To Nap Or Not To Nap; That Is The Question
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Is it good to nap in the afternoon, or better to get the famous 7 to 9 hours at night and leave it at that? I’m worried that daytime napping to make up for a shorter night’s sleep will just perpetuate and worsen it in the long run, is there a categorical answer here?❞
Generally considered best is indeed the 7–9 hours at night (yes, including at older ages):
Why You Probably Need More Sleep
…and sleep efficiency does matter too:
Why 7 Hours Sleep Is Not Enough
…which in turn, is influenced by factors other than just length and depth:
The 6 Dimensions Of Sleep (And Why They Matter)
However! Knowing what is best in theory does not help at all if it’s unattainable in practice. So, if you’re not getting a good night’s sleep (and we’ll assume you’re already practising good sleep hygiene; fresh bedding, lights-off by a certain time, no alcohol or caffeine before bed, that kind of thing), then a first port-of-call may be sleep remedies:
Safe Effective Sleep Aids For Seniors
If even those don’t work, then napping is now likely your best back-up option. But, napping done incorrectly can indeed cause as many problems as it solves. There’s a difference between:
- “I napped and now I have energy again” and you continue with your day
- “Darkness took me, and I strayed out of thought and time. Stars wheeled overhead, and every day was as long as the life age of the earth—but it was not the end.” and now you’re not sure whether it’s day or night, whose house you’re in, or whether you’ve been drugged.
These two very common napping experiences are influenced by factors that we can control:
How To Nap Like A Pro (No More “Sleep Hangovers”!)
If you still prefer to not risk napping but do need at least some kind of refreshment that’s actually a refreshment and not just taking stimulants, then you might consider this practice (from yoga nidra) that gives some of the same benefits of sleep, without actually sleeping:
Non-Sleep Deep Rest: A Neurobiologist’s Insights
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Castor Oil: All-Purpose Life-Changer, Or Snake Oil?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As “trending” health products go, castor oil is enjoying a lot of popularity presently, lauded as a life-changing miracle-worker, and social media is abuzz with advice to put it everywhere from your eyes to your vagina.
But:
- what things does science actually say it’s good for,
- what things lack evidence, and
- what things go into the category of “wow definitely do not do that”?
We don’t have the space to go into all of its proposed uses (there are simply far too many), but we’ll examine some common ones:
To heal/improve the skin barrier
Like most oils, it’s functional as a moisturizer. In particular, its high (90%!) ricinoleic fatty acid content does indeed make it good at that, and furthermore, has properties that can help reduce skin inflammation and promote wound healing:
Bioactive polymeric formulations for wound healing ← there isn’t a conveniently quotable summary we can just grab here, but you can see the data and results, from which we can conclude:
- formulations with ricinoleic acid (such as with castor oil) performed very well for topical anti-inflammatory purposes
- they avoided the unwanted side effects associated with some other contenders
- they consistently beat other preparations in the category of wound-healing
To support hair growth and scalp health
There is no evidence that it helps. We’d love to provide a citation for this, but it’s simply not there. There’s also no evidence that it doesn’t help. For whatever reason, despite its popularity, peer-reviewed science has simply not been done for this, or if it has, it wasn’t anywhere publicly accessible.
It’s possible that if a person is suffering hair loss specifically as a result of prostaglandin D2 levels, that ricinoleic acid will inhibit the PGD2, reversing the hair loss, but even this is hypothetical so far, as the science is currently only at the step before that:
However, due to some interesting chemistry, the combination of castor oil and warm water can result in acute (and irreversible) hair felting, in other words, the strands of hair suddenly glue together to become one mass which then has to be cut off:
“Castor Oil” – The Culprit of Acute Hair Felting
👆 this is a case study, which is generally considered a low standard of evidence (compared to high-quality Randomized Controlled Trials as the highest standard of evidence), but let’s just say, this writer (hi, it’s me) isn’t risking her butt-length hair on the off-chance, and doesn’t advise you to, either. There are other hair-oils out there; argan oil is great, coconut oil is totally fine too.
As a laxative
This time, there’s a lot of evidence, and it’s even approved for this purpose by the FDA, but it can be a bit too good, insofar as taking too much can result in diarrhea and uncomfortable cramping (the cramps are a feature not a bug; the mechanism of action is stimulatory, i.e. it gets the intestines squeezing, but again, it can result in doing that too much for comfort):
Castor Oil: FDA-Approved Indications
To soothe dry eyes
While putting oil in your eyes may seem dubious, this is another one where it actually works:
❝Castor oil is deemed safe and tolerable, with strong anti-microbial, anti-inflammatory, anti-nociceptive, analgesic, antioxidant, wound healing and vasoconstrictive properties.
These can supplement deficient physiological tear film lipids, enabling enhanced lipid spreading characteristics and reducing aqueous tear evaporation.
Studies reveal that castor oil applied topically to the ocular surface has a prolonged residence time, facilitating increased tear film lipid layer thickness, stability, improved ocular surface staining and symptoms.❞
Source: Therapeutic potential of castor oil in managing blepharitis, meibomian gland dysfunction and dry eye
Against candidiasis (thrush)
We couldn’t find science for (or against) castor oil’s use against vaginal candidiasis, but here’s a study that investigated its use against oral candidiasis:
…in which castor oil was the only preparation that didn’t work against the yeast.
Summary
We left a lot unsaid today (so many proposed uses, it feels like a shame to skip them), but in few words: it’s good for skin (including wound healing) and eyes; but we’d give it a miss for hair, candidiasis, and digestive disorders.
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Take care!
Share This Post
-
‘Disease X’: What it is (and isn’t)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- In January 2024, the World Economic Forum hosted an event called Preparing for Disease X to discuss strategies to improve international pandemic response.
- Disease X is a term used in epidemiology to refer to potential disease threats. It is not a real disease or a global conspiracy.
- Preparation to prevent and respond to future pandemics is a necessary part of global health to keep us all safer.
During the World Economic Forum’s 54th annual meeting in Davos, Switzerland, global health experts discussed ways to strengthen health care systems in preparation for future pandemics. Conspiracy theories quickly began circulating posts about the event and the fictional disease at its center, so-called Disease X.
What is Disease X?
In 2018, the World Health Organization added Disease X to its list of Blueprint Priority Diseases that are public health risks. But, unlike the other diseases on the list, Disease X doesn’t exist. The term represents a hypothetical human disease capable of causing a pandemic. Although experts don’t know what the next Disease X will be, they can make educated guesses about where and how it may emerge—and how we can prepare for it.
Why are we hearing about Disease X now?
COVID-19 has been the deadliest infectious disease outbreak of the 21st century. It’s also an example of a Disease X: a previously unknown pathogen that spreads rapidly around the world, claiming millions of lives.
When the WEF hosted a panel of experts to discuss Disease X, it was the first exposure that many people had to a concept that global health experts have been discussing since 2018.
Even before the routine pandemic preparedness event took place, online conspiracy theorists began circulating false claims that those discussing and preparing for Disease X had sinister motives, underscoring how widespread distrust of global health entities has become in the wake of the COVID-19 pandemic.
Why does Disease X matter?
Epidemiologists use concepts like Disease X to plan for future outbreaks and avoid the mistakes of past outbreaks. The COVID-19 pandemic and the recent non-endemic outbreak of mpox highlight the importance of global coordination to efficiently prevent and respond to disease outbreaks.
Pandemics are inevitable, but the scale of their destruction doesn’t have to be. Major disease outbreaks are likely to become more frequent due to the impacts of climate change. Preparing for a pandemic now helps ensure that the world is better equipped to handle the next one.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
-
Broccoli Sprouts & Sulforaphane
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝How much science is there behind sulforaphane / broccoli spirits and its health claims??❞
So, first of all, what it is: sulforaphane is a compound found in Brassica oleracea, of which species broccoli is a cultivar. It’s found in the other Brassica oleracea cultivars too (e.g. cauliflower, various cabbages, Brussels sprouts, kale, etc), but for whatever reason*, most research has been on broccoli and broccoli sprouts.
*Likely the reason is: research begets research—it’s easier to get funding to expand upon previous research, than it is to break ground on researching a different plant, where for the first third of your paper you have almost no existing scientific literature to cite. So once they got started on broccoli sprouts, everything else has been broccoli sprouts too.
And for clarity on what broccoli sprouts are: this means that when broccoli seeds have been germinated and just begun to sprout, they are harvested and eaten. That’s the one-line explanation, anyway; there’s a little more to it than that, so anyone interested should check out our previous main feature:
Good Things Come In Small Packages: Sprout Your Seeds, Grains, Beans, Etc
…and for more depth than we have room for in a one-page article, check out this book we reviewed:
The Sprout Book: Tap Into The Power Of The Planet’s Most Nutritious Food – by Doug Evans
One thing that the science is clear on: sprouts of a given plant indeed have much higher general nutritional density than their “adult” siblings. And in the case of sulforaphane specifically, it’s about 100x higher in broccoli sprouts than in adult broccoli:
Broccoli or Sulforaphane: Is It the Source or Dose That Matters? ← we suggest skipping down to the section “broccoli-based clinical trials”
So, that prompts the next question: do we care?
In other words: is sulforaphane really particularly important?
Sulforaphane vs cancer
The most well-evidenced health-giving property of sulforaphane is its anticancer activity:
Brassicaceae-Derived Anticancer Agents: Towards a Green Approach to Beat Cancer
A lot of the research there is epidemiological rather than RCTs, and where there are RCTs, they are mostly small ones, like this 10-person broccoli soup study about bioavailability (rather than the effects themselves):
Bioavailability of Glucoraphanin and Sulforaphane from High-Glucoraphanin Broccoli
To get into sulforaphane’s anticancer potential in seriousness, we have to look at a lot of in-vitro studies trialling it to limit carcinogenesis, or to shrink tumors with it, or specifically targetting cancer stem cells with it, which make for quite compelling reading:
A quick aside: if you’re reading that and thinking “Why is sonic the hedgehog in here?” it’s because after the observation of the influence of certain genes that influence cuticular denticles (the growth of spikes) on fruit fly larvae (bearing in mind the fruit fly Drosophila melanogaster is used for so much first- or second-line genetic research, being either the go-to or the go-to after the nematode C. elegans) caused the whole group of genes to get called “hedgehog genes” and then it became scientific convention to name each newly researched gene in that set after a different kind of hedgehog. One of them, instead of being named after a real-world hedgehog species like the others, got named after the videogame character.
Unfortunately, this now means that because the gene is associated with a certain congenital brain disorder, sometimes a doctor has to explain to a family that the reason their baby has a brain defect is because of a mutated sonic hedgehog.
Ok, back to talking about cancer. Let’s just quickly drop a few more papers so it’s clear that this is well-established:
- Multi-targeted prevention of cancer by sulforaphane ← this shows how it works on the cellular level
- Cruciferous vegetables: dietary phytochemicals for cancer prevention ← this shows how it works on the population level
However, that’s not the only established benefit:
❝SFN has other beneficial effects in addition to cancer protection. SFN exhibits neuroprotective effects and is implemented in treating conditions such as traumatic brain injury, Alzheimer’s disease and Parkinson’s disease.❞
Source: Sulforaphane in broccoli: The green chemoprevention!! Role in cancer prevention and therapy
Now, after the extract we quoted above, the rest of the section “other health benefits of sulforaphane” includes a lot of speculation, weak science, and/or things attributable to other phytochemicals in broccoli, including various polyphenols, vitamins, and minerals.
About those broccoli spirits
Ok, we know it was a typo, but… Actually, there is something worth mentioning here, and that’s that sulforaphane is only activated when glucoraphanin (its inactive form) comes into contact with myrosinase (an enzyme that’s only released when the plant is damaged).
In other words, it’s necessary to injure the broccoli before consuming it, in order to release the
spiritsmyrosinase. Now, while very few people are out there swallowing adult broccoli plants whole, it could well happen that people might wolf down uncut broccoli sprouts, since they are only small, after all.For this reason, it’s best that broccoli, even if it’s broccoli sprouts, be cut while raw before consumption.
In terms of cooking, heat in excess of 140℃ / 284℉ will destroy the glucoraphanin, and less/no glucoraphanin means less/no sulforaphane.
So, enjoying them raw or lightly steaming them seems to be best for this purpose:
Impact of thermal processing on sulforaphane yield from broccoli (Brassica oleracea L. ssp. italica)
Just want a supplement?
Many studies (including some cited by the research reviews we cited above) deal with sulforaphane in extract form, rather than whole plants, so there’s no shame in taking it that way if you’re not a fan of broccoli.
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
Related Posts
-
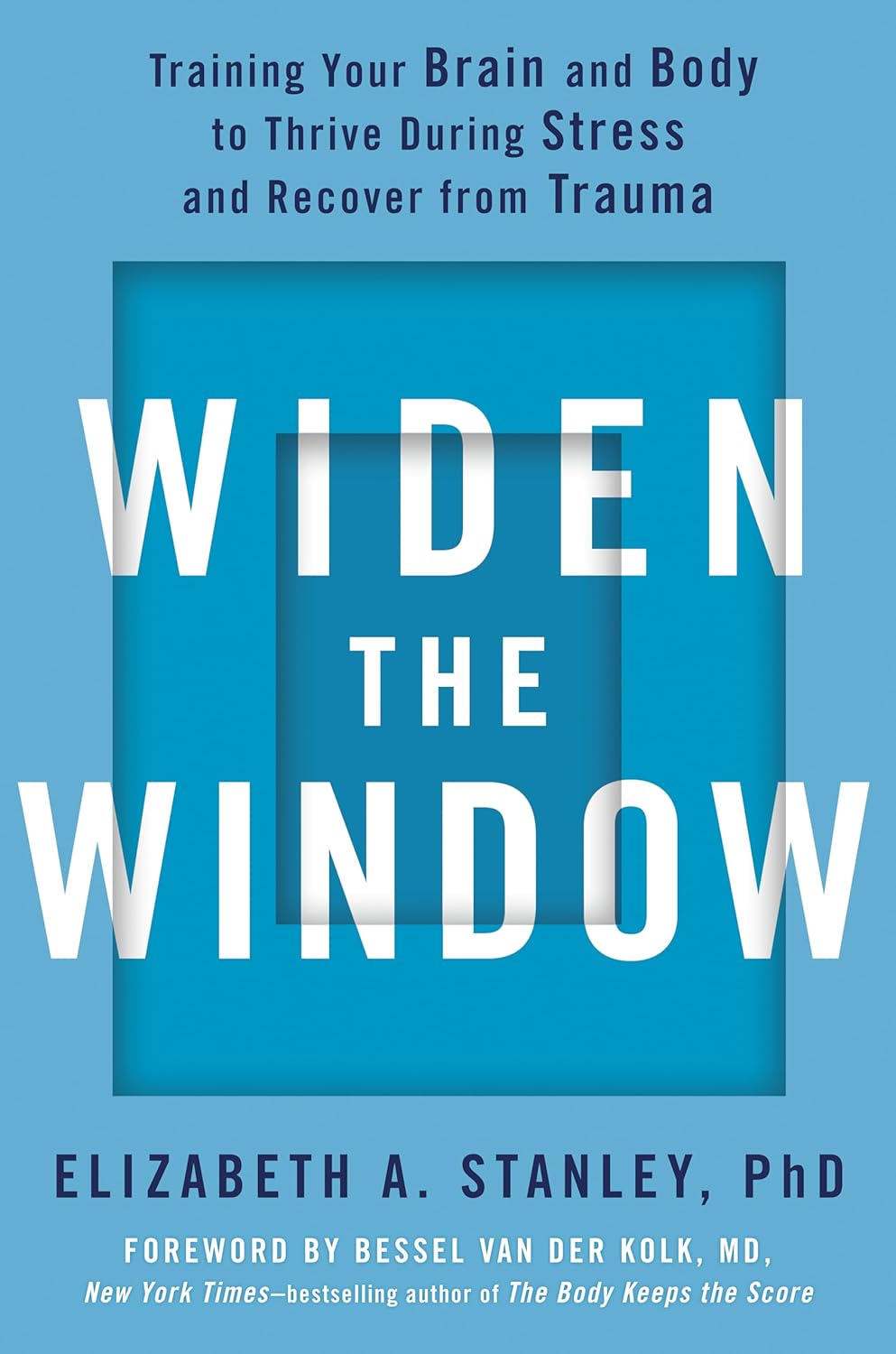
Widen the Window – by Dr. Elizabeth Stanley
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, about the title… That “window” that the author bids us “widen” is not a flowery metaphor, but rather, is referring to the window of exhibited resilience to stress/trauma; the “window” in question looks like an “inverted U” bell-curve on the graph.
In other words: Dr. Stanley’s main premise here is that we respond best to moderate stress (i.e: in that window, the area under the curve!), but if there is too little or too much, we don’t do so well. The key, she argues, is widening that middle part (expanding the area under the curve) in which we perform optimally. That way, we can still function in a motivated fashion without extrinsic threats, and we also don’t collapse under the weight of overwhelm, either.
The main strength of this book, however, lies in its practical exercises to accomplish that—and more.
“And more”, because the subtitle also promised recovery from trauma, and the author delivers in that regard too. In this case, it’s about widening that same window, but this time to allow one’s parasympathetic nervous system to recognize that the traumatic event is behind us, and no longer a threat; we are safe now.
Bottom line: if you would like to respond better to stress, and/or recover from trauma, this book is a very good tool.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Maximize Your Misery! (7 Great Methods)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s imagine that instead of being healthily fulfilled in life, you wanted to spend your days as miserable as possible. What should you do?
Here are a few pointers:
Stay still
Avoid physical activity and/or outdoor exposure, to avoid any mood-lifting neurochemicals. In fact, remain indoors as much as possible, preferably in the same room.
If you want to absolutely maximize your misery, make your bedroom the sole space for all activities that it’s possible to do there.
Disrupt your sleep
Keep an irregular sleep schedule by varying your bedtime and wake-up times frequently. Sleep in as much as possible, and make up for it by staying up late to ensure ongoing exhaustion.
Maximize screentime
Use digital entertainment as much as possible to distract you from meaningful activities and rest—as a bonus, this will also help you to avoid self-reflection.
Begin and end your day with a device in hand.
Fuel negative emotions
If you’re going to focus on something, focus on problems you cannot control, to stoke the fires of anger and angst.
A good way of doing this is by staying informed about distressing events, while avoiding meaningful actions to address them. Contribute only in token gestures, and then lament the lack of change.
Follow your impulses
Act on short-term desires without considering long-term consequences, while avoiding behaviors that you know might improve your mood or wellbeing.
Trust that doing the same things that have not previously resulted in happiness, will continue to reliably deliver unhappiness.
Set goals to miss
It’s important that your goals should be vague, and overly ambitious in their scope and/or deliverability. Ideally you should also disregard any preparatory work that a person would normally do before embarking on such a project.
Bonus tip: you can further sabotage any chances of progress, by waiting for motivation to strike before you take any action.
Pursue happiness
Focus on chasing happiness itself, instead of improving your situation or skills. Treat happiness as an end goal, instead of a by-product of worthwhile activities.
Want to learn more?
If you’d like to know many more ways to be miserable, we featured these 7 from this book of 40, which we haven’t reviewed yet, but probably will one of these days:
How to Be Miserable: 40 Strategies You Already Use – by Dr. Randy Paterson
Alternatively…
If for some strange reason you’d rather not do those things, you might consider a previous article of ours:
How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
10 Simple Japanese Habits For Healthier & Longer Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You don’t have to be Japanese or live in Okinawa to enjoy the benefits of healthy longevity. A lot of it comes down to simple habits:
Easy to implement
We’ll not keep the 10 habits a mystery; they are:
- Start the day with hot water: drinking hot water in the morning helps with hydration, warming the body, and aiding digestion.
- Enjoy a hearty breakfast: Japanese breakfasts are traditionally filling, nutritious, and help promote energy and longevity. Typical components include rice, miso soup, fish, and pickles.
- Take balanced meals: Japanese education emphasizes nutrition from a young age, promoting balanced meals with proteins, fiber, and vitamins & minerals.
- Enjoy fermented foods: fermented foods, such as nattō and soy-based condiments, support digestion, heart health, and the immune system.
- Drink green tea and matcha: both are rich in health benefits; preparing matcha mindfully adds a peaceful ritual to daily life too.
- Keep the “80% full” rule: “hara hachi bu” encourages eating until 80% full, which can improve longevity and, of course, prevent overeating.
- Use multiple small dishes: small servings and a variety of dishes help prevent overeating and ensure a diverse intake of nutrients.
- Gratitude before and after meals: saying “itadakimasu” and “gochisousama” promotes mindful eating, and afterwards, good digestion. Speaking Japanese is of course not the key factor here, but rather, do give yourself a moment of reflection before and after meals.
- Use vinegar in cooking: vinegar, often used in sushi rice and sauces like ponzu, adds flavor and offers health benefits, mostly pertaining to blood sugar balance.
- Eat slowly: Eating at a slower pace will improve digestion, and can enhance satiety and prevent accidentally overeating.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Get More Out Of What’s On Your Plate
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: