Why 7 Hours Sleep Is Not Enough
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Sleep-Deprived Are You, Really?
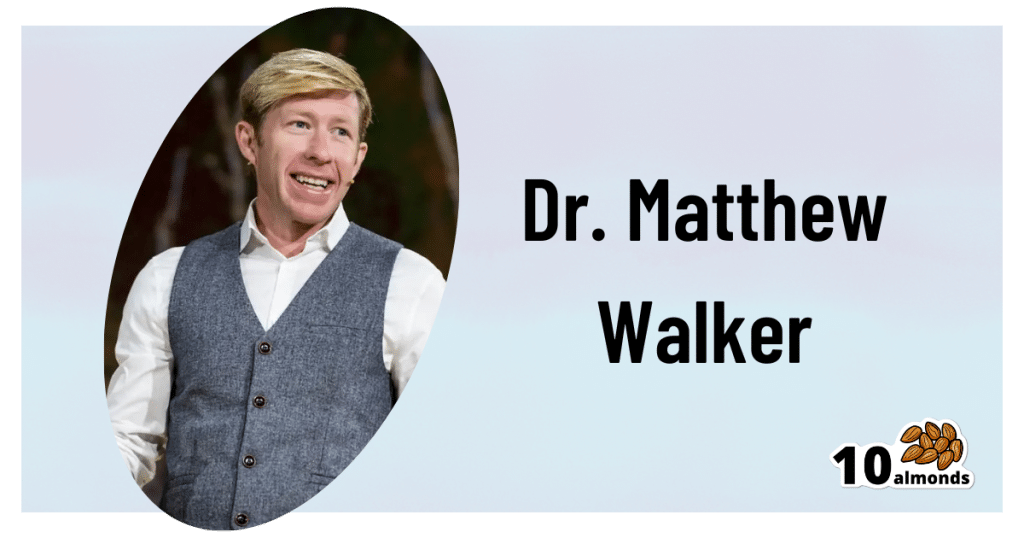
This is Dr. Matthew Walker. He’s a neuroscientist and sleep specialist, and is the Director of the Center for Human Sleep Science at UC Berkeley’s Department of Psychology. He’s also the author of the international bestseller “Why We Sleep”.
What does he want us to know?
Sleep deprivation is more serious than many people think it is. After about 16 hours without sleep, the brain begins to fail, and needs more than 7 hours of sleep to “reset” cognitive performance.
Note: note “seven or more”, but “more than seven”.
After ten days with only 7 hours sleep (per day), Dr. Walker points out, the brain is as dysfunctional as it would be after going without sleep for 24 hours.
Here’s the study that sparked a lot of Dr. Walker’s work:
Importantly, in Dr. Walker’s own words:
❝Three full nights of recovery sleep (i.e., more nights than a weekend) are insufficient to restore performance back to normal levels after a week of short sleeping❞
~ Dr. Matthew Walker
See also: Why You Probably Need More Sleep
Furthermore: the sleep-deprived mind is unaware of how sleep-deprived it is.
You know how a drunk person thinks they can drive safely? It’s like that.
You do not know how sleep-deprived you are, when you are sleep-deprived!
For example:
❝(60.7%) did not signal sleepiness before a sleep fragment occurred in at least one of the four MWT trials❞
Source: Sleepiness is not always perceived before falling asleep in healthy, sleep-deprived subjects
Sleep efficiency matters
With regard to the 7–9 hours band for optimal health, Dr. Walker points out that the sleep we’re getting is not always the sleep we think we’re getting:
❝Assuming you have a healthy sleep efficiency (85%), to sleep 9 hours in terms of duration (i.e. to be a long-sleeper), you would need to be consistently in bed for 10 hours and 36 minutes a night. ❞
~ Dr. Matthew Walker
At the bottom end of that, by the way, doing the same math: to get only the insufficient 7 hours sleep discussed earlier, a with a healthy 85% sleep efficiency, you’d need to be in bed for 8 hours and 14 minutes per night.
The unfortunate implication of this: if you are consistently in bed for 8 hours and 14 minutes (or under) per night, you are not getting enough sleep.
“But what if my sleep efficiency is higher than 85%?”
It shouldn’t be.If your sleep efficiency is higher than 85%, you are sleep-deprived and your body is having to enforce things.
Want to know what your sleep efficiency is?
We recommend knowing this, by the way, so you might want to check out:
Head-To-Head Comparison of Google and Apple’s Top Sleep-Monitoring Apps
(they will monitor your sleep and tell you your sleep efficiency, amongst other things)
Want to know more?
You might like his book:
Why We Sleep: Unlocking the Power of Sleep and Dreams
…and/or his podcast:
…and for those who like videos, here’s his (very informative) TED talk:
Prefer text? Click here to read the transcript
Want to watch it, but not right now? Bookmark it for later
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Blood-Sugar Balancing Beetroot Cutlets
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
These beetroot cutlets are meaty and proteinous and fibrous and even have a healthy collection of fats, making these much better for your heart and blood than an animal-based equivalent.
You will need
- 1 can kidney beans, drained and rinsed (or 1 cup same, cooked, drained, and rinsed)
- ½ cup chopped roasted or steamed beetroot, blotted dry
- ½ cup chopped walnuts (if allergic, substitute with ¼ cup pumpkin seeds)
- ½ cup cooked (ideally: mixed) grains of your choice (if you need gluten-free, there are plenty of gluten-free grains and pseudocereals)
- ¼ cup finely chopped onion
- ¼ bulb garlic, minced or crushed
- 2 tbsp nutritional yeast
- 2 tbsp ground flaxseeds
- 2 tbsp ground chia seeds
- 2 tsp tomato purée
- 1 tsp black pepper
- ½ tsp white miso paste
- ½ tsp smoked paprika
- ½ tsp cayenne pepper
- ¼ tsp MSG or ½ tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Combine the beetroot, beans, walnuts, grains, and onion in a food processor, and process until a coarse even mixture.
2) Add the remaining ingredients and process to mix thoroughly.
3) Transfer the mixture to a clean work surface and divide into six balls. If the structural integrity is not good (i.e. too soft), add a little more of any or all of these ingredients: chopped walnuts, ground flax, ground chia, nutritional yeast.
4) Press the balls firmly into cutlets, and refrigerate for at least 1 hour, but longer is even better if you have the time. Alternatively, if you’d like to freeze them for later use, then this is the point at which to do that.
5) Preheat the oven to 375℉ / 190℃.
6) Roast the cutlets on a baking tray lined with baking paper, for about 30 minutes, turning over carefully with a spatula halfway through. They should be firm when done; if they’re not, give them a little longer.
7) Serve hot, for example on a bed of greens and with a drizzle of aged balsamic vinegar.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Beetroot’s Many Benefits
- Our Top 5 Spices: How Much Is Enough For Benefits?
- What Omega-3 Fatty Acids Really Do For Us
- Three Daily Servings of Beans?
- If You’re Not Taking Chia, You’re Missing Out
Take care!
Share This Post
-
What’s Your Ikigai?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ikigai: A Closer Look
We’ve mentioned ikigai from time to time, usually when discussing the characteristics associated with Blue Zone centenarians, for example as number 5 of…
It’s about finding one’s “purpose”. Not merely a function, but what actually drives you in life. And, if Japanese studies can be extrapolated to the rest of the world, it has a significant and large impact on mortality (other factors being controlled for); not having a sense of ikigai is associated with an approximately 47%* increase in 7-year mortality risk in the categories of cardiovascular disease and external cause mortality:
Sense of life worth living (ikigai) and mortality in Japan: Ohsaki Study
*we did a lot of averaging and fuzzy math to get this figure; the link will show you the full stats though!
In case that huge (n=43,391) study didn’t convince you, here’s another comparably-sized (n=43,117) one that found similarly, albeit framing the numbers the other way around, i.e. a comparable decrease in mortality risk for having a sense of ikigai:
This study was even longer (12 years rather than 7), so the fact that it found pretty much the same results the 7-year study we cited just before is quite compelling evidence. Again, multivariate hazard ratios were adjusted for age, BMI, drinking and smoking status, physical activity, sleep duration, education, occupation, marital status, perceived mental stress, and medical history—so all these things were effectively controlled for statistically.
Three kinds of ikigai
There are three principal kinds of ikigai:
- Social ikigai: for example, a caring role in the family or community, volunteer work, teaching
- Asocial ikigai: for example, a solitary practice of self-discipline, spirituality, or study without any particular intent to teach others
- Antisocial ikigai: for example, a strong desire to outlive an enemy, or to harm a person or group that one hates
You may be thinking: wait, aren’t those last things bad?
And… Maybe! But ikigai is not a matter of morality or even about “warm fuzzy feelings”. The fact is, having a sense of purpose increases longevity regardless of moral implications or niceness.
Nevertheless, for obvious reasons there is a lot more focus on the first two categories (social and asocial), and of those, especially the first category (social), because on a social level, “we all do well when we all do well”.
We exemplified them above, but they can be defined:
- Social: working for the betterment of society
- Asocial: working for the betterment of oneself
Of course, for many people, the same ikigai may cover both of those—often somebody who excels at something for its own sake and/but shares it with others to enrich their lives also, for example a teacher, an artist, a scientist, etc.
For it to cover both, however, requires that both parts of it are genuinely part of their feeling of ikigai, and not merely unintended consequences.
For example, a piano teacher who loves music in general and the piano in particular, and would gladly spend every waking moment studying/practising/performing, but hates having to teach it, but needs to pay the bills so teaches it anyway, cannot be said to be living any kind of social ikigai there, just asocial. And in fact, if teaching the piano is causing them to not have the time or energy to pursue it for its own sake, they might not even be living any ikigai at all.
One other thing to watch out for
There is one last stumbling block, which is that while we can find ikigai, we can also lose it! Examples of this may include:
- A professional whose job is their ikigai, until they face mandatory retirement or are otherwise unable to continue their work (perhaps due to disability, for example)
- A parent whose full-time-parent role is their ikigai, until their children leave for school, university, life in general
- A married person whose “devoted spouse” role is their ikigai, until their partner dies
For this reason, people of any age can have a “crisis of identity” that’s actually more of a “crisis of purpose”.
There are two ways of handling this:
- Have a back-up ikigai ready! For example, if your profession is your ikigai, maybe you have a hobby waiting in the wings, that you can smoothly jump ship to upon retirement.
- Embrace the fluidity of life! Sometimes, things don’t happen the way we expect. Sometimes life’s surprises can trip us up; sometimes they can leave us a sobbing wreck. But so long as life continues, there is an opportunity to pick ourselves up and decide where to go from that point. Note that this is not fatalism, by the way, it doesn’t have to be “this bad thing happened so that we could find this good thing, so really it was a good thing all along”. Rather, it can equally readily be “well, we absolutely did not want that bad thing to happen, but since it did, now we shall take it this way from here”.
For more on developing/maintaining psychological resilience in the face of life’s less welcome adversities, see:
Psychological Resilience Training
…and:
Putting The Abs Into Absurdity ← do not underestimate the power of this one
Take care!
Share This Post
-
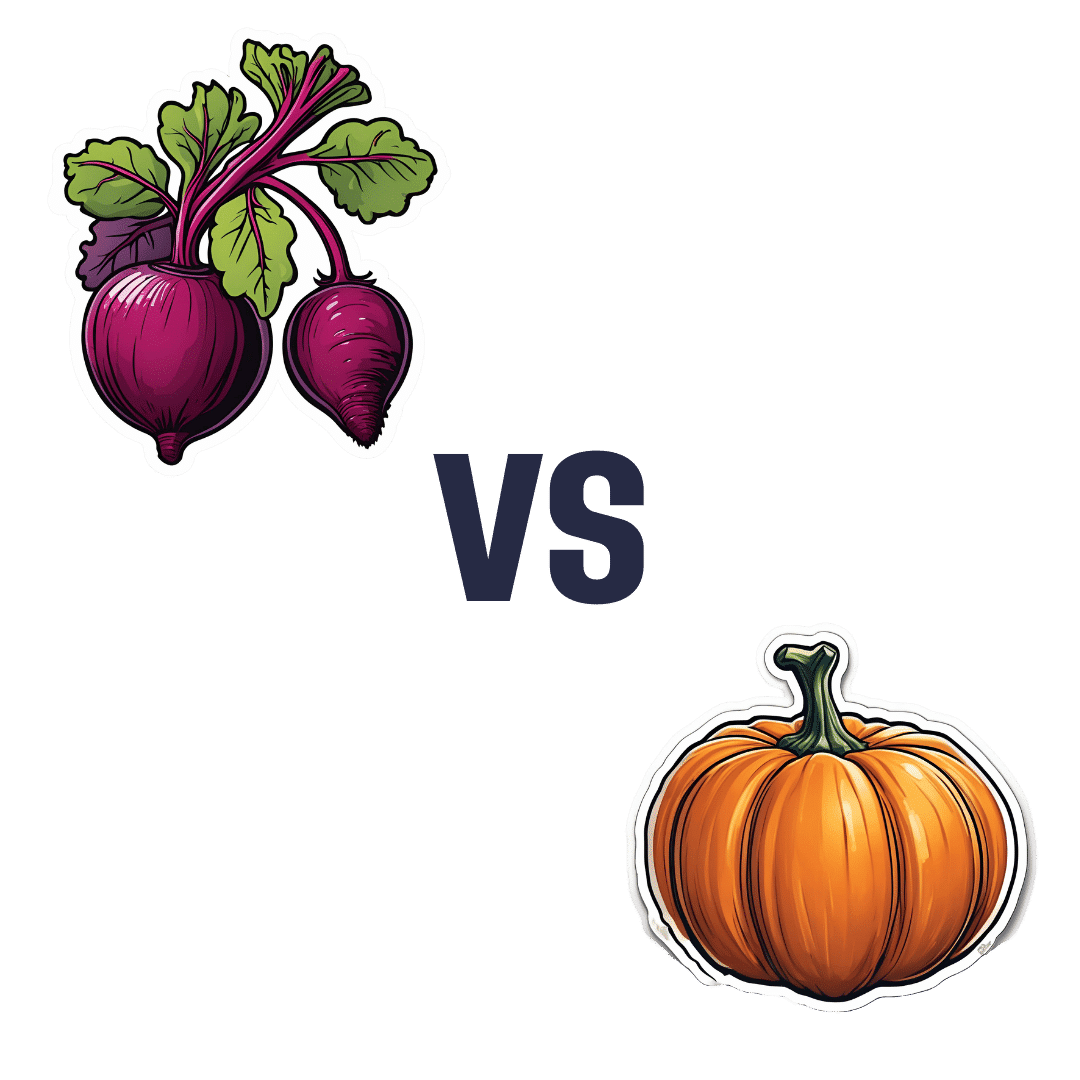
Beetroot vs Pumpkin – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing beetroot to pumpkin, we picked the beetroot.
Why?
It was close! And an argument could be made for either.
In terms of macros, beetroot has about 3x more protein and about 3x more fiber, as well as about 2x more carbs, making it the “more food per food” option. While both have a low glycemic index, we picked the beetroot here for its better numbers overall.
In the category of vitamins, beetroot has more of vitamins B6 and B9, while pumpkin has more of vitamins A, B2, B3, B5, E, and K. So, a fair win for pumpkin this time.
When it comes to minerals, though, beetroot has more calcium, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while pumpkin has a tiny bit more copper. An easy win for beetroot here.
In short, both are great, and although pumpkin shines in the vitamin category, beetroot wins on overall nutritional density.
Want to learn more?
You might like to read:
No, beetroot isn’t vegetable Viagra. But here’s what it can do
Take care!
Share This Post
Related Posts
-
Vitamin C (Drinkable) vs Vitamin C (Chewable) – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing vitamin C (drinkable) to vitamin C (chewable), we picked the drinkable.
Why?
First let’s look at what’s more or less the same in each:
- The usable vitamin C content is comparable
- The bioavailability is comparable
- The additives to hold it together are comparable
So what’s the difference?
With the drinkable, you also drink a glass of water
If you’d like to read more about how to get the most out of the vitamins you take, you can do so here:
Are You Wasting Your Vitamins? Maybe, But You Don’t Have To
If you’d like to get some of the drinkable vitamin C, here’s an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
7-Minute Face Fitness For Lymphatic Drainage & Youthful Jawline
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Valeriia Veksler is a registered nurse with a background in cosmetic medicine. She’s been practicing for 7 years, and on the strength of that, is going to teach us how to give our face some love for 7 minutes:
The routine, step by step
Preparation: clean your face and apply your usual moisturizer. Breathe deeply: Inhale through the nose, exhale to release tension.
Neck massage: use fingertips in circular motion from the bottom of the neck to the hairline and back for 30 seconds. This helps promote blood flow to the face.
Sternocleidomastoid massage: use knuckles to massage in circles from the sternal area up to the jawline and down to the collarbone for 30 seconds. Keep posture straight, shoulders down, and relax muscles.
Collarbone pressure: apply and release pressure with fingertips above the collarbones for 30 seconds. This stimulates lymphatic flow and helps reduce puffiness.
Under-chin massage: use knuckles to massage side-to-side under the chin for 30 seconds. Relax the under-chin area and promote lymphatic drainage.
Jawline massage: with knuckles, massage from the chin towards the ears in circular motion for 30 seconds. Relax the jaw.
Nasolabial fold and nose massage: place index fingers near nostrils and move mouth in a “O” shape, then massage around the nostrils and up the nose for 30 seconds.
Smile line lift: press palms on the smile lines and slide hands up towards the temples for 30 seconds. This helps lift the face and sculpt cheekbones.
Under-eye massage: use index fingers in a hook shape, massaging under the eyes along the bone structure for 30 seconds. This promotes blood flow and lymphatic drainage.
Temple lift: use fingertips to lift the area near the left temple for 30 seconds, then assist with the opposite hand to lift further. Repeat on the other side. This reduces crow’s feet and lifts the corners of the eyes.
Forehead lift: place hands on the forehead, lock fingers, and gently elevate the skin upwards. Glide fingers towards the hairline for 30 seconds. This promotes blood flow and smooths the forehead.
Relax 11 Lines: place fingers at the center of the forehead, gently press into the tissue, and let them glide away from each other towards the eyebrows for 30 seconds.
Bonus:
- Ensure good posture throughout.
- Relax, stay mindful, and breathe deeply during the exercises.
- Feel the warmth and energy from improved circulation, after the routine.
For more on all of this plus a visual demonstration of everything, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Top 10 Foods That Promote Lymphatic Drainage and Lymph Flow
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Gluconolactone Restores Immune Regulation In Lupus
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s be clear up front: this will not cure lupus.
However, it will interrupt the pathology of lupus in such a way as to, as the title says, restore immune regulation—so that your body stops attacking itself, or at the very least, attacks itself significantly less.
What is gluconolactone anyway?
Gluconolactone (also called glucono-δ-lactone) an oxidized derivative of glucose, when glucose is exposed to oxygen and a certain enzyme (glucose oxidase). It’s used in various food-related fermentation processes, and also helps such foods to have a tangy flavor.
It’s also known as E575, showing that E-numbers need not always be scary 🙂
How does it work?
First, a recap on how lupus works: lupus is an autoimmune disease where the immune system attacks its own tissues, causing inflammation and organ damage (to oversimplify it in very few words).
Next, how lupus is currently treated: mostly with immunosuppressant drugs, which reduce symptoms but have significant side effects, not least of all the fact that your immune system will be suppressed, leaving you vulnerable to infections, cancer, aging, and the like. So, there’s really a “damned if you do, damned if you don’t” aspect here (because untreated lupus will run your immune system into the ground with its chronic inflammation, which will also leave you vulnerable to the aforementioned things).
See also: How to Prevent (or Reduce) Inflammation
Now, how gluconolactone works: it increases the number of regulatory T-cells (also called “Tregs” by scientists who don’t want to have to say/write “regulatory T-cells” many times per day), which are the ones that tell the rest of your immune system what not to attack. It also inhibits pro-inflammatory T-helper-cells that are otherwise involved in autoimmune dysfunction.
Where is the science for this?
It’s a shiny new paper that covers three angles:
- In lupus-suffering mouse in vivo studies, it improved Treg function and reduced inflammatory skin rashes
- In human cell culture in vitro studies (with cell cultures from human lupus patients), it bolstered Treg count and improved immune regulation
- In human patient in vivo studies, a gluconolactone cream controlled skin inflammation and improved the clinical and histologic appearance of the skin lesions within 2 weeks
❝These results suggest that gluconolactone could be a targeted treatment option with fewer side effects for autoimmune diseases such as lupus.
Gluconolactone acts like a ‘power food’ for regulatory T cells—a real win-win situation for immune regulation❞
~ Dr. Antonios Kolios
You can find the paper itself here:
Where can I get gluconolactone?
At the moment, this is still in the clinical trials phase, so it’s not something you can get a prescription for yet, alas.
But definitely keep an eye out for it!
We would hypothesize that eating foods fermented with E575 (it’s sometimes used in feta cheese, hence today’s featured image, and it’s also often used as a pickling agent) may well help, but that’s just our hypothesis as it isn’t what was tested in the above studies.
Want to learn more?
In the meantime, if you’d like to learn more about lupus, we recommend this very comprehensive book:
*The “et al.” are: Jemima Albayda, MD; Divya Angra, MD; Alan N. Baer, MD; Sasha Bernatsky, MD, PhD; George Bertsias, MD, PhD; Ashira D. Blazer, MD; Ian Bruce, MD; Jill Buyon, MD; Yashaar Chaichian, MD; Maria Chou, MD; Sharon Christie, Esq; Angelique N. Collamer, MD; Ashté Collins, MD; Caitlin O. Cruz, MD; Mark M. Cruz, MD; Dana DiRenzo, MD; Jess D. Edison, MD; Titilola Falasinnu, PhD; Andrea Fava, MD; Cheri Frey, MD; Neda F. Gould, PhD; Nishant Gupta, MD; Sarthak Gupta, MD; Sarfaraz Hasni, MD; David Hunt, MD; Mariana J. Kaplan, MD; Alfred Kim, MD; Deborah Lyu Kim, DO; Rukmini Konatalapalli, MD; Fotios Koumpouras, MD; Vasileios C. Kyttaris, MD; Jerik Leung, MPH; Hector A. Medina, MD; Timothy Niewold, MD; Julie Nusbaum, MD; Ginette Okoye, MD; Sarah L. Patterson, MD; Ziv Paz, MD; Darryn Potosky, MD; Rachel C. Robbins, MD; Neha S. Shah, MD; Matthew A. Sherman, MD; Yevgeniy Sheyn, MD; Julia F. Simard, ScD; Jonathan Solomon, MD; Rodger Stitt, MD; George Stojan, MD; Sangeeta Sule, MD; Barbara Taylor, CPPM, CRHC; George Tsokos, MD; Ian Ward, MD; Emma Weeding, MD; Arthur Weinstein, MD; Sean A. Whelton, MD
The reason we mention this is to render it clear that this isn’t one man’s opinions (as happens with many books about certain topics), but rather, a panel of that many doctors all agreeing that this is correct and good, evidence-based, up-to-date (as of the publication of this latest revised edition) information.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: