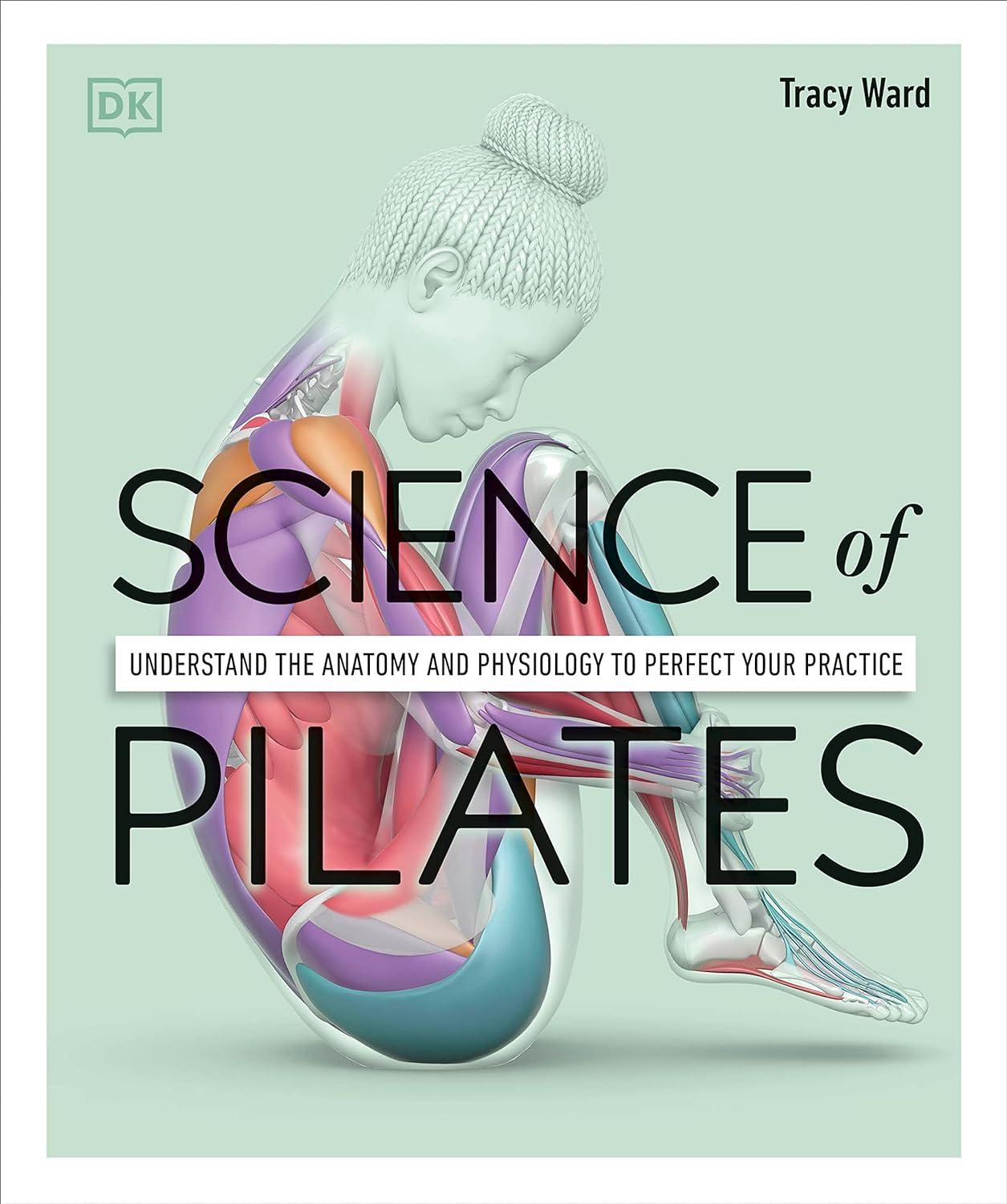
Science of Pilates – by Tracy Ward
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed other books in this series, “Science of Yoga” and “Science of HIIT” (they’re great too; check them out!). What does this one add to the mix?
Pilates is a top-tier “combination exercise” insofar as it checks a lot of boxes, e.g:
- Strength—especially core strength, but also limbs
- Mobility—range of motion and resultant reduction in injury risk
- Stability—impossible without the above two things, but Pilates trains this too
- Fitness—many dynamic Pilates exercises can be performed as cardio and/or HIIT.
The author, a physiotherapist, explains (as the title promises!) the science of Pilates, with:
- the beautifully clear diagrams we’ve come to expect of this series,
- equally clear explanations, with a great balance of simplicity of terms and depth where necessary, and
- plenty of citations for the claims made, linking to lots of the best up-to-date science.
Bottom line: if you are in a position to make a little time for Pilates (if you don’t already), then there is nobody who would not benefit from reading this book.
Click here to check out Science of Pilates, and keep your body well!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
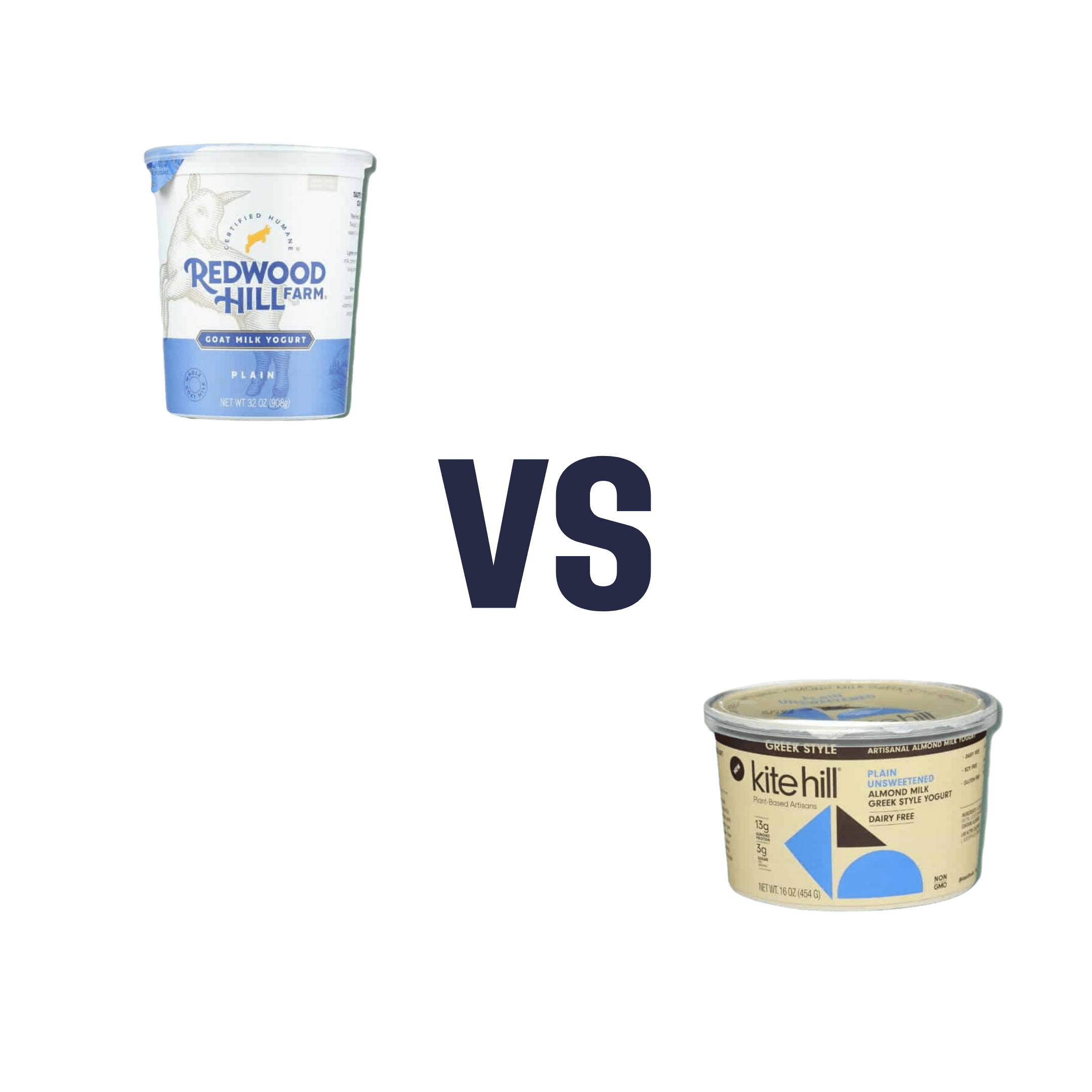
Goat Milk Greek Yogurt vs Almond Milk Greek Yogurt – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing goat milk yogurt to almond milk yogurt, we picked the almond milk yogurt.
Why?
Surprised? Honestly, we were too!
Much as we love almonds, we were fully expecting to write about how they’re very close in nutritional value, but the dairy yogurt has more probiotics, but no, as it turns out when we looked into them, they’re quite comparable in that regard.
It’s easy to assume “goat milk yogurt is more natural and therefore healthier”, but in both cases, it was a case of taking a fermentable milk, and fermenting it (an ancient process). “But almond milk is a newfangled thing”, well, new-ish…
So what was the deciding factor?
In this case, the almond milk yogurt has about twice the protein per (same size) serving, compared to the goat milk; all the other macros are about the same, and the micronutrients are similar. Like many plant-based milks and yogurts, this one is fortified with calcium and vitamin D, so that wasn’t an issue either.
In short: the only meaningful difference was the protein, and the almond came out on top.
However!
The almond came out on top only because it is strained; this can be done (or not) with any kind of yogurt, be it from an animal or a plant.
In other words: if it had been different brands, the goat milk yogurt could have come out on top!
The take-away idea here is: always read labels, because as you’ve just seen, even we can get surprised sometimes!
seriously if you only remember one thing from this today, make it the above
Other thing worth mentioning: yogurts, and dairy products in general, are often made with common allergens (e.g. dairy, nuts, soy, etc). So if you are allergic or intolerant, obviously don’t choose the one to which you are allergic or intolerant.
That said… If you are lactose-intolerant, but not allergic, goat’s milk does have less lactose than cow’s milk. But of course, you know your limits better than we can in this regard.
Want to try some?
Amazon is not coming up with the goods for this one (or anything even similar, at time of writing), so we recommend trying your local supermarket (and reading labels, because products vary widely!)
What you’re looking for (be it animal- or plant-based):
- Live culture probiotic bacteria
- No added sugar
- Minimal additives in general
- Lastly, check out the amounts for protein, calcium, vitamin D, etc.
Enjoy!
Share This Post
-
‘Free birthing’ and planned home births might sound similar but the risks are very different
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The death of premature twins in Byron Bay in an apparent “wild birth”, or free birth, last week has prompted fresh concerns about giving birth without a midwife or medical assistance.
This follows another case from Victoria this year, where a baby was born in a critical condition following a reported free birth.
It’s unclear how common free birthing is, as data is not collected, but there is some evidence free births increased during the COVID pandemic.
Planned home births also became more popular during the pandemic, as women preferred to stay away from hospitals and wanted their support people with them.
But while free births and home births might sound similar, they are a very different practice, with free births much riskier. So what’s the difference, and why might people opt for a free birth?
What are home births?
Planned home births involve care from midwives, who are registered experts in childbirth, in a woman’s home.
These registered midwives work privately, or are part of around 20 publicly funded home birth programs nationally that are attached to hospitals.
They provide care during the pregnancy, labour and birth, and in the first six weeks following the birth.
The research shows that for women with low risk pregnancies, planned home births attended by competent midwives (with links to a responsive mainstream maternity system) are safe.
Home births result in less intervention than hospital births and women perceive their experience more positively.
What are free births?
A free birth is when a woman chooses to have a baby, usually at home, without a registered health professional such as a midwife or doctor in attendance.
Different terms such as unassisted birth or wild pregnancy or birth are also used to refer to free birth.
The parents may hire an unregulated birth worker or doula to be a support at the birth but they do not have the training or medical equipment needed to manage emergencies.
Women may have limited or no health care antenatally, meaning risk factors such as twins and breech presentations (the baby coming bottom first) are not detected beforehand and given the right kind of specialist care.
Why do some people choose to free birth?
We have been studying the reasons women and their partners choose to free birth for more than a decade. We found a previous traumatic birth and/or feeling coerced into choices that are not what the woman wants were the main drivers for avoiding mainstream maternity care.
Australia’s childbirth intervention rates – for induction or augmentation of labour, episiotomy (cutting the tissue between the vaginal opening and the anus) and caesarean section – are comparatively high.
One in ten women report disrespectful or abusive care in childbirth and some decide to make different choices for future births.
Lack of options for a natural birth and birth choices such as home birth or birth centre birth also played a major role in women’s decision to free birth.
Publicly funded home birth programs have very strict criteria around who can be accepted into the program, excluding many women.
In other countries such as the United Kingdom, Netherlands and New Zealand, publicly funded home births are easier to access.
It can be difficult to access home birth services in Australia.
Ink Drop/ShutterstockOnly around 200 midwives provide private midwifery services for home births nationally. Private midwives are yet to obtain insurance for home births, which means they are risking their livelihoods if something goes wrong and they are sued.
The cost of a home birth with a private midwife is not covered by Medicare and only some health funds rebate some of the cost. This means women can be out of pocket A$6-8,000.
Access to home birth is an even greater issue in rural and remote Australia.
How to make mainstream care more inclusive
Many women feel constrained by their birth choices in Australia. After years of research and listening to thousands of women, it’s clear more can be done to reduce the desire to free birth.
As my co-authors and I outline in our book, Birthing Outside the System: The Canary in the Coal Mine, this can be achieved by:
- making respectful care a reality so women aren’t traumatised and alienated by maternity care and want to engage with it
- supporting midwifery care. Women are seeking more physiological and social ways of birthing, minimising birth interventions, and midwives are the experts in this space
- supporting women’s access to their chosen place of birth and model of care and not limiting choice with high out-of-pocket expenses
- providing more flexible, acceptable options for women experiencing risk factors during pregnancy and/or birth, such as having a previous caesarean birth, having twins or having a baby in breech position. Women experiencing these complications experience pressure to have a caesarean section
- getting the framework right with policies, guidelines, education, research, regulation and professional leadership.
Ensuring women’s rights and choices are informed and respected means they’re less likely to feel they’re left with no other option.
Hannah Dahlen, Professor of Midwifery, Associate Dean Research and HDR, Midwifery Discipline Leader, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Hormone Replacement
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I cant believe 10 Almonds addresses questions. Thanks. I see the word symptoms for menopause. I don’t know what word should replace it but maybe one should be used or is symptom accurate? And I recently read that there was a great disservice for women in my era as they were denied/scared of hormones replacement. Unnecessarily❞
You’d better believe it! In fact we love questions; they give us things to research and write about.
“Symptom” is indeed an entirely justified word to use, being:
- General: any phenomenon or circumstance accompanying something and serving as evidence of it.
- Medical: any phenomenon that arises from and accompanies a particular disease or disorder and serves as an indication of it.
If the question is more whether the menopause can be considered a disease/disorder, well, it’s a naturally occurring and ultimately inevitable change, yes, but then, so is cancer (it’s in the simple mathematics of DNA replication and mutation that, unless a cure for cancer is found, we will always eventually get cancer, if nothing else kills us first).
So, something being natural/inevitable isn’t a reason to not consider it a disease/disorder, nor a reason to not treat it as appropriate if it is causing us harm/discomfort that can be safely alleviated.
Moreover, and semantics aside, it is medical convention to consider menopause to be a medical condition, that has symptoms. Indeed, for example, the US’s NIH (and its constituent NIA, the National Institute of Aging) and the UK’s NHS, both list the menopause’s symptoms, using that word:
- NIA (NIH): What are the signs and symptoms of menopause?
- NHS: Common symptoms of menopause and perimenopause
With regard to fearmongering around HRT, certainly that has been rife, and there were some very flawed (and later soundly refuted) studies a while back that prompted this—and even those flawed studies were not about the same (bioidentical) hormones available today, in any case. So even if they had been correct (they weren’t), it still wouldn’t be a reason to not get treatment nowadays, if appropriate!
Share This Post
Related Posts
-
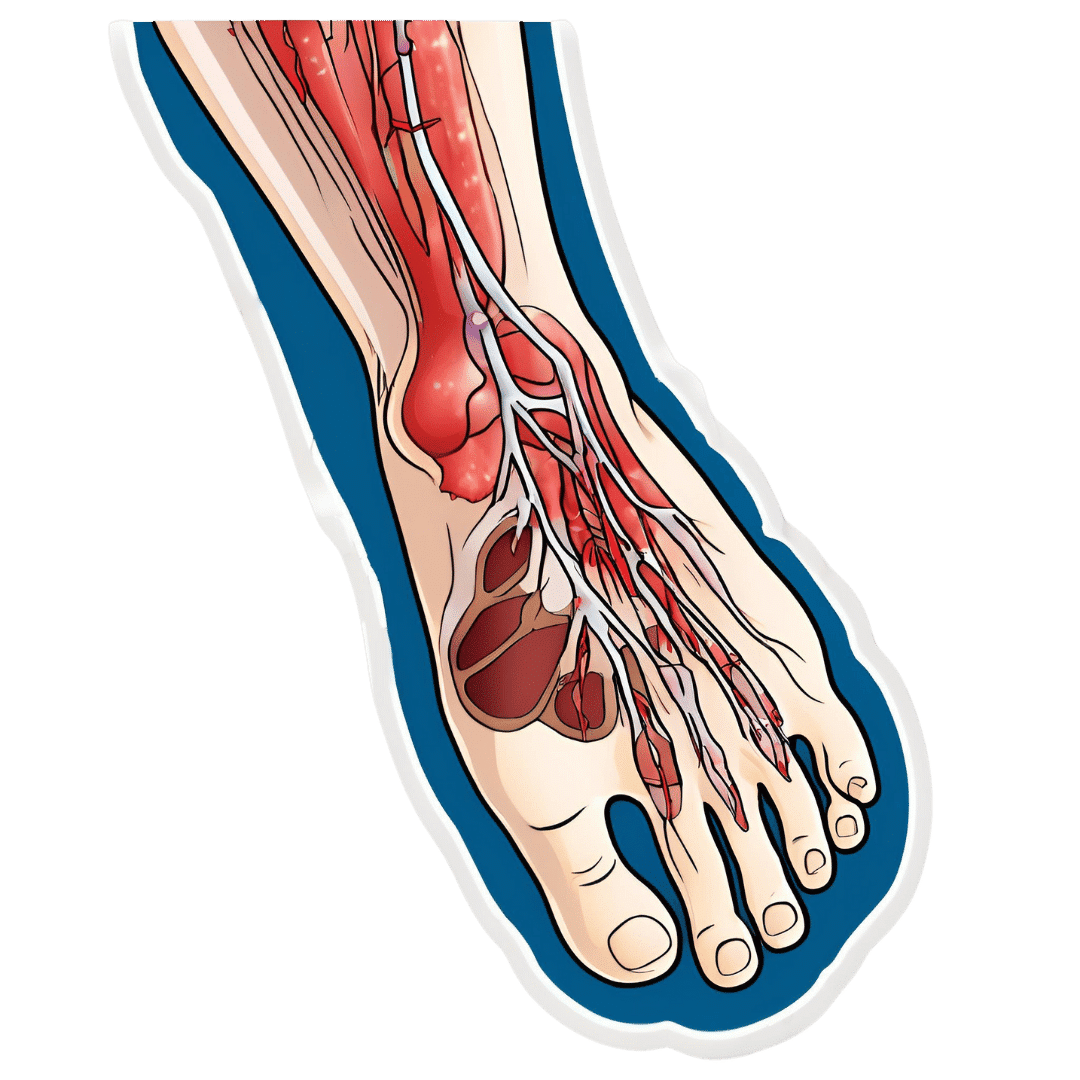
How To Stay A Step Ahead Of Peripheral Artery Disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Far less well-known than Coronary Artery Disease, it can still result in loss of life and limb (not in that order). Fortunately, there are ways to be on your guard:
What it is
Peripheral Artery Disease (PAD) is the same thing as Coronary Artery Disease (CAD), just, in the periphery—which by definition means “outside of the heart and brain”, but in practice, it starts with the extremities. And of the extremities, it tends to start with the feet and legs, for the simple reason that if someone’s circulation is sluggish, then because of gravity, that’s where’s going to get blocked first.
In both CAD and PAD, the usual root cause is atherosclerosis, that is to say, the build-up of fatty material inside the arteries, usually commensurate to LDL (“bad”) cholesterol, especially in men (high LDL is still a predictor of cardiovascular disease in women though, just more modestly so, at least pre-menopause or in cases of treated menopause whereby HRT has returned hormones to pre-menopause levels).
See also: Demystifying Cholesterol
And for that about sex differences: His & Hers: The Hidden Complexities of Statins and Cardiovascular Disease (CVD)
Why it is
This one’s straightforward, as it’s the same things as any kind of cardiovascular disease: high blood pressure, high cholesterol, older age, obesity, smoking, drinking, diabetes, and genetic factors (so, a risk factor is: family history of heart disease).
However, while those are the main causes and/or risk factors, it absolutely can still strike other people, so it’s as well to be watch out for…
What to look out for
Many people first notice signs and symptoms that turn out to be PAD when they experience pain or numbness in the foot or feet, and/or a discoloration of the feet (especially toes), and slow wound healing.
At that stage, chances are you will need to go urgently to a specialist, and surgery is a likely necessity. With a little luck, it’ll be a minimally-invasive surgery to unblock an artery; failing that, an amputation will be in order.
At that stage, under 50% will be alive 5 years from diagnosis:
You probably want to avoid those. Good news is, you can, by catching it earlier!
What to look out for before that
The most common test for PAD is one you can do at home, but enlisting a nurse to do it for you will help ensure accurate readings. It’s called the Ankle-Brachial Index (ABI) test, and it involves comparing the blood pressure in your ankle with the blood pressure in your arm, and expressing them as a ratio.
Here’s how to do it (instructions and a video demonstration if you want it):
Do Try This At Home: ABI Test For Clogged Arteries
If you need a blood pressure monitor, by the way, here’s an example product on Amazon.
- A healthy ABI score is between 1.0 and 1.4; anything outside this range may indicate arterial problems.
- Low ABI scores (below 0.8) suggest plaque is likely obstructing blood flow
- High ABI scores (above 1.4) may indicate artery hardening
Do note also that yes, if you have plaque obstructing blood flow and hardened arteries, your scores may cancel out and give you a “healthy” score, despite your arteries being very much not healthy.
For this reason, this test can be used to raise the alarm, but not to give the “all clear”.
There are other tests that clinicians can do for you, but you can’t do at home unless you have an MRI machine, a CT scanner, an x-ray machine, a doppler-and-ultrasound machine, etc. We’ll not go into those in detail here, but ask your doctor about them if you’re concerned.
What to do about it
In the mid-to-late stages of the disease, the options are medication and surgery, respectively, but your doctor will advise about those in that eventuality.
In the early stages of the disease, the first-line recommend treatment is exercise, of which, especially walking:
Lower Extremity Peripheral Artery Disease: Diagnosis and Treatment
Given that this more often happens when someone hasn’t been walking so much, it can be a walk-rest-walk approach at first (a treadmill on a low setting can be very useful for this):
See also: Exercise Comparison Head-to-Head: Treadmill vs Road
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
6 Signs Of Stroke (One Month In Advance)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most people can recognise the signs of a stroke when it’s just happened, but knowing the signs that appear a month beforehand would be very useful. That’s what this video’s about!
The Warning Signs
- Persistently elevated blood pressure: one more reason to have an at-home testing kit and use it regularly! Or a smartwatch or similar that’ll do it for you. The reason this is relevant is because high blood pressure can lead to damaging blood vessels, causing a stroke.
- Excessive fatigue: of course, this one can have many possible causes, but one of them is a “transient ischemic attack” (TIA), which is essentially a micro-stroke, and can be a precursor to a more severe stroke. So, we’re not doing the Google MD thing here of saying “if this, then that”, but we are saying: paying attention to the overall patterns can be very useful. Rather than fretting unduly about a symptom in isolation, see how it fits into the big picture.
- Vision problems: especially if sudden-onset with no obvious alternative cause can be a sign of neural damage, and may indicate a stroke on the way.
- Speech problems: if there’s not an obvious alternative explanation (e.g. you’ve just finished your third martini, or was this the fourth?), then speech problems (e.g. slurred speech, trouble forming sentences, etc) are a very worrying indicator and should be treated as a medical emergency.
- Neurological problems: a bit of a catch-all category, but memory issues, loss of balance, nausea without an obvious alternative cause, are all things that should get checked out immediately just in case.
- Numbness or weakness in the extremities: especially if on one side of the body only, is often caused by the TIA we mentioned earlier. If it’s both sides, then peripheral neuropathy may be the culprit, but having a neurologist take a look at it is a good idea either way.
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Two Things You Can Do To Improve Stroke Survival Chances
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Broccoli Sprouts & Sulforaphane
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝How much science is there behind sulforaphane / broccoli spirits and its health claims??❞
So, first of all, what it is: sulforaphane is a compound found in Brassica oleracea, of which species broccoli is a cultivar. It’s found in the other Brassica oleracea cultivars too (e.g. cauliflower, various cabbages, Brussels sprouts, kale, etc), but for whatever reason*, most research has been on broccoli and broccoli sprouts.
*Likely the reason is: research begets research—it’s easier to get funding to expand upon previous research, than it is to break ground on researching a different plant, where for the first third of your paper you have almost no existing scientific literature to cite. So once they got started on broccoli sprouts, everything else has been broccoli sprouts too.
And for clarity on what broccoli sprouts are: this means that when broccoli seeds have been germinated and just begun to sprout, they are harvested and eaten. That’s the one-line explanation, anyway; there’s a little more to it than that, so anyone interested should check out our previous main feature:
Good Things Come In Small Packages: Sprout Your Seeds, Grains, Beans, Etc
…and for more depth than we have room for in a one-page article, check out this book we reviewed:
The Sprout Book: Tap Into The Power Of The Planet’s Most Nutritious Food – by Doug Evans
One thing that the science is clear on: sprouts of a given plant indeed have much higher general nutritional density than their “adult” siblings. And in the case of sulforaphane specifically, it’s about 100x higher in broccoli sprouts than in adult broccoli:
Broccoli or Sulforaphane: Is It the Source or Dose That Matters? ← we suggest skipping down to the section “broccoli-based clinical trials”
So, that prompts the next question: do we care?
In other words: is sulforaphane really particularly important?
Sulforaphane vs cancer
The most well-evidenced health-giving property of sulforaphane is its anticancer activity:
Brassicaceae-Derived Anticancer Agents: Towards a Green Approach to Beat Cancer
A lot of the research there is epidemiological rather than RCTs, and where there are RCTs, they are mostly small ones, like this 10-person broccoli soup study about bioavailability (rather than the effects themselves):
Bioavailability of Glucoraphanin and Sulforaphane from High-Glucoraphanin Broccoli
To get into sulforaphane’s anticancer potential in seriousness, we have to look at a lot of in-vitro studies trialling it to limit carcinogenesis, or to shrink tumors with it, or specifically targetting cancer stem cells with it, which make for quite compelling reading:
A quick aside: if you’re reading that and thinking “Why is sonic the hedgehog in here?” it’s because after the observation of the influence of certain genes that influence cuticular denticles (the growth of spikes) on fruit fly larvae (bearing in mind the fruit fly Drosophila melanogaster is used for so much first- or second-line genetic research, being either the go-to or the go-to after the nematode C. elegans) caused the whole group of genes to get called “hedgehog genes” and then it became scientific convention to name each newly researched gene in that set after a different kind of hedgehog. One of them, instead of being named after a real-world hedgehog species like the others, got named after the videogame character.
Unfortunately, this now means that because the gene is associated with a certain congenital brain disorder, sometimes a doctor has to explain to a family that the reason their baby has a brain defect is because of a mutated sonic hedgehog.
Ok, back to talking about cancer. Let’s just quickly drop a few more papers so it’s clear that this is well-established:
- Multi-targeted prevention of cancer by sulforaphane ← this shows how it works on the cellular level
- Cruciferous vegetables: dietary phytochemicals for cancer prevention ← this shows how it works on the population level
However, that’s not the only established benefit:
❝SFN has other beneficial effects in addition to cancer protection. SFN exhibits neuroprotective effects and is implemented in treating conditions such as traumatic brain injury, Alzheimer’s disease and Parkinson’s disease.❞
Source: Sulforaphane in broccoli: The green chemoprevention!! Role in cancer prevention and therapy
Now, after the extract we quoted above, the rest of the section “other health benefits of sulforaphane” includes a lot of speculation, weak science, and/or things attributable to other phytochemicals in broccoli, including various polyphenols, vitamins, and minerals.
About those broccoli spirits
Ok, we know it was a typo, but… Actually, there is something worth mentioning here, and that’s that sulforaphane is only activated when glucoraphanin (its inactive form) comes into contact with myrosinase (an enzyme that’s only released when the plant is damaged).
In other words, it’s necessary to injure the broccoli before consuming it, in order to release the
spiritsmyrosinase. Now, while very few people are out there swallowing adult broccoli plants whole, it could well happen that people might wolf down uncut broccoli sprouts, since they are only small, after all.For this reason, it’s best that broccoli, even if it’s broccoli sprouts, be cut while raw before consumption.
In terms of cooking, heat in excess of 140℃ / 284℉ will destroy the glucoraphanin, and less/no glucoraphanin means less/no sulforaphane.
So, enjoying them raw or lightly steaming them seems to be best for this purpose:
Impact of thermal processing on sulforaphane yield from broccoli (Brassica oleracea L. ssp. italica)
Just want a supplement?
Many studies (including some cited by the research reviews we cited above) deal with sulforaphane in extract form, rather than whole plants, so there’s no shame in taking it that way if you’re not a fan of broccoli.
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: