What Flexible Dieting Really Means
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Flexibility Is The Dish Of The Day
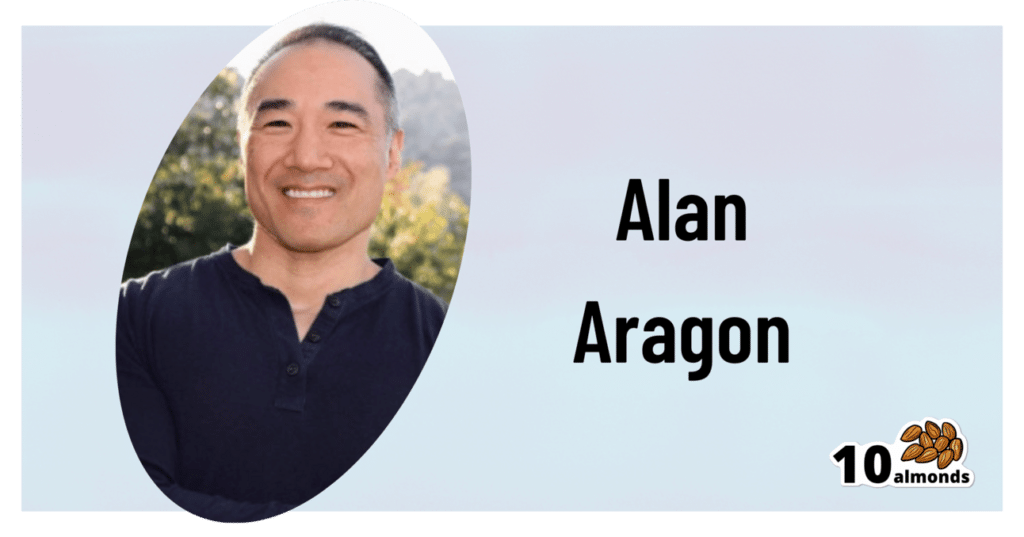
This is Alan Aragon. Notwithstanding not being a “Dr. Alan Aragon”, he’s a research scientist with dozens of peer-reviewed nutrition science papers to his name, as well as being a personal trainer and fitness educator. Most importantly, he’s an ardent champion of making people’s pursuit of health and fitness more evidence-based.
We’ll be sharing some insights from a book of his that we haven’t reviewed yet, but we will link it at the bottom of today’s article in any case.
What does he want us to know?
First, get out of the 80s and into the 90s
In the world of popular dieting, the 80s were all about calorie-counting and low-fat diets. They did not particularly help.
In the 90s, it was discovered that not only was low-fat not the way to go, but also, regardless of the diet in question, rigid dieting leads to “disinhibition”, that is to say, there comes a point (usually not far into a diet) whereby one breaks the diet, at which point, the floodgates open and the dieter binges unhealthily.
Aragon would like to bring our attention to a number of studies that found this in various ways over the course of the 90s measuring various different metrics including rigid vs flexible dieting’s impacts on BMI, weight gain, weight loss, lean muscle mass changes, binge-eating, anxiety, depression, and so forth), but we only have so much room here, so here’s a 1999 study that’s pretty much the culmination of those:
Flexible vs. Rigid Dieting Strategies: Relationship with Adverse Behavioral Outcomes
So in short: trying to be very puritan about any aspect of dieting will not only not work, it will backfire.
Next, get out of the 90s into the 00s
…which is not only fun if you read “00s” out loud as “naughties”, but also actually appropriate in this case, because it is indeed important to be comfortable being a little bit naughty:
In 2000, Dr. Marika Tiggemann found that dichotomous perceptions of food (e.g. good/bad, clean/dirty, etc) were implicated as a dysfunctional cognitive style, and predicted not only eating disorders and mood disorders, but also adverse physical health outcomes:
Dieting and Cognitive Style: The Role of Current and Past Dieting Behaviour and Cognitions
This was rendered clearer, in terms of physical health outcomes, by Dr. Susan Byrne & Dr. Emma Dove, in 2009:
❝Weight loss was negatively associated with pre-treatment depression and frequency of treatment attendance, but not with dichotomous thinking. Females who regard their weight as unacceptably high and who think dichotomously may experience high levels of depression irrespective of their actual weight, while depression may be proportionate to the degree of obesity among those who do not think dichotomously❞
Aragon’s advice based on all this: while yes, some foods are better than others, it’s more useful to see foods as being part of a spectrum, rather than being absolutist or “black and white” about it.
Next: hit those perfect 10s… Imperfectly
The next decade expanded on this research, as science is wont to do, and for this one, Aragon shines a spotlight on Dr. Alice Berg’s 2018 study with obese women averaging 69 years of age, in which…
In other words (and in fact, to borrow Dr. Berg’s words from that paper),
❝encouraging a flexible approach to eating behavior and discouraging rigid adherence to a diet may lead to better intentional weight loss for overweight and obese older women❞
You may be wondering: what did this add to the studies from the 90s?
And the key here is: rather than being observational, this was interventional. In other words, rather than simply observing what happened to people who thought one way or another, this study took people who had a rigid, dichotomous approach to food, and gave them a 6-month behavioral intervention (in other words, support encouraging them to be more flexible and open in their approach to food), and found that this indeed improved matters for them.
Which means, it’s not a matter of fate or predisposition, as it could have been back in the 90s, per “some people are just like that; who’s to say which factor causes which”. Instead, now we know that this is an approach that can be adopted, and it can be expected to work.
Beyond weight loss
Now, so far we’ve talked mostly about weight loss, and only touched on other health outcomes. This is because:
- weight loss a very common goal for many
- it’s easy to measure so there’s a lot of science for it
Incidentally, if it’s a goal of yours, here’s what 10almonds had to say about that, along with two follow-up articles for other related goals:
Spoiler: we agree with Aragon, and recommend a relaxed and flexible approach to all three of these things
Aragon’s evidence-based approach to nutrition has found that this holds true for other aspects of healthy eating, too. For example…
To count or not to count?
It’s hard to do evidence-based anything without counting, and so Aragon talks a lot about this. Indeed, he does a lot of counting in scientific papers of his own, such as:
and
The effect of protein timing on muscle strength and hypertrophy: a meta-analysis
…as well as non-protein-related but diet-related topics such as:
But! For the at-home health enthusiast, Aragon recommends that the answer to the question “to count or not to count?” is “both”:
- Start off by indeed counting and tracking everything that is important to you (per whatever your current personal health intervention is, so it might be about calories, or grams of protein, or grams of carbs, or a certain fat balance, or something else entirely)
- Switch to a more relaxed counting approach once you get used to the above. By now you probably know the macros for a lot of your common meals, snacks, etc, and can tally them in your head without worrying about weighing portions and knowing the exact figures.
- Alternatively, count moderately standardized portions of relevant foods, such as “three servings of beans or legumes per day” or “no more than one portion of refined carbohydrates per day”
- Eventually, let habit take the wheel. Assuming you have established good dietary habits, this will now do you just fine.
This latter is the point whereby the advice (that Aragon also champions) of “allow yourself an unhealthy indulgence of 10–20% of your daily food”, as a budget of “discretionary calories”, eventually becomes redundant—because chances are, you’re no longer craving that donut, and at a certain point, eating foods far outside the range of healthiness you usually eat is not even something that you would feel inclined to do if offered.
But until that kicks in, allow yourself that budget of whatever unhealthy thing you enjoy, and (this next part is important…) do enjoy it.
Because it is no good whatsoever eating that cream-filled chocolate croissant and then feeling guilty about it; that’s the dichotomous thinking we had back in the 80s. Decide in advance you’re going to eat and enjoy it, then eat and enjoy it, then look back on it with a sense of “that was enjoyable” and move on.
The flipside of this is that the importance of allowing oneself a “little treat” is that doing so actively helps ensure that the “little treat” remains “little”. Without giving oneself permission, then suddenly, “well, since I broke my diet, I might as well throw the whole thing out the window and try again on Monday”.
On enjoying food fully, by the way:
Mindful Eating: How To Get More Nutrition Out Of The Same Food
Want to know more from Alan Aragon?
Today we’ve been working heavily from this book of his; we haven’t reviewed it yet, but we do recommend checking it out:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Chaga Mushrooms’ Immune & Anticancer Potential
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What Do Chaga Mushrooms Do?
Chaga mushrooms, which also go by other delightful names including “sterile conk trunk rot” and “black mass”, are a type of fungus that grow on birch trees in cold climates such as Alaska, Northern Canada, Northern Europe, and Siberia.
They’ve enjoyed a long use as a folk remedy in Northern Europe and Siberia, mostly to boost immunity, mostly in the form of a herbal tea.
Let’s see what the science says…
Does it boost the immune system?
It definitely does if you’re a mouse! We couldn’t find any studies on humans yet. But for example:
- Immunomodulatory Activity of the Water Extract from Medicinal Mushroom Inonotus obliquus
- Inonotus obliquus extracts suppress antigen-specific IgE production through the modulation of Th1/Th2 cytokines in ovalbumin-sensitized mice
(cytokines are special proteins that regulate the immune system, and Chaga tells them to tell the body to produce more white blood cells)
Wait, does that mean it increases inflammation?
Definitely not if you’re a mouse! We couldn’t find any studies on humans yet. But for example:
- Anti-inflammatory effects of orally administered Inonotus obliquus in ulcerative colitis
- Orally administered aqueous extract of Inonotus obliquus ameliorates acute inflammation
Anti-inflammatory things often fight cancer. Does chaga?
Definitely if you’re a mouse! We couldn’t find any studies in human cancer patients yet. But for example:
While in vivo human studies are conspicuous by their absence, there have been in vitro human studies, i.e., studies performed on cancerous human cell samples in petri dishes. They are promising:
- Anticancer activities of extracts and compounds from the mushroom Inonotus obliquus
- Extract of Innotus obliquus induces G1 cell cycle arrest in human colon cancer cells
- Anticancer activity of Inonotus obliquus extract in human cancer cells
I heard it fights diabetes; does it?
You’ll never see this coming, but: definitely if you’re a mouse! We couldn’t find any human studies yet. But for example:
- Anti-diabetic effects of Inonotus obliquus in type 2 diabetic mice
- Anti-diabetic effects of Inonotus obliquus in type 2 diabetic mice and potential mechanism
Is it safe?
Honestly, there simply have been no human safety studies to know for sure, or even to establish an appropriate dosage.
Its only-partly-understood effects on blood sugar levels and the immune system may make it more complicated for people with diabetes and/or autoimmune disorders, and such people should definitely seek medical advice before taking chaga.
Additionally, chaga contains a protein that can prevent blood clotting. That might be great by default if you are at risk of blood clots, but not so great if you are already on blood-thinning medication, or otherwise have a bleeding disorder, or are going to have surgery soon.
As with anything, we’re not doctors, let alone your doctors, so please consult yours before trying chaga.
Where can we get it?
We don’t sell it (or anything else), but for your convenience, here’s an example product on Amazon.
Enjoy!
Share This Post
-
Fight Inflammation & Protect Your Brain, With Quercetin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Querying Quercetin
Quercetin is a flavonoid (and thus, antioxidant) pigment found in many plants. Capers, radishes, and coriander/cilantro score highly, but the list is large:
USDA Database for the Flavonoid Content of Selected Foods
Indeed,
❝Their regular consumption is associated with reduced risk of a number of chronic diseases, including cancer, cardiovascular disease (CVD) and neurodegenerative disorders❞
~ Dr. Aleksandra Kozłpwsla & Dr. Dorota Szostak-Wegierek
Read more: Flavonoids—food sources and health benefits
For this reason, quercetin is often sold/consumed as a supplement on the strength of its health-giving properties.
But what does the science say?
Quercetin and inflammation
In short, it helps:
❝500 mg per day quercetin supplementation for 8 weeks resulted in significant improvements in clinical symptoms, disease activity, hs-TNFα, and Health Assessment Questionnaire scores in women with rheumatoid athritis❞
Quercetin and blood pressure
It works, if antihypertensive (i.e., blood pressure lowering) effect is what you want/need:
❝…significant effect of quercetin supplementation in the reduction of BP, possibly limited to, or greater with dosages of >500 mg/day.❞
~ Dr. Maria-Corina Serban et al.
Quercetin and diabetes
We’re less confident to claim this one, because (almost?) all of the research so far as been in non-human animals or in vitro. As one team of researchers put it:
❝Despite the wealth of in animal research results suggesting the anti-diabetic and its complications potential of quercetin, its efficacy in diabetic human subjects is yet to be explored❞
Quercetin and neuroprotection
Research has been done into the effect of quercetin on the risk of Parkinson’s disease and Alzheimer’s disease, and they found…
❝The data indicate that quercetin is the major neuroprotective component in coffee against Parkinson’s disease and Alzheimer’s disease❞
Read more: Quercetin, not caffeine, is a major neuroprotective component in coffee
Summary
Quercetin is a wonderful flavonoid that can be enjoyed as part of one’s diet and by supplementation. In terms of its popular health claims:
- It has been found very effective for lowering inflammation
- It has a moderate blood pressure lowering effect
- It may have anti-diabetes potential, but the science is young
- It has been found to have a potent neuroprotective effect
Want to get some?
We don’t sell it, but for your convenience, here’s an example product on Amazon
Enjoy!
Share This Post
-
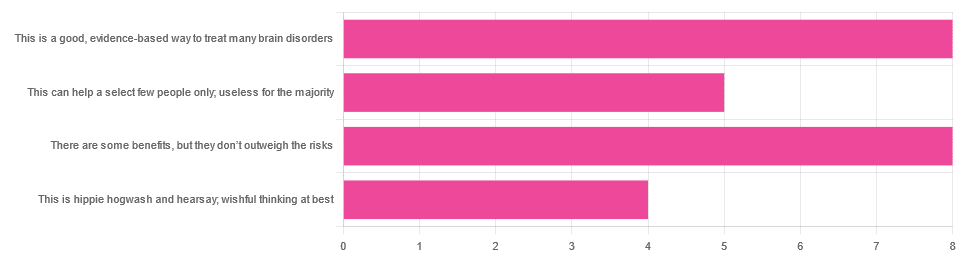
Taking A Trip Through The Evidence On Psychedelics
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In Tuesday’s newsletter, we asked you for your opinions on the medicinal use of psychedelics, and got the above-depicted, below-described, set of responses:
- 32% said “This is a good, evidence-based way to treat many brain disorders”
- 32% said “There are some benefits, but they don’t outweigh the risks”
- 20% said “This can help a select few people only; useless for the majority”
- 16% said “This is hippie hogwash and hearsay; wishful thinking at best”
Quite a spread of answers, so what does the science say?
This is hippie hogwash and hearsay; wishful thinking at best! True or False?
False! We’re tackling this one first, because it’s easiest to answer:
There are some moderately-well established [usually moderate] clinical benefits from some psychedelics for some people.
If that sounds like a very guarded statement, it is. Part of this is because “psychedelics” is an umbrella term; perhaps we should have conducted separate polls for psilocybin, MDMA, ayahuasca, LSD, ibogaine, etc, etc.
In fact: maybe we will do separate main features for some of these, as there is a lot to say about each of them separately.
Nevertheless, looking at the spread of research as it stands for psychedelics as a category, the answers are often similar across the board, even when the benefits/risks may differ from drug to drug.
To speak in broad terms, if we were to make a research summary for each drug it would look approximately like this in each case:
- there has been research into this, but not nearly enough, as “the war on drugs” may well have manifestly been lost (the winner of the war being: drugs; still around and more plentiful than ever), but it did really cramp science for a few decades.
- the studies are often small, heterogenous (often using moderately wealthy white student-age population samples), and with a low standard of evidence (i.e. the methodology often has some holes that leave room for reasonable doubt).
- the benefits recorded are often small and transient.
- in their favor, though, the risks are also generally recorded as being quite low, assuming proper safe administration*.
*Illustrative example:
Person A takes MDMA in a club, dances their cares away, has had only alcohol to drink, sweats buckets but they don’t care because they love everyone and they see how we’re all one really and it all makes sense to them and then they pass out from heat exhaustion and dehydration and suffer kidney damage (not to mention a head injury when falling) and are hospitalized and could die;
Person B takes MDMA in a lab, is overwhelmed with a sense of joy and the clarity of how their participation in the study is helping humanity; they want to hug the researcher and express their gratitude; the researcher reminds them to drink some water.
Which is not to say that a lab is the only safe manner of administration; there are many possible setups for supervised usage sites. But it does mean that the risks are often as much environmental as they are risks inherent to the drug itself.
Others are more inherent to the drug itself, such as adverse cardiac events for some drugs (ibogaine is one that definitely needs medical supervision, for example).
For those who’d like to see numbers and clinical examples of the bullet points we gave above, here you go; this is a great (and very readable) overview:
NIH | Evidence Brief: Psychedelic Medications for Mental Health and Substance Use Disorders
Notwithstanding the word “brief” (intended in the sense of: briefing), this is not especially brief and is rather an entire book (available for free, right there!), but we do recommend reading it if you have time.
This can help a select few people only; useless for the majority: True or False?
True, technically, insofar as the evidence points to these drugs being useful for such things as depression, anxiety, PTSD, addiction, etc, and estimates of people who struggle with mental health issues in general is often cited as being 1 in 4, or 1 in 5. Of course, many people may just have moderate anxiety, or a transient period of depression, etc; many, meanwhile, have it worth.
In short: there is a very large minority of people who suffer from mental health issues that, for each issue, there may be one or more psychedelic that could help.
This is a good, evidence-based way to treat many brain disorders: True or False?
True if and only if we’re willing to accept the so far weak evidence that we discussed above. False otherwise, while the jury remains out.
One thing in its favor though is that while the evidence is weak, it’s not contradictory, insofar as the large preponderance of evidence says such therapies probably do work (there aren’t many studies that returned negative results); the evidence is just weak.
When a thousand scientists say “we’re not completely sure, but this looks like it helps; we need to do more research”, then it’s good to believe them on all counts—the positivity and the uncertainty.
This is a very different picture than we saw when looking at, say, ear candling or homeopathy (things that the evidence says simply do not work).
We haven’t been linking individual studies so far, because that book we linked above has many, and the number of studies we’d have to list would be:
n = number of kinds of psychedelic drugs x number of conditions to be treated
e.g. how does psilocybin fare for depression, eating disorders, anxiety, addiction, PTSD, this, that, the other; now how does ayahuasca fare for each of those, and so on for each drug and condition; at least 25 or 30 as a baseline number, and we don’t have that room.
But here are a few samples to finish up:
- Psilocybin as a New Approach to Treat Depression and Anxiety in the Context of Life-Threatening Diseases—A Systematic Review and Meta-Analysis of Clinical Trials
- Therapeutic Use of LSD in Psychiatry: A Systematic Review of Randomized-Controlled Clinical Trials
- Efficacy of Psychoactive Drugs for the Treatment of Posttraumatic Stress Disorder: A Systematic Review of MDMA, Ketamine, LSD and Psilocybin
- Changes in self-rumination and self-compassion mediate the effect of psychedelic experiences on decreases in depression, anxiety, and stress.
- Psychedelic Treatments for Psychiatric Disorders: A Systematic Review and Thematic Synthesis of Patient Experiences in Qualitative Studies
- Repeated lysergic acid diethylamide (LSD) reverses stress-induced anxiety-like behavior, cortical synaptogenesis deficits and serotonergic neurotransmission decline
In closing…
The general scientific consensus is presently “many of those drugs may ameliorate many of those conditions, but we need a lot more research before we can say for sure”.
On a practical level, an important take-away from this is twofold:
- drugs, even those popularly considered recreational, aren’t ontologically evil, generally do have putative merits, and have been subject to a lot of dramatization/sensationalization, especially by the US government in its famous war on drugs.
- drugs, even those popularly considered beneficial and potentially lifechangingly good, are still capable of doing great harm if mismanaged, so if putting aside “don’t do drugs” as a propaganda of the past, then please do still hold onto “don’t do drugs alone”; trained professional supervision is a must for safety.
Take care!
Share This Post
Related Posts
-
Pneumonia: Prevention Is Better Than Cure
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pneumonia: What We Can & Can’t Do About It
Pneumonia is a significant killer of persons over the age of 65, with the risk increasing with age after that, rising very sharply around the age of 85:
While pneumonia is treatable, especially in young healthy adults, the risks get more severe in the older age brackets, and it’s often the case that someone goes into hospital with one thing, then develops pneumonia, which the person was already not in good physical shape to fight, because of whatever hospitalized them in the first place:
American Lung Association | Pneumonia Treatment and Recovery
Other risk factors besides age
There are a lot of things that can increase our risk factor for pneumonia; they mainly fall into the following categories:
- Autoimmune diseases
- Other diseases of the immune system (e.g. HIV)
- Medication-mediated immunosuppression (e.g. after an organ transplant)
- Chronic lung diseases (e.g. asthma, COPD, Long Covid, emphysema, etc)
- Other serious health conditions ← we know this one’s broad, but it encompasses such things as diabetes, heart disease, and cancer
See also:
Why Chronic Obstructive Pulmonary Disease (COPD) Is More Likely Than You Think
Things we can do about it
When it comes to risks, we can’t do much about our age and some of the other above factors, but there are other things we can do to reduce our risk, including:
- Get vaccinated against pneumonia if you are over 65 and/or have one of the aforementioned risk factors. This is not perfect (it only reduces the risk for certain kinds of infection) and may not be advisable for everyone (like most vaccines, it can put the body through its paces a bit after taking it), so speak with your own doctor about this, of course.
- See also: Vaccine Mythbusting
- Avoid contagion. While pneumonia itself is not spread person-to-person, it is caused by bacteria or viruses (there are numerous kinds) that are opportunistic and often become a secondary infection when the immune system is already busy with the first one. So, if possible avoid being in confined spaces with many people, and do wash your hands regularly (as a lot of germs are transferred that way and can get into the respiratory tract because you touched your face or such).
- See also: The Truth About Handwashing
- If you have a cold, or flu, or other respiratory infection, take it seriously, rest well, drink fluids, get good immune-boosting nutrients. There’s no such thing as “just a cold”; not anymore.
- Look after your general health too—health doesn’t exist in a vacuum, and nor does disease. Every part of us affects every other part of us, so anything that can be in good order, you want to be in good order.
This last one, by the way? It’s an important reminder that while some diseases (such as some of the respiratory infections that can precede pneumonia) are seasonal, good health isn’t.
We need to take care of our health as best we can every day along the way, because we never know when something could change.
Want to do more?
Check out: Seven Things To Do For Good Lung Health!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Relationships: When To Stick It Out & When To Call It Quits
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Like A Ship Loves An Anchor?
Today’s article may seem a little bit of a downer to start with, but don’t worry, it picks up again too. Simply put, we’ve written before about many of the good parts of relationships, e.g:
Only One Kind Of Relationship Promotes Longevity This Much!
…but what if that’s not what we have?
Note: if you have a very happy, secure, fulfilling, joyous relationship, then, great! Or if you’re single and happy, then, also great! Hopefully you will still find today’s feature of use if you find yourself advising a friend or family member one day. So without further ado, let’s get to it…
You may be familiar with the “sunk cost fallacy”; if not: it’s what happens when a person or group has already invested into a given thing, such that even though the thing is not going at all the way they hoped, they now want to continue trying to make that thing work, lest their previous investment be lost. But the truth is: if it’s not going to work, then the initial investment is already lost, and pouring out extra won’t help—it’ll just lose more.
That “investment” in a given thing could be money, time, energy, or (often the case) a combination of the above.
In the field of romance, the “sunk cost fallacy” keeps a lot of bad relationships going for longer than perhaps they should, and looking back (perhaps after a short adjustment period), the newly-single person says “why did I let that go on?” and vows to not make the same mistake again.
But that prompts the question: how can we know when it’s right to “keep working on it, because relationships do involve work”, as perfectly reasonable relationship advice often goes, and when it’s right to call it quits?
Should I stay or should I go?
Some questions for you (or perhaps a friend you might find yourself advising) to consider:
- What qualities do you consider the most important for a partner to have—and does your partner have them?
- If you described the worst of your relationship to a close friend, would that friend feel bad for you?
- Do you miss your partner when they’re away, or are you glad of the break? When they return, are they still glad to see you?
- If you weren’t already in this relationship, would you seek to enter it now? (This takes away sunk cost and allows a more neutral assessment)
- Do you feel completely safe with your partner (emotionally as well as physically), or must you tread carefully to avoid conflict?
- If your partner decided tomorrow that they didn’t want to be with you anymore and left, would that be just a heartbreak, or an exciting beginning of a new chapter in your life?
- What things would you generally consider dealbreakers in a relationship—and has your partner done any of them?
The last one can be surprising, by the way. We often see or hear of other people’s adverse relationship situations and think “I would never allow…” yet when we are in a relationship and in love, there’s a good chance that we might indeed allow—or rather, excuse, overlook, and forgive.
And, patience and forgiveness certainly aren’t inherently bad traits to have—it’s just good to deploy them consciously, and not merely be a doormat.
Either way, reflect (or advise your friend/family member to reflect, as applicable) on the “score” from the above questions.
- If the score is good, then maybe it really is just a rough patch, and the tools we link at the top and bottom of this article might help.
- If the score is bad, the relationship is bad, and no amount of historic love or miles clocked up together will change that. Sometimes it’s not even anyone’s fault; sometimes a relationship just ran its course, and now it’s time to accept that and turn to a new chapter.
“At my age…”
As we get older, it’s easy for that sunk cost fallacy to loom large. Inertia is heavy, the mutual entanglement of lives is far-reaching, and we might not feel we have the same energy for dating that we did when we were younger.
And there may sometimes be a statistical argument for “sticking it out” at least for a while, depending on where we are in the relationship, per this study (with 165,039 participants aged 20–76), which found:
❝Results on mean levels indicated that relationship satisfaction decreased from age 20 to 40, reached a low point at age 40, then increased until age 65, and plateaued in late adulthood.
As regards the metric of relationship duration, relationship satisfaction decreased during the first 10 years of the relationship, reached a low point at 10 years, increased until 20 years, and then decreased again.❞
Source: Development of Relationship Satisfaction Across the Life Span: A Systematic Review and Meta-Analysis
And yet, when it comes to prospects for a new relationship…
- If our remaining life is growing shorter, then it’s definitely too short to spend in an unhappy relationship
- Maybe we really won’t find romance again… And maybe that’s ok, if w’re comfortable making our peace with that and finding joy in the rest of life (this widowed writer (hi, it’s me) plans to remain single now by preference, and her life is very full of purpose and beauty and joy and yes, even love—for family, friends, etc, plus the memory of my wonderful late beloved)
- Nevertheless, the simple fact is: many people do find what they go on to describe as their best relationship yet, late in life ← this study is with a small sample size, but in this case, even anecdotal evidence seems sufficient to make the claim reasonable; probably you personally know someone who has done so. If they can, so can you, if you so wish.
- Adding on to that last point… Later life relationships can also offer numerous significant advantages unique to such (albeit some different challenges too—but with the right person, those challenges are just a fun thing to tackle together). See for example:
An exploratory investigation into dating among later‐life women
And about those later-life relationships that do work? They look like this:
this one looks like the title says it all, but it really doesn’t, and it’s very much worth at least reading the abstract, if not the entire paper—because it talks a lot about the characteristics that make for happy or unhappy relationships, and the effect that those things have on people. It really is very good, and quite an easy read.
See again: Healthy Relationship, Healthy Life
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Almonds vs Walnuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing almonds to walnuts, we picked the almonds.
Why?
It wasn’t just our almond bias, but it was close!
In terms of macros, the main important differences are:
- Almonds are higher in protein
- Walnuts are higher in fats (they are healthy fats)
So far, so even.
In terms of vitamins, both are rich in many vitamins; mostly the same ones. However, walnuts have more of most of the B vitamins (except for B2 and B3, where almonds win easily), and almonds have more vitamin E by several orders of magnitude.
So far, so balanced.
Almonds have slightly more choline.
Almonds have a better mineral profile, with more of most minerals that they both contain, and especially, a lot more calcium.
Both nuts have [sometimes slightly different, but] comparable benefits against diabetes, cancer, neurodegeneration, and other diseases.
In summary
This one’s close. After balancing out the various “almonds have this but walnuts have that” equal-but-different benefits, we’re going to say almonds take first place by virtue of the better mineral profile, and more choline.
But: enjoy both!
Learn more
You might like this previous article of ours:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: