Meditations for Mortals – by Oliver Burkeman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed this author’s “Four Thousand Weeks”, but for those who might have used a lot of those four thousand weeks already, and would like to consider things within a smaller timeframe for now, this work is a 28-day daily reader.
Now, daily readers are usually 366 days, but the chapters here are not the single page chapters that 366-page daily readers usually have. So, expect to invest a little more time per day (say, about 6 pages for each daily chapter).
Burkeman does not start the way we might expect, by telling us to take the time to smell the roses. Instead, he starts by examining the mistakes that most of us make most of the time, often due to unexamined assumptions about the world and how it works. Simply put, we’ve often received bad lessons in life (usually not explicitly, but rather, from our environments), and it takes some unpacking first to deal with that.
Nor is the book systems-based, as many books that get filed under “time management” may be, but rather, is simply principles-based. This is a strength, because principles are a lot easier to keep to than systems.
The writing style is direct and conversational, and neither overly familiar nor overly academic. It strikes a very comfortably readable balance.
Bottom line: if you’d like to get the most out of your days, this book can definitely help improve things a lot.
Click here to check out Meditations For Mortals, and live fulfilling days!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Prevent And Reverse Type 2 Diabetes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
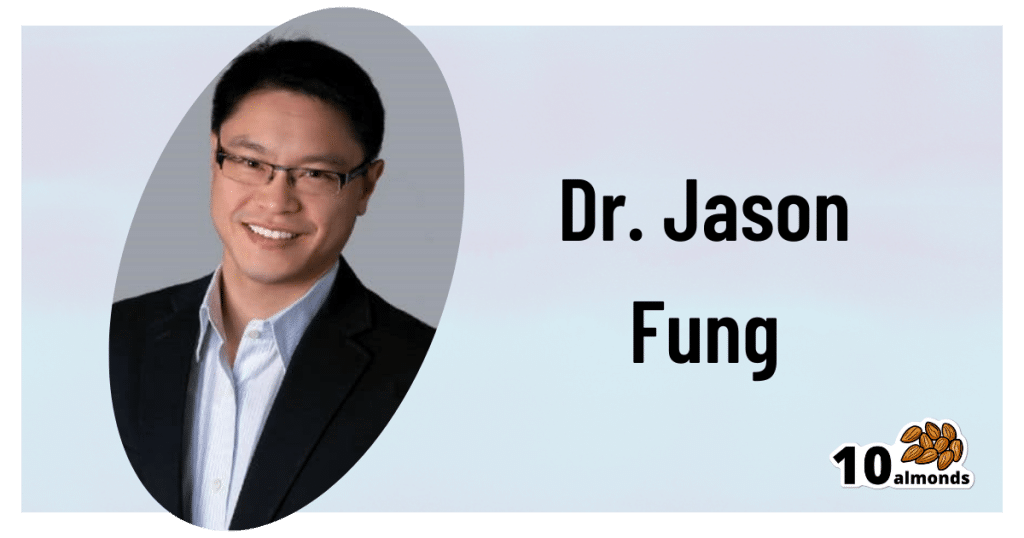
Turn back the clock on insulin resistance
This is Dr. Jason Fung. He’s a world-leading expert on intermittent fasting and low carbohydrate approaches to diet. He also co-founded the Intensive Dietary Management Program, later rebranded to the snappier title: The Fasting Method, a program to help people lose weight and reverse type 2 diabetes. Dr. Fung is certified with the Institute for Functional Medicine, for providing functional medicine certification along with educational programs directly accredited by the Accreditation Council for Continuing Medical Education (ACCME).
Why Intermittent Fasting?
Intermittent fasting is a well-established, well-evidenced, healthful practice for most people. In the case of diabetes, it becomes complicated, because if one’s blood sugars are too low during a fasting period, it will need correcting, thus breaking the fast.
Note: this is about preventing and reversing type 2 diabetes. Type 1 is very different, and sadly cannot be prevented or reversed in this fashion.
However, these ideas may still be useful if you have T1D, as you have an even greater need to avoid developing insulin resistance; you obviously don’t want your exogenous insulin to stop working.
Nevertheless, please do confer with your endocrinologist before changing your dietary habits, as they will know your personal physiology and circumstances in ways that we (and Dr. Fung) don’t.
In the case of having type 2 diabetes, again, please still check with your doctor, but the stakes are a lot lower for you, and you will probably be able to fast without incident, depending on your diet itself (more on this later).
Intermittent Fasting can be extra helpful for the body in the case of type 2 diabetes, as it helps give the body a rest from high insulin levels, thus allowing the body to become gradually re-sensitised to insulin.
Why low carbohydrate?
Carbohydrates, especially sugars, especially fructose*, cause excess sugar to be quickly processed by the liver and stored there. When the body’s ability to store glycogen is exceeded, the liver stores energy as fat instead. The resultant fatty liver is a major contributor to insulin resistance, when the liver can’t keep up with the demand; the blood becomes spiked full of unprocessed sugars, and the pancreas must work overtime to produce more and more insulin to deal with that—until the body starts becoming desensitized to insulin. In other words, type 2 diabetes.
There are other factors that affect whether we get type 2 diabetes, for example a genetic predisposition. But, our carb intake is something we can control, so it’s something that Dr. Fung focuses on.
*A word on fructose: actual fruits are usually diabetes-neutral or a net positive due to their fiber and polyphenols.
Fructose as an added ingredient, however, not so much. That stuff zips straight into your veins with nothing to slow it down and nothing to mitigate it.
The advice from Dr. Fung is simple here: cut the carbs. If you are already diabetic and do this with no preparation, you will probably simply suffer hypoglycemia, so instead:
- Enjoy a fibrous starter (a salad, some fruit, or perhaps some nuts)
- Load up with protein first, during your main meal—this will start to trigger your feelings of satedness
- Eat carbs last (preferably whole, unprocessed carbohydrates), and stop eating when 80% full.
Adapting Intermittent Fasting to diabetes
Dr. Fung advocates for starting small, and gradually increasing your fasting period, until, ideally, fasting 16 hours per day. You probably won’t be able to do this immediately, and that’s fine.
You also probably won’t be able to do this, if you don’t also make the dietary adjustments that help to give your liver a break, and thus by knock-on-effect, give your pancreas a break too.
With the dietary adjustments too, however, your insulin production-and-response will start to return to its pre-diabetic state, and finally its healthy state, after which, it’s just a matter of maintenance.
Want to hear more from Dr. Fung?
You may enjoy his blog, and for those who like videos, here is his YouTube channel:
Share This Post
-
Tell Yourself a Better Lie – by Marissa Peer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As humans, we generally lie to ourselves constantly. Or perhaps we really believe some of the things we tell ourselves, even if they’re not objectively necessarily true:
- I’ll always be poor
- I’m destined to be alone
- I don’t deserve good things
- Etc.
Superficially, it’s easy to flip those, and choose to tell oneself the opposite. But it feels hollow and fake, doesn’t it? That’s where Marissa Peer comes in.
Our stories that we tell ourselves don’t start where we are—they’re generally informed by things we learned along the way. Sometimes good lessons, sometimes bad ones. Sometimes things that were absolutely wrong and/or counterproductive.
Peer invites the reader to ask “What if…”, unravel how the unhelpful lessons got wired into our brains in the first place, and then set about untangling them.
“Tell yourself a better lie” does not mean self-deceit. It means that we’re the authors of our own stories, so we might as well make them work for us. Many things in life are genuinely fixed; others are open to interpretation.
Sorting one from the other, and then treating them correctly in a way that’s helpful to us? That’s how we can stop hurting ourselves, and instead bring our own stories around to uplift and fortify us.
Get Your Copy of “Tell Yourself A Better Lie” on Amazon Today!
Share This Post
-
What Would a Second Trump Presidency Look Like for Health Care?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
On the presidential campaign trail, former President Donald Trump is, once again, promising to repeal and replace the Affordable Care Act — a nebulous goal that became one of his administration’s splashiest policy failures.
“We’re going to fight for much better health care than Obamacare. Obamacare is a catastrophe,” Trump said at a campaign stop in Iowa on Jan. 6.
The perplexing revival of one of Trump’s most politically damaging crusades comes at a time when the Obama-era health law is even more popular and widely used than it was in 2017, when Trump and congressional Republicans proved unable to pass their own plan to replace it. That failed effort was a big part of why Republicans lost control of the House of Representatives in the 2018 midterms.
Despite repeated promises, Trump never presented his own Obamacare replacement. And much of what Trump’s administration actually accomplished in health care has been reversed by the Biden administration.
Still, Trump secured some significant policy changes that remain in place today, including efforts to bring more transparency to prices charged by hospitals and paid by health insurers.
Trying to predict Trump’s priorities in a second term is even more difficult given that he frequently changes his positions on issues, sometimes multiple times.
The Trump campaign did not respond to a request for comment.
Perhaps Trump’s biggest achievement is something he rarely talks about on the campaign trail. His administration’s “Operation Warp Speed” managed to create, test, and bring to market a covid-19 vaccine in less than a year, far faster than even the most optimistic predictions.
Many of Trump’s supporters, though, don’t support — and some even vehemently oppose — covid vaccines.
Here is a recap of Trump’s health care record:
Public Health
Trump’s pandemic response dominates his overall record on health care.
More than 400,000 Americans died from covid over Trump’s last year in office. His travel bans and other efforts to prevent the global spread of the virus were ineffective, his administration was slower than other countries’ governments to develop a diagnostic test, and he publicly clashed with his own government’s health officials over the response.
Ahead of the 2020 election, Trump resumed large rallies and other public campaign events that many public health experts regarded as reckless in the face of a highly contagious, deadly virus. He personally flouted public health guidance after contracting covid himself and ending up hospitalized.
At the same time, despite what many saw as a politicization of public health by the White House, Trump signed a massive covid relief bill (after first threatening to veto it). He also presided over some of the largest boosts for the National Institutes of Health’s budget since the turn of the century. And the mRNA-based vaccines Operation Warp Speed helped develop were an astounding scientific breakthrough credited with helping save millions of lives while laying the groundwork for future shots to fight other diseases including cancer.
Abortion
Trump’s biggest contribution to abortion policy was indirect: He appointed three Supreme Court justices, who were instrumental in overturning the constitutional right to an abortion.
During his 2024 campaign, Trump has been all over the place on the red-hot issue. Since the Supreme Court overturned Roe v. Wade in 2022, Trump has bemoaned the issue as politically bad for Republicans; criticized one of his rivals, Florida Gov. Ron DeSantis, for signing a six-week abortion ban; and vowed to broker a compromise with “both sides” on abortion, promising that “for the first time in 52 years, you’ll have an issue that we can put behind us.”
He has so far avoided spelling out how he’d do that, or whether he’d support a national abortion ban after any number of weeks.
More recently, however, Trump appears to have mended fences over his criticism of Florida’s six-week ban and more with key abortion opponents, whose support helped him get elected in 2016 — and whom he repaid with a long list of policy changes during his presidency.
Among the anti-abortion actions taken by the Trump administration were a reinstatement of the “Mexico City Policy” that bars giving federal funds to international organizations that support abortion rights; a regulation to bar Planned Parenthood and other organizations that provide abortions from the federal family planning program, Title X; regulatory changes designed to make it easier for health care providers and employers to decline to participate in activities that violate their religious and moral beliefs; and other changes that made it harder for NIH scientists to conduct research using fetal tissue from elective abortions.
All of those policies have since been overturned by the Biden administration.
Health Insurance
Unlike Trump’s policies on reproductive health, many of his administration’s moves related to health insurance still stand.
For example, in 2020, Trump signed into law the No Surprises Act, a bipartisan measure aimed at protecting patients from unexpected medical bills stemming from payment disputes between health care providers and insurers. The bill was included in the $900 billion covid relief package he opposed before signing, though Trump had expressed support for ending surprise medical bills.
His administration also pushed — over the vehement objections of health industry officials — price transparency regulations that require hospitals to post prices and insurers to provide estimated costs for procedures. Those requirements also remain in place, although hospitals in particular have been slow to comply.
Medicaid
While first-time candidate Trump vowed not to cut popular entitlement programs like Medicare, Medicaid, and Social Security, his administration did not stick to that promise. The Affordable Care Act repeal legislation Trump supported in 2017 would have imposed major cuts to Medicaid, and his Department of Health and Human Services later encouraged states to require Medicaid recipients to prove they work in order to receive health insurance.
Drug Prices
One of the issues the Trump administration was most active on was reducing the price of prescription drugs for consumers — a top priority for both Democratic and Republican voters. But many of those proposals were blocked by the courts.
One Trump-era plan that never took effect would have pegged the price of some expensive drugs covered by Medicare to prices in other countries. Another would have required drug companies to include prices in their television advertisements.
A regulation allowing states to import cheaper drugs from Canada did take effect, in November 2020. However, it took until January 2024 for the FDA, under Trump’s successor, to approve the first importation plan, from Florida. Canada has said it won’t allow exports that risk causing drug shortages in that country, leaving unclear whether the policy is workable.
Trump also signed into law measures allowing pharmacists to disclose to patients when the cash price of a drug is lower than the cost using their insurance. Previously pharmacists could be barred from doing so under their contracts with insurers and pharmacy benefit managers.
Veterans’ Health
Trump is credited by some advocates for overhauling Department of Veterans Affairs health care. However, while he did sign a major bill allowing veterans to obtain care outside VA facilities, White House officials also tried to scuttle passage of the spending needed to pay for the initiative.
Medical Freedom
Trump scored a big win for the libertarian wing of the Republican Party when he signed into law the “Right to Try Act,” intended to make it easier for patients with terminal diseases to access drugs or treatments not yet approved by the FDA.
But it is not clear how many patients have managed to obtain treatment using the law because it is aimed at the FDA, which has traditionally granted requests for “compassionate use” of not-yet-approved drugs anyway. The stumbling block, which the law does not address, is getting drug companies to release doses of medicines that are still being tested and may be in short supply.
Trump said in a Jan. 10 Fox News town hall that the law had “saved thousands and thousands” of lives. There’s no evidence for the claim.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
How To Avoid Age-Related Macular Degeneration
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Avoiding Age-Related Macular Degeneration
Eye problems can strike at any age, but as we get older, it becomes a lot more likely. In particular, age-related macular degeneration is, as the name suggests, an age-bound disease.
Is there no escaping it, then?
The risk factors for age-related macular degeneration are as follows:
- Being over the age of 55 (can’t do much about this one)
- Being over the age of 65 (risk climbs sharply now)
- Having a genetic predisposition (can’t do much about this one)
- Having high cholesterol (this one we can tackle)
- Having cardiovascular disease (this one we can tackle)
- Smoking (so, just don’t)
Genes predispose; they don’t predetermine. Or to put it another way: genes load the gun, but lifestyle pulls the trigger.
Preventative interventions against age-related macular degeneration
Prevention is better than a cure in general, and this especially goes for things like age-related macular degeneration, because the most common form of it has no known cure.
So first, look after your heart (because your heart feeds your eyes).
See also: The Mediterranean Diet
Next, eat to feed your eyes specifically. There’s a lot of research to show that lutein helps avoid age-related diseases in the eyes and the rest of the brain, too:
See also: Brain Food? The Eyes Have It
Do supplements help?
They can! There was a multiple-part landmark study by the National Eye Institute, a formula was developed that reduced the 5-year risk of intermediate disease progressing to late disease by 25–30%. It also reduced the risk of vision loss by 19%.
You can read about both parts of the study here:
Age-Related Eye Disease Studies (AREDS/AREDS2): major findings
As you can see, an improvement was made between the initial study and the second one, by replacing beta-carotene with lutein and zeaxanthin.
The AREDS2 formula contains:
- 500 mg vitamin C
- 180 mg vitamin E
- 80 mg zinc
- 10 mg lutein
- 2 mg copper
You can learn more about these supplements, and where to get them, here on the NEI’s corner of the official NIH website:
AREDS 2 Supplements for Age-Related Macular Degeneration
Take care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Real Superfoods – by Ocean Robbins & Nichole Dandrea-Russert
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Of the two authors, the former is a professional public speaker, and the latter is a professional dietician. As a result, we get a book that is polished and well-presented, while actually having a core of good solid science (backed up with plenty of references).
The book is divided into two parts; the first part has 9 chapters pertaining to 9 categories of superfood (with more details about top-tier examples of each, within), and the second part has 143 pages of recipes.
And yes, as usual, a couple of the recipes are “granola” and “smoothie”, but when are they not? Most of the recipes are worthwhile, though, with a lot of good dishes that should please most people.
Bottom line: this is half pop-science presentation of superfoods, and half cookbook featuring those ingredients. Definitely a good way to increase your consumption of superfoods, and get the most out of your diet.
Click here to check out Real Superfoods, and power up your health!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Sun Exposure Dilemma
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Sun Exposure Dilemma
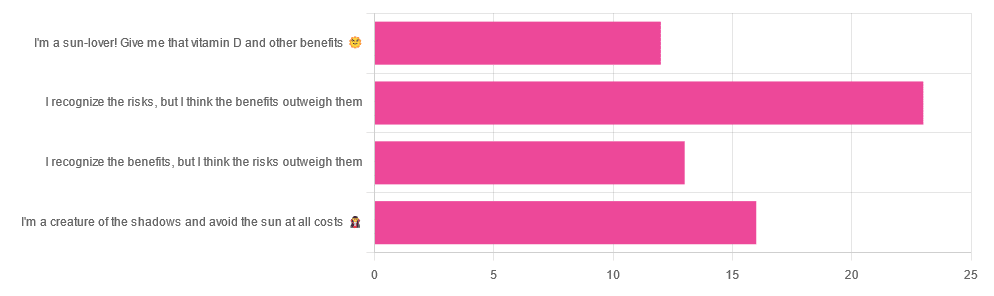
Yesterday, we asked you about your policy on sun exposure, and got the above-pictured, below-described, set of answers:
- A little over a third of respondents chose “I recognize the risks, but I think the benefits outweigh them”
- A quarter of respondents chose “I am a creature of the shadows and I avoid the sun at all costs”
- A little over a fifth of respondents chose “I recognize the benefits, but I think the risks outweigh them”
- A little under a fifth of respondents chose “I’m a sun-lover! Give me that vitamin D and other benefits!”
All in all, this is perhaps the most even spread of answers we’ve had for Friday mythbuster polls—though the sample size was smaller than it often is.
Of those who added comments, common themes were to mention your local climate, and the importance of sunscreen and/or taking vitamin D supplements.
One subscriber mentioned having lupus and living in Florida, which is a particularly unfortunate combination:
Lupus Foundation | Lupus & UV exposure: What you need to know
Another subscriber wrote:
❝Use a very good sunscreen with a high SPF all the time. Reapply after swimming or as needed! I also wear polarized sunglasses anytime I’m outside.❞
…which are important things to note too, and a lot of people forget!
See also: Who Screens The Sunscreens? (on fearing chemical dangers, vs the protection given)
But, onto today’s science for the topic at hand…
We need to get plenty of sun to get plenty of vitamin D: True or False?
True or False, depending on so many factors—to the point that many people get it wildly wrong in either direction.
Whether we are getting enough vitamin D depends on many circumstances, including:
- The climate (and depending on latitude, time of year) where we live
- Our genes, and especially (but not only) our skintone
- The clothes we wear (or don’t)
- Our diet (and not just “how much vitamin D do we consume”)
- Chronic diseases that affect vitamin D metabolism and/or requirements and/or sensitivity to the sun
For a rundown on these factors and more, check out:
Should I be getting my vitamin D levels checked?
Notably, on the topic of whether you should stay in the sun for longer to get more vitamin D…
❝The body can only produce a certain amount of vitamin D at the time, so staying in the sun any longer than needed (which could be just a few minutes, in a sunny climate) is not going to help increase your vitamin D levels, while it will increase your risk of skin cancer.❞
In contrast, she does also note:
❝During winter, catching enough sun can be difficult, especially if you spend your days confined indoors. Typically, the required exposure increases to two to three hours per week in winter. This is because sunlight exposure can only help produce vitamin D if the UVB rays reach us at the correct angle. So in winter we should regularly spend time outside in the middle of the day to get our dose of vitamin D.❞
See also: Vitamin D & Calcium: Too Much Of A Good Thing?
We can skip the sun and get our vitamin D from diet/supplements: True or False?
True! However, vitamin D is not the only health benefit of sun exposure.
Not only is sunlight-induced serotonin production important for many things ranging from mood to circadian rhythm (which in turn affects many other aspects of health), but also…
While too much sun can cause skin cancer, too little sun could cause other kinds of cancer:
Benefits of Sunlight: A Bright Spot for Human Health
Additionally, according to new research, the circadian rhythm benefits we mentioned above may also have an impact on type 2 diabetes:
Can catching some rays help you fight off type 2 diabetes?
Which way to jump?
A lot of it depends on who you are, ranging from the factors we mentioned earlier, to even such things as “having many moles” or “having blonde hair”.
This latter item, blonde hair, is a dual thing: it’s a matter of genetic factors that align with being prone to being more sensitive to the sun, as well as being a lesser physical barrier to the sun’s rays than dark hair (that can block some UV rays).
So for example, if two people have comparably gray hair now, but one of them used to have dark hair and the other blonde, there will still be a difference in how they suffer damage, or don’t—and yes, even if their skin is visually of the same approximate skintone.
You probably already know for yourself whether you are more likely to burn or tan in the sun, and the former group are less resistant to the sun’s damage… But the latter group are more likely to spend longer in the sun, and accumulate more damage that way.
If you’d like a very comprehensive downloadable, here are the guidelines issued by the UK’s National Institute for Health and Care Excellence:
NICE Guidelines | Sunlight exposure: risks and benefits
…and skip to “At risk groups”, if you don’t want to read the whole thing; “Skin type” is also an important subsection, which also uses your hair and eye color as indicators.
Writer’s note: genetics are complicated and not everyone will fall neatly into categories, which is why it’s important to know the individual factors.
For example, I am quite light-skinned with slightly graying dark hair and gray-blue eyes, and/but also have an obscure Sámi gene that means my skin makes vitamin D easily, while simultaneously being unusually resistant to burning (I just tan). Basically: built for the midnight sun of the Arctic circle.
And yet! My hobbies include not getting skin cancer, so I tend to still be quite mindful of UV levels in different weathers and times of day, and make choices (schedule, clothing, sunscreen or not) accordingly.
Bottom line:
That big self-perpetuating nuclear explosion in the sky is responsible for many things, good and bad for our health, so be aware of your own risk factors, especially for vitamin D deficiency, and skin cancer.
- If you have a predisposition to both, that’s unfortunate, but diet and supplementation at least can help with the vitamin D while getting modest amounts of sun at most.
- Remember that you can only make so much vitamin D at once, so sunbathing for health benefits need only take a few minutes
- Remember that sunlight is important for our circadian rhythm, which is important for many things.
- That’s governed by specific photoreceptor cells, though, so we don’t need our skin to be exposed for that; we just need to be able to see sunlight.
- If you’re going to be out in the sun, and not covered up, sunscreen is your friend, and yes, that goes for clear cold days under the winter sun too.
- Most phone weather apps these days have a UV index score as part of the data they give. Get used to checking it as often as you’d check for rain.
Stay safe, both ways around!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: