Spinach vs Chard – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing spinach to chard, we picked the spinach.
Why?
In terms of macros, spinach has slightly more fiber and protein, while chard has slightly more carbs. Now, those carbs are fine; nobody is getting metabolic disease from eating greens. But, by the numbers, this is a clear, albeit marginal, win for spinach.
In the category of vitamins, spinach has more of vitamins A, B1, B2, B3, B5, B6, B9, E, and K, while chard has more of vitamins C and choline. An even clearer victory for spinach this time.
When it comes to minerals, spinach has more calcium, copper, iron, magnesium, manganese, phosphorus, selenium, and zinc, while chard has more potassium. Once again, a clear win for spinach.
You may be wondering about oxalates, in which spinach is famously high. However, chard is nearly 2x higher in oxalates. In practical terms, this doesn’t mean too much for most people. If you have kidney problems or a family history of such, it is recommended to avoid oxalates. For everyone else, the only downside is that oxalates diminish calcium bioavailability, which is a pity, as spinach is (by the numbers) a good source of calcium.
However, oxalates are broken down by heat, so this means that cooked spinach (lightly steamed is fine; you don’t need to do anything drastic) will be much lower in oxalates (if you have kidney problems, do still check with your doctor/dietician, though).
All in all, spinach beats chard by most metrics, and by a fair margin. Still, enjoy either or both, unless you have kidney problems, in which case maybe go for kale or collard greens instead!
Want to learn more?
You might like to read:
Make Your Vegetables Work Better Nutritionally ← includes a note on breaking down oxalates, and lots of other information besides!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ice Cream vs Fruit Sorbet – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing ice cream to fruit sorbet, we picked the ice cream.
Why?
Well, neither are great!
But the deciding factor is simple: ice cream has more nutrients to go with its sugar.
While “fruit is good” is a very reliable truism in and of itself, sorbet tends to be made with fruit juice (or at best, purée, which for these purposes is more or less the same) and sugar. The small vitamin content is nowhere near enough to make up for this. The fiber having been removed by juicing or puréeing, the fruit juice with added sugar is basically shooting glucose and fructose into your veins while doing little else.
Fruit juice (even freshly-pressed) is nowhere near in the same league of healthiness as actual fruit!
See also: Which Sugars Are Healthier, And Which Are Just The Same?
Ice cream, meanwhile, is also not exactly a health food. But it has at least some minerals worth speaking of (mostly: calcium, potassium, phosphorus), and some fat that a) can be used b) helps slightly slow the absorption of the sugars.
In short: please do not consider either of these things to be a health food. But if you’re going to choose one or the other (and are not lactose-intolerant), then ice cream has some small positives to go with its negatives.
Take care!
Share This Post
-
Never Too Old?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Age Limits On Exercise?
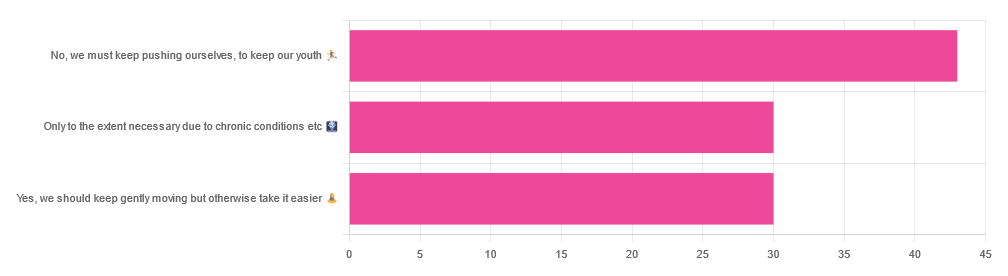
In Tuesday’s newsletter, we asked you your opinion on whether we should exercise less as we get older, and got the above-depicted, below-described, set of responses:
- About 42% said “No, we must keep pushing ourselves, to keep our youth“
- About 29% said “Only to the extent necessary due to chronic conditions etc”
- About 29% said “Yes, we should keep gently moving but otherwise take it easier”
One subscriber who voted for “No, we must keep pushing ourselves, to keep our youth“ wrote to add:
❝I’m 71 and I push myself. I’m not as fast or strong as I used to be but, I feel great when I push myself instead of going through the motions. I listen to my body!❞
~ 10almonds subscriber
One subscriber who voted for “Only to the extent necessary due to chronic conditions etc” wrote to add:
❝It’s never too late to get stronger. Important to keep your strength and balance. I am a Silver Sneakers instructor and I see first hand how helpful regular exercise is for seniors.❞
~ 10almonds subscriber
One subscriber who voted to say “Yes, we should keep gently moving but otherwise take it easier” wrote to add:
❝Keep moving but be considerate and respectful of your aging body. It’s a time to find balance in life and not put yourself into a positon to damage youself by competing with decades younger folks (unless you want to) – it will take much longer to bounce back.❞
~ 10almonds subscriber
These will be important, because we’ll come back to them at the end.
So what does the science say?
Endurance exercise is for young people only: True or False?
False! With proper training, age is no barrier to serious endurance exercise.
Here’s a study that looked at marathon-runners of various ages, and found that…
- the majority of middle-aged and elderly athletes have training histories of less than seven years of running
- there are virtually no relevant running time differences (p<0.01) per age in marathon finishers from 20 to 55 years
- after 55 years, running times did increase on average, but not consistently (i.e. there were still older runners with comparable times to the younger age bracket)
The researchers took this as evidence of aging being indeed a biological process that can be sped up or slowed down by various lifestyle factors.
See also:
Age & Aging: What Can (And Can’t) We Do About It?
this covers the many aspects of biological aging (it’s not one number, but many!) and how our various different biological ages are often not in sync with each other, and how we can optimize each of them that can be optimized
Resistance training is for young people only: True or False?
False! In fact, it’s not only possible for older people, but is also associated with a reduction in all-cause mortality.
Specifically, those who reported strength-training at least once per week enjoyed longer lives than those who did not.
You may be thinking “is this just the horse-riding thing again, where correlation is not causation and it’s just that healthier people (for other reasons) were able to do strength-training more, rather than the other way around?“
…which is a good think to think of, so well-spotted if you were thinking that!
But in this case no; the benefits remained when other things were controlled for:
❝Adjusted for demographic variables, health behaviors and health conditions, a statistically significant effect on mortality remained.
Although the effects on cardiac and cancer mortality were no longer statistically significant, the data still pointed to a benefit.
Importantly, after the physical activity level was controlled for, people who reported strength exercises appeared to see a greater mortality benefit than those who reported physical activity alone.❞
See the study: Is strength training associated with mortality benefits? A 15 year cohort study of US older adults
And a pop-sci article about it: Strength training helps older adults live longer
Closing thoughts
As it happens… All three of the subscribers we quoted all had excellent points!
Because in this case it’s less a matter of “should”, and more a selection of options:
- We (most of us, at least) can gain/regain/maintain the kind of strength and fitness associated with much younger people, and we need not be afraid of exercising accordingly (assuming having worked up to such, not just going straight from couch to marathon, say).
- We must nevertheless be mindful of chronic conditions or even passing illnesses/injuries, but that goes for people of any age
- We also can’t argue against a “safety first” cautious approach to exercise. After all, sure, maybe we can run marathons at any age, but that doesn’t mean we have to. And sure, maybe we can train to lift heavy weights, but if we’re content to be able to carry the groceries or perhaps take our partner’s weight in the dance hall (or the bedroom!), then (if we’re also at least maintaining our bones and muscles at a healthy level) that’s good enough already.
Which prompts the question, what do you want to be able to do, now and years from now? What’s important to you?
For inspiration, check out: Train For The Event Of Your Life!
Take care!
Share This Post
-
The Inflammation Spectrum – by Dr. Will Cole
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Cole’s other book “Gut Feelings”, and now he’s back, this time to tackle inflammation.
The focus here is on understanding what things trigger inflammation in your body—personally yours, not someone else’s—by something close to the usual elimination process yes, but he offers a way of sliding into it gently instead of simply quitting all the things and gradually adding everything back in.
The next step he takes the reader through is eating not just to avoid triggering inflammation, but to actively combat it. From there, it should be possible for the reader to build an anti-inflammatory cookbook, that’s not only one’s own personal repertoire of cooking, but also specifically tailored to one’s own personal responses to different ingredients.
The style of this book is very pop-science, helpful, walking-the-reader-by-the-hand through the processes involved. Dr. Cole wants to make everything as easy as possible.
Bottom line: if your diet could use an anti-inflammatory revamp, this is a top-tier guidebook for doing just that.
Click here to check out The Inflammation Spectrum, find your food triggers and reset your system!
Share This Post
Related Posts
-
HRT Side Effects & Troubleshooting
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Heather Hirsch. She’s a board-certified internist, and her clinical expertise focuses on women’s health, particularly in midlife and menopause, and its intersection with chronic diseases (ranging from things associated with sexual health, to things like osteoporosis and heart disease).
So, what does she want us to know?
HRT can be life-changingly positive, but it can be a shaky start
Hormone Replacement Therapy (HRT), and in this context she’s talking specifically about the most common kind, Menopausal Hormone Therapy (MHT), involves taking hormones that our body isn’t producing enough of.
If these are “bioidentical hormones” as used in most of the industrialized world and increasingly also in N. America, then this is by definition a supplement rather than a drug, for what it’s worth, whereas some non-bioidentical hormones (or hormone analogs, which by definition function similarly to hormones but aren’t the same thing) can function more like drugs.
We wrote a little about his previously:
Hormone Replacement Therapy: A Tale Of Two Approaches
For most people most of the time, bioidentical hormones are very much the best way to go, as they are not only more effective, but also have fewer side effects.
That said, even bioidentical hormones can have some undesired effects, so, how to deal with those?
Don’t worry; bleed happy
A reprise of (usually quite light) menstrual bleeding is the most common side effect of menopausal HRT.
This happens because estrogen affects* the uterus, leading to a build-up and shedding of the uterine lining.
*if you do not have a uterus, estrogen can effect uterine tissue. That’s not a typo—here we mean the verb “effect”, as in “cause to be”. It will not grow a new uterus, but it can cause some clumps of uterine tissue to appear; this means that it becomes possible to get endometriosis without having a uterus. This information should not be too shocking, as endometriosis is a matter of uterine tissue growing inconveniently, often in places where it shouldn’t, and sometimes quite far from the uterus (if present, or its usual location, if absent). However, the risk of this happening is far lower than if you actually have a uterus:
What you need to know about endometriosis
Back to “you have a uterus and it’s making you wish you didn’t”:
This bleeding should, however, be light. It’ll probably be oriented around a 28-day cycle even if you are taking your hormones at the same dose every day of the month, and the bleeding will probably taper off after about 6 months of this.
If the bleeding is heavier, all the time, or persists longer than 6 months, then speak to your gynecologist about it. Any of those three; it doesn’t have to be all three!
Bleeding outside of one’s normal cycle can be caused by anything from fibroids to cancer; statistically speaking it’s probably nothing too dire,but when your safety is in question, don’t bet on “probably”, and do get it checked out:
When A Period Is Very Late (i.e., Post-Menopause)
Dr. Hirsch recommends, as possible remedies to try (preferably under your gynecologist’s supervision):
- lowering your estrogen dose
- increasing your progesterone dose
- taking progesterone continuously instead of cyclically
And if you’re not taking progesterone, here’s why you might want to consider taking this important hormone that works with estrogen to do good things, and against estrogen to rein in some of estrogen’s less convenient things:
Progesterone Menopausal HRT: When, Why, And How To Benefit
(the above link contains, as well as textual information, an explanatory video from Dr. Hirsch herself)
Get the best of the breast
Calm your tits. Soothe your boobs. Destress your breasts. Hakuna your tatas. Undo the calamity beleaguering your mammaries.
Ok, more seriously…
Breast tenderness is another very common symptom when starting to take estrogen. It can worry a lot of people (à la “aagh, what is this and is it cancer!?”), but is usually nothing to worry about. But just to be sure, do also check out:
Keeping Abreast Of Your Cancer Risk: How To Triple Your Breast Cancer Survival Chances
Estrogen can cause feelings of breast fullness, soreness, nipple irritation, and sometimes lactation, but this later will be minimal—we’re talking a drop or two now and again, not anything that would feed a baby.
Basically, it happens when your body hasn’t been so accustomed to normal estrogen levels in a while, and suddenly wakes up with a jolt, saying to itself “Wait what are we doing puberty again now? I thought we did menopause? Are we pregnant? What’s going on? Ok, checking all systems!” and then may calm down not too long afterwards when it notes that everything is more or less as it should be already.
If this persists or is more than a minor inconvenience though, Dr. Hirsch recommends looking at the likely remedies of:
- Adjust estrogen (usually the cause)
- Adjust progesterone (less common)
- If it’s progesterone, changing the route of administration can ameliorate things
What if it’s not working? Is it just me?
Dr. Hirsch advises the most common reasons are simply:
- wrong formulation (e.g. animal-derived estrogen or hormone analog, instead of bioidentical)
- wrong dose (e.g. too low)
- wrong route of administration (e.g. oral vs transdermal; usually transdermal estradiol is most effective but many people do fine on oral; progesterone meanwhile is usually best as a pessary/suppository, but many people do fine on oral)
Writer’s example: in 2022 there was an estrogen shortage in my country, and while I had been on transdermal estradiol hemihydrate gel, I had to go onto oral estradiol valerate tablets for a few months, because that’s what was available. And the tablets simply did not work for me at all. I felt terrible and I have a good enough intuitive sense of my hormones to know when “something wrong is not right”, and a good enough knowledge of the pharmacology & physiology to know what’s probably happening (or not happening). And sure enough, when I got my blood test results, it was as though I’d been taking nothing. It was such a relief to get back on the gel once it became available again!
So, if something doesn’t seem to be working for you, speak up and get it fixed if at all possible.
See also: What You Should Have Been Told About Menopause Beforehand
Want to know more from Dr. Hirsch?
You might like this book of hers, which we haven’t reviewed yet, but present here for your interest:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How the stress of playing chess can be fatal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The death of a chess player in the middle of a match at the world’s most prestigious competition may have shocked those who view the game as a relaxing pastime. Kurt Meier, 67, collapsed during his final match in the tournament and died in hospital later that day. But chess, like any other game or sport, can lead to an immense amount of stress, which can be bad for a competitor’s physical health too.
We tend to associate playing sport or games with good health and well-being. And there are a countless number of studies showing playing games has an association with feeling happier. While this argument is true for recreational players, the story can be different for the elite, where success and failure are won and lost by the finest margins and where winning can mean funding and a future, and losing can mean poverty and unemployment. If this is the case, can being successful at a sport or game actually be bad for you?
Competitive anxiety
Elite competition can be stressful because the outcome is so important to the competitors. We can measure stress using a whole range of physiological indicators such as heart rate and temperature, and responses such as changes in the intensity of our emotions.
Emotions provide a warning of threat. So if you feel that achieving your goal is going to be difficult, then expect to feel intense emotions. The leading candidate that signals we are experiencing stress is anxiety, characterised by thoughts of worry, fears of dread about performance, along with accompanying physiological responses such as increased heart rate and sweaty palms. If these symptoms are experienced regularly or chronically, then this is clearly detrimental to health.
This stress response is probably not restricted to elite athletes. Intense emotions are linked to trying to achieve important goals and while it isn’t the only situation where it occurs, it is just very noticeable in sport.
The causes of stress
It makes more sense to focus on what the causes of stress are rather than where we experience it. The principle is that the more important the goal is to achieve, then the greater the propensity for the situation to intensify emotions.
Emotions intensify also by the degree of uncertainty and competing, at whatever level of a sport, is uncertain when the opposition is trying its hardest to win the contest and also has a motivation to succeed. The key point is that almost all athletes at any level can suffer bouts of stress, partly due to high levels of motivation.
A stress response is also linked to how performance is judged and reported. Potentially stressful tasks tend to be ones where performance is public and feedback is immediate. In chess – as with most sporting contests – we see who the winner is and can start celebrating success or commiserating failure as soon as the game is over.
There are many tasks which have similar features. Giving a speech in public, taking an academic examination, or taking your driving test are all examples of tasks that can illicit stress. Stress is not restricted to formal tasks but can also include social tasks. Asking a potential partner for a date, hand in marriage, and meeting the in-laws for the first time can be equally stressful.
Winning a contest or going on a date relate to higher-order goals about how we see ourselves. If we define ourselves as “being a good player” or “being attractive or likeable” then contrasting information is likely to associate with unpleasant emotions. You will feel devastated if you are turned down when asking someone out on a date, for instance, and if this was repeated, it could lead to reduced self-esteem and depression.
The key message here is to recognise what your goals are and think about how important they are. If you want to achieve them with a passion and if the act of achieving them leads to intense and sometimes unwanted emotions, then it’s worth thinking about doing some work to manage these emotions.
Andrew Lane, Professor in Sport and Learning, University of Wolverhampton
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Keep Inflammation At Bay
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How to Prevent (or Reduce) Inflammation
You asked us to do a main feature on inflammation, so here we go!
Before we start, it’s worth noting an important difference between acute and chronic inflammation:
- Acute inflammation is generally when the body detects some invader, and goes to war against it. This (except in cases such as allergic responses) is usually helpful.
- Chronic inflammation is generally when the body does a civil war. This is almost never helpful.
We’ll be tackling the latter, which frees up your body’s resources to do better at the former.
First, the obvious…
These five things are as important for this as they are for most things:
- Get a good diet—the Mediterranean diet is once again a top-scorer
- Exercise—move and stretch your body; don’t overdo it, but do what you reasonably can, or the inflammation will get worse.
- Reduce (or ideally eliminate) alcohol consumption. When in pain, it’s easy to turn to the bottle, and say “isn’t this one of red wine’s benefits?” (it isn’t, functionally*). Alcohol will cause your inflammation to flare up like little else.
- Don’t smoke—it’s bad for everything, and that goes for inflammation too.
- Get good sleep. Obviously this can be difficult with chronic pain, but do take your sleep seriously. For example, invest in a good mattress, nice bedding, a good bedtime routine, etc.
*Resveratrol (which is a polyphenol, by the way), famously found in red wine, does have anti-inflammatory properties. However, to get enough resveratrol to be of benefit would require drinking far more wine than will be good for your inflammation or, indeed, the rest of you. So if you’d like resveratrol benefits, consider taking it as a supplement. Superficially it doesn’t seem as much fun as drinking red wine, but we assure you that the results will be much more fun than the inflammation flare-up after drinking.
About the Mediterranean Diet for this…
There are many causes of chronic inflammation, but here are some studies done with some of the most common ones:
- Beneficial effect of Mediterranean diet in systemic lupus erythematosus patients
- How the Mediterranean diet and some of its components modulate inflammatory pathways in arthritis
- The effects of the Mediterranean diet on biomarkers of vascular wall inflammation and plaque vulnerability in subjects with high risk for cardiovascular disease
- Adherence to Mediterranean diet and 10-year incidence of diabetes: correlations with inflammatory and oxidative stress biomarkers*
*Type 1 diabetes is a congenital autoimmune disorder, as the pancreas goes to war with itself. Type 2 diabetes is different, being a) acquired and b) primarily about insulin resistance, and/but this is related to chronic inflammation regardless. It is also possible to have T1D and go on to develop insulin resistance, and that’s very bad, and/but beyond the scope of today’s newsletter, in which we are focusing on the inflammation aspects.
Some specific foods to eat or avoid…
Eat these:
- Leafy greens
- Cruciferous vegetables
- Tomatoes
- Fruits in general (berries in particular)
- Healthy fats, e.g. olives and olive oil
- Almonds and other nuts
- Dark chocolate (choose high cocoa, low sugar)
Avoid these:
- Processed meats (absolute worst offenders are hot dogs, followed by sausages in general)
- Red meats
- Sugar (includes most fruit juices, but not most actual fruits—the difference with actual fruits is they still contain plenty of fiber, and in many cases, antioxidants/polyphenols that reduce inflammation)
- Dairy products (unless fermented, in which case it seems to be at worst neutral, sometimes even a benefit, in moderation)
- White flour (and white flour products, e.g. white bread, white pasta, etc)
- Processed vegetable oils
See also: 9 Best Drinks To Reduce Inflammation, Says Science
Supplements?
Some supplements that have been found to reduce inflammation include:
(links are to studies showing their efficacy)
Consider Intermittent Fasting
Remember when we talked about the difference between acute and chronic inflammation? It’s fair to wonder “if I reduce my inflammatory response, will I be weakening my immune system?”, and the answer is: generally, no.
Often, as with the above supplements and dietary considerations, reducing inflammation actually results in a better immune response when it’s actually needed! This is because your immune system works better when it hasn’t been working in overdrive constantly.
Here’s another good example: intermittent fasting reduces the number of circulating monocytes (a way of measuring inflammation) in healthy humans—but doesn‘t compromise antimicrobial (e.g. against bacteria and viruses) immune response.
See for yourself: Dietary Intake Regulates the Circulating Inflammatory Monocyte Pool ← the study is about the anti-inflammatory effects of fasting
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: