversible
Quick question: who do you think should be given puberty-blockers? For whom do you think they were developed? Not adults, for sure! They were not developed for trans teens either, but for cis pre-teens with precocious puberty, to keep puberty at bay, to do it correctly later. Nobody argues they’re unsafe for much younger cis children, and only object when it’s trans teens.
They’re not only safe and reversible, but also self-reversing. Stop taking them, and the normally scheduled puberty promptly ensues by itself. For trans kids, the desired effect is to buy the kid time to make an informed and well-considered decision. After all, the effects of the wrong puberty are really difficult to undo!
A lot of people rush medical transition and regret it!
Trans people wish it could be rushed! It’s a lot harder to get gender-affirming care as a trans person, than it is to get the same (or comparable) care as a cis person. Yes, cis people get gender-affirming care, from hormones to surgeries, and have done for a long time.
As for regret… Medical transition has around a 1% regret rate. For comparison, hip replacement has a 4.8% regret rate and knee replacement has a 17.1% regret rate.
A medical procedure with a 99% success rate would generally be considered a miracle cure!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: