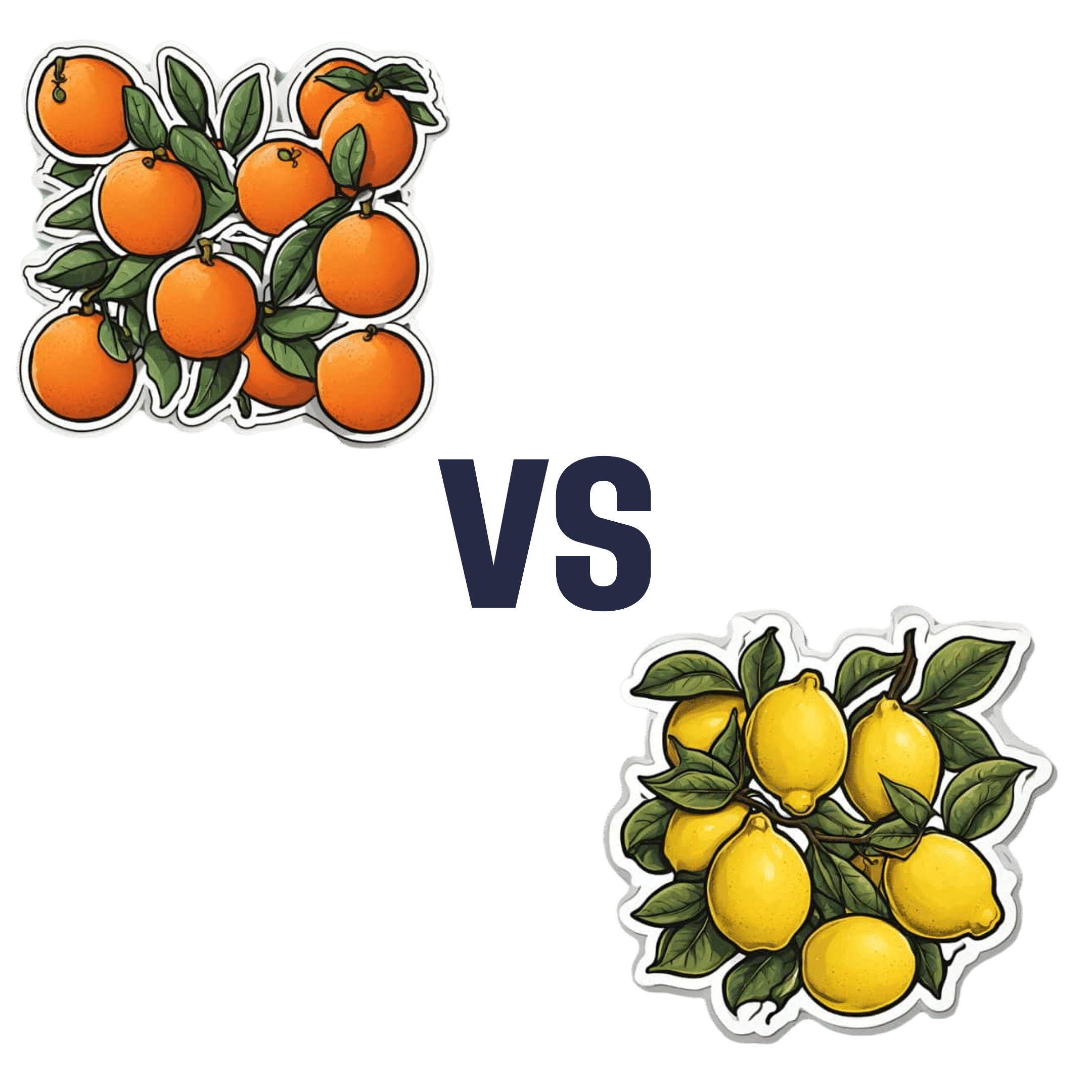
Oranges vs Lemons – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing oranges to lemons, we picked the oranges.
Why?
In the battle of these popular citrus fruits, there is a clear winner on the nutritional front.
Things were initially promising for lemons when looking at the macros—lemons have a little more fiber while oranges are slightly higher in carbs, but the differences are small and both are very healthy in this regard.
However, alas for this writer who prefers sour fruits to sweet ones (I’m sweet enough already), the micronutrient profiles tell a different story:
In terms of vitamins, oranges have more of vitamins A, B1, B2, B3, B5, B9, E, and choline. In contrast, lemons have a (very) little more vitamin B6. You might be wondering about vitamin C, since both fruits are famous for that—they’re equal on vitamin C. But, with that stack we listed above, oranges clearly win the vitamin category easily.
As for minerals, oranges boast more calcium, copper, magnesium, potassium, selenium, and zinc, while lemons have more iron, manganese, and phosphorus.
Technically lemons also have more sodium, but the numbers are truly miniscule (by coincidence, we discover upon grabbing a calculator, you’d need to eat approximately your own bodyweight in whole lemons to get to the RDA of sodium—and that’s to reach the RDA, not the upper healthy limit) so we’ll overlook the tiny sodium difference as irrelevant. Which means, while closer than the vitamins category, oranges win on minerals with a 6:3 lead over lemons.
Both fruits offer generous helpings of flavonoids and other polyphenols such as naringenin and hesperidin, which have anti-inflammatory properties and more specifically can also reduce allergy symptoms (unless, of course, you are allergic to citrus fruits, which is a relatively rare but extant allergy).
In short: as ever, enjoy both; diversity is great for the health. But if you want to maximize the nutrients you get, it’s oranges.
Want to learn more?
You might like to read:
Lemons vs Limes – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Rest For The Restless (Legs)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Any tips for dealing with restless legs syndrome?❞
As a neurological disorder (Willis-Ekbom Disease, as it is also called
by almost nobody outside of academia), there’s a lot that’s not known about its pathology, but we do know that looking after one’s nerves can help a lot.This means:
- Avoid alcohol, as this is bad for everything, including nerves
- See also: How To Reduce Or Quit Alcohol
- Don’t smoke, as this is bad for everything, including nerves
- Do exercise those restless legs! It may sound funny, but in seriousness, movement promotes nerve health
- See also: Walking… Better.
- Take care of your blood sugars, because diabetic neuropathy can also cause this
- See also: 10 Ways To Balance Blood Sugars
- Massage your legs, and enjoy a hot bath/shower
You can also take into account the measures recommended for dealing with peripheral neuropathy, e.g:
Peripheral Neuropathy: How To Avoid It, Manage It, Treat It
There are also medication options for RLS; most of them are dopamine agonists, so if you want to try something yourself before going the pharmaceutical route, then things that improve your dopamine levels will probably be a worth checking out. In the category of supplements, you might enjoy:
NALT: The Dopamine Precursor And More
Take care! And… Want something answered here? Send us your questions!
Share This Post
- Avoid alcohol, as this is bad for everything, including nerves
-
Tuna vs Catfish – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing tuna to catfish, we picked the tuna.
Why?
Today in “that which is more expensive and/or harder to get is not necessarily healthier”…
Looking at their macros, tuna has more protein and less fat (and overall, less saturated fat, and also less cholesterol).
In the category of vitamins, both are good but tuna distinguishes itself: tuna has more of vitamins A, B1, B2, B3, B6, and D, while catfish has more of vitamins B5, B9, B12, E, and K. They are both approximately equal in choline, and as an extra note in tuna’s favor (already winning 6:5), tuna is a very good source of vitamin D, while catfish barely contains any. All in all: a moderate, but convincing, win for tuna.
When it comes to minerals, things are clearer still: tuna has more copper, iron, magnesium, phosphorus, potassium, and selenium, while catfish has more calcium, manganese, and zinc. Oh, and catfish is also higher in one other mineral: sodium, which most people in industrialized countries need less of, on average. So, a 6:3 win for tuna, before we even take into account the sodium content (which makes the win for tuna even stronger).
In short: tuna wins the day in every category!
Want to learn more?
You might like to read:
Farmed Fish vs Wild Caught (It Makes Quite A Difference)
Take care!
Share This Post
-
Breathe; Don’t Vent (At Least In The Moment)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Zen And The Art Of Breaking Things
We’ve talked before about identifying emotions and the importance of being able to express them:
Answering The Most Difficult Question: How Are You?
However, there can be a difference between “expressing how we feel” and “being possessed by how we feel and bulldozing everything in our path”
…which is, of course, primarily a problem in the case of anger—and by extension, emotions that are often contemporaneous with anger, such as jealousy, shame, fear, etc.
How much feeling is too much?
While this is in large part a subjective matter, clinically speaking the key question is generally: is it adversely affecting daily life to the point of being a problem?
For example, if you have to spend half an hour every day actively managing a certain emotion, that’s probably indicative of something unusual, but “unusual” is not inherently bad. If you’re managing it safely and in a way that doesn’t negatively affect the rest of your life, then that is generally considered fine, unless you feel otherwise about it.
A good example of this is complicated grief and/or prolonged grief.
But what about when it comes to anger? How much is ok?
When it comes to those around you, any amount of anger can seem like too much. Anger often makes us short-tempered even with people who are not the object of our anger, and it rarely brings out the best in us.
We can express our feelings in non-aggressive ways, for example:
and
Seriously Useful Communication Skills!
Sometimes, there’s another way though…
Breathe; don’t vent
That’s a great headline, but we can’t take the credit for it, because it came from:
Breathe, don’t vent: turning down the heat is key to managing anger
…in which it was found that, by all available metrics, the popular wisdom of “getting it off your chest” doesn’t necessarily stand up to scrutiny, at least in the short term:
❝The work was inspired in part by the rising popularity of rage rooms that promote smashing things (such as glass, plates and electronics) to work through angry feelings.
I wanted to debunk the whole theory of expressing anger as a way of coping with it,” she said. “We wanted to show that reducing arousal, and actually the physiological aspect of it, is really important.❞
And indeed, he and his team did find that various arousal-increasing activities (such as hitting a punchbag, breaking things, doing vigorous exercise) did not help as much as arousal-decreasing activities, such as mindfulness-based relaxation techniques.
If you’d like to read the full paper, then so would we, but we couldn’t get full access to this one yet. However, the abstract includes representative statistics, so that’s worth a once-over:
Caveat!
Did you notice the small gap between their results and their conclusion?
In a lab or similar short-term observational setting, their recommendation is clearly correct.
However, if the source of your anger is something chronic and persistent, it could well be that calming down without addressing the actual cause is just “kicking the can down the road”, and will still have to actually be dealt with eventually.
So, while “here be science”, it’s not a mandate for necessarily suffering in silence. It’s more about being mindful about how we go about tackling our anger.
As for a primer on mindfulness, feel free to check out:
No-Frills, Evidence-Based Mindfulness
Take care!
Share This Post
Related Posts
-
Can Home Tests Replace Check-Ups?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I recently hit 65 and try to get regular check-ups, but do you think home testing can be as reliable as a doctor visit? I try to keep as informed as I can and am a big believer in taking responsibility for my own health if I can, but I don’t want to miss something important either. Best as a supplemental thing, perhaps?❞
Depends what’s being tested! And your level of technical knowledge, though there’s always something to be said for ongoing learning.
- If you’re talking blood tests, urine tests, etc per at-home test kits that get sent off to a lab, then provided they’re well-sourced (and executed correctly by you), they should be as accurate as what a doctor will give, since they are basically doing the same thing (taking a sample and sending it off to a lab).
- If you’re talking about checking for lumps etc, then a dual approach is best: check yourself at home as often as you feel is reasonable (with once per month being advised at a minimum, especially if you’re aware of an extra risk factor for you) and check-ups with the doctor per their recommendations.
- If you’re talking about general vitals (blood pressure, heart rate, heart rate variability, VO₂ max, etc), then provided you have a reliable way of testing them, then doing them very frequently at home, to get the best “big picture” view. In contrast, getting them done once a year at your doctor’s could result in a misleading result, if you just ate something different that day or had a stressful morning, for example.
Enjoy
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Truth About Statins – by Barbara H. Roberts, M.D.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
All too often, doctors looking to dispense a “quick fix” will prescribe from their playbook of a dozen or so “this will get you out of my office” drugs. Most commonly, things that treat symptoms rather than the cause. Sometimes, this can be fine! For example, in some cases, painkillers and antidepressants can make a big improvement to people’s lives. What about statins, though?
Prescribed to lower cholesterol, they broadly do exactly that. However…
Dr. Roberts wants us to know that we could be missing the big picture of heart health, and making a potentially fatal mistake.
This is not to say that the book argues that statins are necessarily terrible, or that they don’t have their place. Just, we need to understand what they will and won’t do, and make an informed choice.
To which end, she does advise regards when statins can help the most, and when they may not help at all. She also covers the questions to ask if your doctor wants to prescribe them. And—all so frequently overlooked—the important differences between men’s and women’s heart health, and the implications these have for the efficacy (or not) of statins.
With regard to the “alternatives to cholesterol-lowering drugs” promised in the subtitle… we won’t keep any secrets here:
Dr. Roberts (uncontroversially) recommends the Mediterranean diet. She also provides two weeks’ worth of recipes for such, in the final part of the book.
All in all, an important book to read if you or a loved one are taking, or thinking of taking, statins.
Pick up your copy of The Truth About Statins on Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ageless – by Dr. Andrew Steele
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So, yet another book with “The new science of…” in the title; does this one deliver new science?
Actually, yes, this time! The author was originally a physicist before deciding that aging was the number one problem that needed solving, and switched tracks to computational biology, and pioneered a lot of research, some of the fruits of which can be found in this book, in amongst a more general history of the (very young!) field of biogerontology.
Downside: most of this is not very practical for the lay reader; most of it is explanations of how things happen on a cellular and/or genetic level, and how we learned that. A lot also pertains to what we can learn from animals that either age very slowly, or are biologically immortal (in other words, they can still be killed, but they don’t age and won’t die of anything age-related), or are immune to cancer—and how we might borrow those genes for gene therapy.
However, there are also chapters on such things as “running repairs”, “reprogramming aging”, and “how to live long enough to live even longer”.
The style is conversational pop science; in the prose, he simply states things without reference, but at the back, there are 40 pages of bibliography, indexed in the order in which they occurred and prefaced with the statement that he’s referencing in each case. It’s an odd way to do citations, but it works comfortably enough.
Bottom line: if you’d like to understand aging on the cellular level, and how we know what we know and what the likely future possibilities are, then this is a great book; it’s also simply very enjoyable to read, assuming you have an interest in the topic (as this reviewer does).
Click here to check out Ageless, and understand the science of getting older without getting old!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: