Is Marine Collagen Worth Taking?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Questions and Answers at 10almonds
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
I wanted to ask if you think marine collagen is decent to take. I’ve heard a lot of bad press about it
We don’t know what you’ve heard, but generally speaking it’s been found to be very beneficial to bones, joints, and skin! We wrote about it quite recently on a “Research Review Monday”:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How old’s too old to be a doctor? Why GPs and surgeons over 70 may need a health check to practise
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A growing number of complaints against older doctors has prompted the Medical Board of Australia to announce today that it’s reviewing how doctors aged 70 or older are regulated. Two new options are on the table.
The first would require doctors over 70 to undergo a detailed health assessment to determine their current and future “fitness to practise” in their particular area of medicine.
The second would require only general health checks for doctors over 70.
A third option acknowledges existing rules requiring doctors to maintain their health and competence. As part of their professional code of conduct, doctors must seek independent medical and psychological care to prevent harming themselves and their patients. So, this third option would maintain the status quo.
PeopleImages.com – Yuri A/Shutterstock Haven’t we moved on from set retirement ages?
It might be surprising that stricter oversight of older doctors’ performance is proposed now. Critics of mandatory retirement ages in other fields – for judges, for instance – have long questioned whether these rules are “still valid in a modern society”.
However, unlike judges, doctors are already required to renew their registration annually to practise. This allows the Medical Board of Australia not only to access sound data about the prevalence and activity of older practitioners, but to assess their eligibility regularly and to conduct performance assessments if and when they are needed.
What has prompted these proposals?
This latest proposal identifies several emerging concerns about older doctors. These are grounded in external research about the effect of age on doctors’ competence as well as the regulator’s internal data showing surges of complaints about older doctors in recent years.
Studies of medical competence in ageing doctors show variable results. However, the Medical Board of Australia’s consultation document emphasises studies of neurocognitive loss. It explains how physical and cognitive impairment can lead to poor record-keeping, improper prescribing, as well as disruptive behaviour.
The other issue is the number of patient complaints against older doctors. These “notifications” have surged in recent years, as have the number of disciplinary actions against older doctors.
In 2022–2023, the Medical Board of Australia took disciplinary action against older doctors about 1.7 times more often than for doctors under 70.
In 2023, notifications against doctors over 70 were 81% higher than for the under 70s. In that year, patients sent 485 notifications to the Medical Board of Australia about older doctors – up from 189 in 2015.
While older doctors make up only about 5.3% of the doctor workforce in Australia (less than 1% over 80), this only makes the high numbers of complaints more starkly disproportionate.
It’s for these reasons that the Medical Board of Australia has determined it should take further regulatory action to safeguard the health of patients.
So what distinguishes the two new proposed options?
The “fitness to practise” assessment option would entail a rigorous assessment of doctors over 70 based on their specialisation. It would be required every three years after the age of 70 and every year after 80.
Surgeons, for example, would be assessed by an independent occupational physician for dexterity, sight and the ability to give clinical instructions.
Importantly, the results of these assessments would usually be confidential between the assessor and the doctor. Only doctors who were found to pose a substantial risk to the public, which was not being managed, would be obliged to report their health condition to the Medical Board of Australia.
The second option would be a more general health check not linked to the doctor’s specific role. It would occur at the same intervals as the “fitness to practise” assessment. However, its purpose would be merely to promote good health-care decision-making among health practitioners. There would be no general obligation on a doctor to report the results to the Medical Board of Australia.
In practice, both of these proposals appear to allow doctors to manage their own general health confidentially.
Older surgeons could be independently assessed for dexterity, sight and the ability to give clinical instructions. worradirek/Shutterstock The law tends to prioritise patient safety
All state versions of the legal regime regulating doctors, known as the National Accreditation and Registration Scheme, include a “paramountcy” provision. That provision basically says patient safety is paramount and trumps all other considerations.
As with legal regimes regulating childcare, health practitioner regulation prioritises the health and safety of the person receiving the care over the rights of the licensed professional.
Complicating this further, is the fact that a longstanding principle of health practitioner regulation has been that doctors should not be “punished” for errors in practice.
All of this means that reforms of this nature can be difficult to introduce and that the balance between patient safety and professional entitlements must be handled with care.
Could these proposals amount to age discrimination?
It is premature to analyse the legal implications of these proposals. So it’s difficult to say how these proposals interact with Commonwealth age- and other anti-discrimination laws.
For instance, one complication is that the federal age discrimination statute includes an exemption to allow “qualifying bodies” such as the Medical Board of Australia to discriminate against older professionals who are “unable to carry out the inherent requirements of the profession, trade or occupation because of his or her age”.
In broader terms, a licence to practise medicine is often compared to a licence to drive or pilot an aircraft. Despite claims of discrimination, New South Wales law requires older drivers to undergo a medical assessment every year; and similar requirements affect older pilots and air traffic controllers.
Where to from here?
When changes are proposed to health practitioner regulation, there is typically much media attention followed by a consultation and behind-the-scenes negotiation process. This issue is no different.
How will doctors respond to the proposed changes? It’s too soon to say. If the proposals are implemented, it’s possible some older doctors might retire rather than undergo these mandatory health assessments. Some may argue that encouraging more older doctors to retire is precisely the point of these proposals. However, others have suggested this would only exacerbate shortages in the health-care workforce.
The proposals are open for public comment until October 4.
Christopher Rudge, Law lecturer, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Rethinking Diabetes – by Gary Taubes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed this author’s “The Case Against Sugar” and “Why We Get Fat And What To Do About It“. There’s an obvious theme, and this book caps it off nicely:
By looking at the history of diabetes treatment (types 1 and 2) in the past hundred years, and analysing the patterns over time, we can see how:
- diabetics have been misled a lot over time by healthcare providers
- we can learn from those mistakes going forwards
Happily, he does this without crystal-balling the future or expecting diet to fix, for example, a pancreas that can’t produce insulin. But what he does do is focus on the “can” items rather than the “can’t” items.
In the category of criticism, one of the strategies he argues for is basically the keto diet, which is indeed just fine for diabetes but often not great for the heart in the long-term (it depends on various factors, including genes). However, even if you choose not to implement that, there is plenty more to try out in this book.
Bottom line: whether you have diabetes, love someone who does, or just plain like to be on top of your glycemic health, this book is full of important insights and opportunities to improve things progressively along the way.
Click here to check out Rethinking Diabetes, and rethink diabetes!
Share This Post
-
What is ‘breathwork’? And do I need to do it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From “breathwork recipes” to breathing techniques, many social media and health websites are recommending breathwork to reduce stress.
But breathwork is not new. Rather it is the latest in a long history of breathing techniques such as Pranayama from India and qigong from China. Such practices have been used for thousands of years to promote a healthy mind and body.
The benefits can be immediate and obvious. Try taking a deep breath in through your nose and exhaling slowly. Do you feel a little calmer?
So, what’s the difference between the breathing we do to keep us alive and breathwork?
Taras Grebinets/Shutterstock Breathwork is about control
Breathwork is not the same as other mindfulness practices. While the latter focus on observing the breath, breathwork is about controlling inhalation and exhalation.
Normally, breathing happens automatically via messages from the brain, outside our conscious control. But we can control our breath, by directing the movement of our diaphragm and mouth.
The diaphragm is a large muscle that separates our thoracic (chest) and abdominal (belly) cavities. When the diaphragm contracts, it expands the thoracic cavity and pulls air into the lungs.
Controlling how deep, how often, how fast and through what (nose or mouth) we inhale is the crux of breathwork, from fire breathing to the humming bee breath.
Breathwork can calm or excite
Even small bits of breathwork can have physical and mental health benefits and complete the stress cycle to avoid burnout.
Calming breathwork includes diaphragmatic (belly) breathing, slow breathing, pausing between breaths, and specifically slowing down the exhale.
In diaphragmatic breathing, you consciously contract your diaphragm down into your abdomen to inhale. This pushes your belly outwards and makes your breathing deeper and slower.
You can also slow the breath by doing:
- box breathing (count to four for each of four steps: breathe in, hold, breathe out, hold), or
- coherent breathing (controlled slow breathing of five or six breaths per minute), or
- alternate nostril breathing (close the left nostril and breathe in slowly through the right nostril, then close the right nostril and breathe out slowly through the left nostril, then repeat the opposite way).
You can slow down the exhalation specifically by counting, humming or pursing your lips as you breathe out.
In contrast to these calming breathing practices, energising fast-paced breathwork increases arousal. For example, fire breathing (breathe in and out quickly, but not deeply, through your nose in a consistent rhythm) and Lion’s breath (breathe out through your mouth, stick your tongue out and make a strong “haa” sound).
What is happening in the body?
Deep and slow breathing, especially with a long exhale, is the best way to stimulate the vagus nerves. The vagus nerves pass through the diaphragm and are the main nerves of the parasympathetic nervous system.
Simulating the vagus nerves calms our sympathetic nervous system (fight or flight) stress response. This improves mood, lowers the stress hormone cortisol and helps to regulate emotions and responses. It also promotes more coordinated brain activity, improves immune function and reduces inflammation.
Taking deep, diaphragmatic breaths also has physical benefits. This improves blood flow, lung function and exercise performance, increases oxygen in the body, and strengthens the diaphragm.
Slow breathing reduces heart rate and blood pressure and increases heart rate variability (normal variation in time between heart beats). These are linked to better heart health.
Taking shallow, quick, rhythmic breaths in and out through your nose stimulates the sympathetic nervous system. Short-term, controlled activation of the stress response is healthy and develops resilience to stress.
Breathing in through the nose
We are designed to inhale through our nose, not our mouth. Inside our nose are lots of blood vessels, mucous glands and tiny hairs called cilia. These warm and humidify the air we breathe and filter out germs and toxins.
We want the air that reaches our airways and lungs to be clean and moist. Cold and dry air is irritating to our nose and throat, and we don’t want germs to get into the body.
Nasal breathing increases parasympathetic activity and releases nitric oxide, which improves airway dilation and lowers blood pressure.
Consistently breathing through our mouth is not healthy. It can lead to pollutants and infections reaching the lungs, snoring, sleep apnoea, and dental issues including cavities and jaw joint problems.
Breathing can be high and shallow when we are stressed. mi_viri/Shutterstock A free workout
Slow breathing – even short sessions at home – can reduce stress, anxiety and depression in the general population and among those with clinical depression or anxiety. Research on breathwork in helping post-traumatic stress disorder (PTSD) is also promising.
Diaphragmatic breathing to improve lung function and strengthen the diaphragm can improve breathing and exercise intolerance in chronic heart failure, chronic obstructive pulmonary disease and asthma. It can also improve exercise performance and reduce oxidative stress (an imbalance of more free radicals and/or less antioxidants, which can damage cells) after exercise.
Waiting at the lights? This could be your signal to do some breathwork. doublelee/Shutterstock A mind-body connection you can access any time
If you feel stressed or anxious, you might subconsciously take shallow, quick breaths, but this can make you feel more anxious. Deep diaphragmatic breaths through your nose and focusing on strong exhalations can help break this cycle and bring calm and mental clarity.
Just a few minutes a day of breathwork can improve your physical and mental health and wellbeing. Daily deep breathing exercises in the workplace reduce blood pressure and stress, which is important since burnout rates are high.
Bottom line: any conscious control of your breath throughout the day is positive.
So, next time you are waiting in a line, at traffic lights or for the kettle to boil, take a moment to focus on your breath. Breathe deeply into your belly through your nose, exhale slowly, and enjoy the benefits.
Theresa Larkin, Associate professor of Medical Sciences, University of Wollongong and Judy Pickard, Senior Lecturer, Clinical Psychology, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
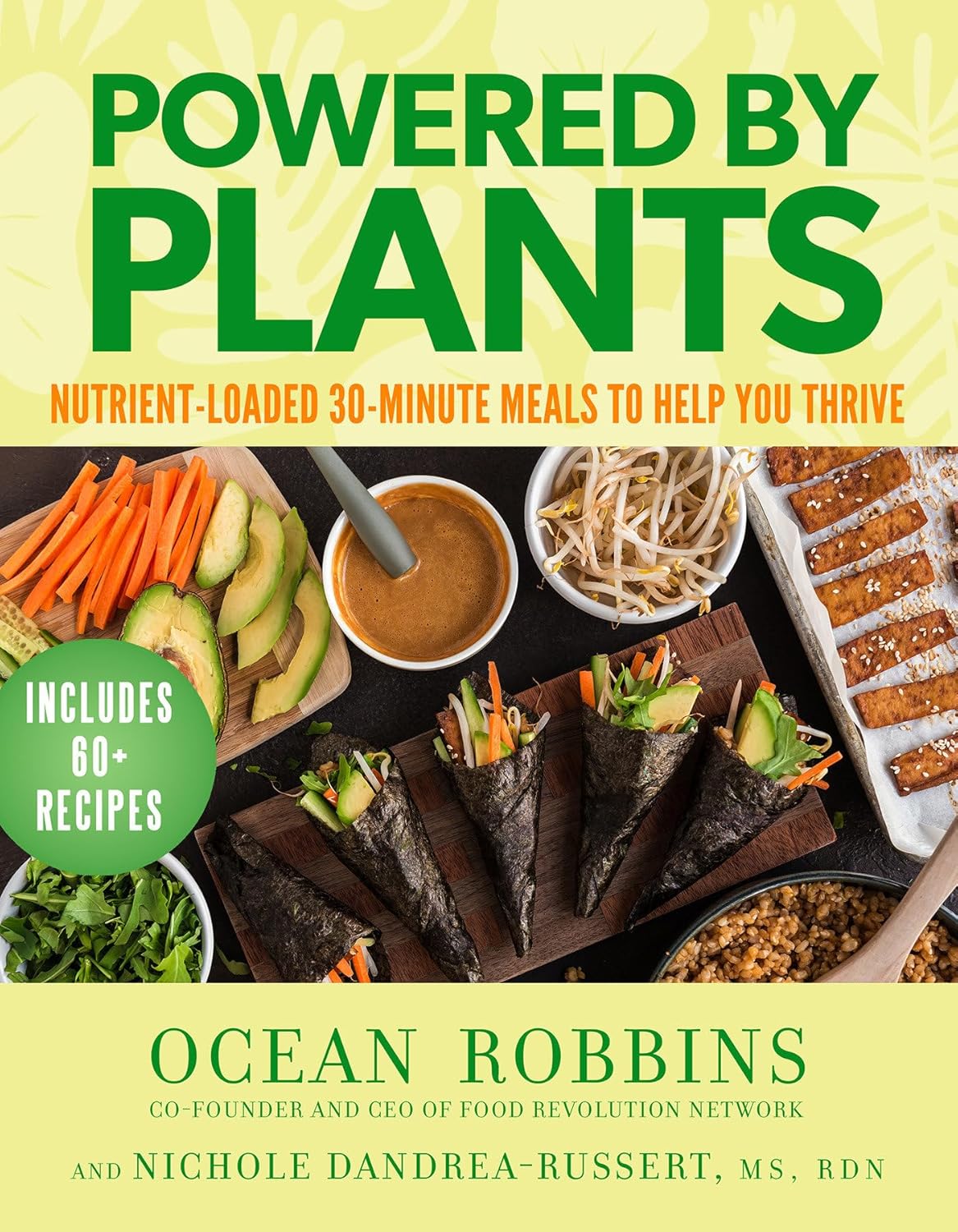
Powered by Plants – by Ocean Robbins & Nichole Dandrea-Russert
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Of the two authors, the former is a professional public speaker, and the latter is a professional dietician. As a result, we get a book that is polished and well-presented, while actually having a core of good solid science (backed up with plenty of references).
There’s an introductory section that’s all about the “notable nutrients”, that will be focused on in the ingredients choices for the recipes in the rest of the book.
The recipes themselves are simple enough to do quickly, yet interesting enough that you’ll want to do them, and certainly they contain all the plant-based nutrient-density you might expect.
Bottom line: if you’d like to expand your plant-based cooking with a focus on nutrition and ease without sacrificing fun, then this is a great cookbook for that.
Click here to check out Powered by Plants, and get powered by plants!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Managing Jealousy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Jealousy is often thought of as a young people’s affliction, but it can affect us at any age—whether we are the one being jealous, or perhaps a partner.
And, the “green-eyed monster” can really ruin a lot of things; relationships, friendships, general happiness, physical health even (per stress and anxiety and bad sleep), and more.
The thing is, jealousy looks like one thing, but is actually mostly another.
Jealousy is a Scooby-Doo villain
That is to say: we can unmask it and see what much less threatening thing is underneath. Which is usually nothing more nor less than: insecurities
- Insecurity about losing one’s partner
- Insecurity about not being good enough
- Insecurity about looking bad socially
…etc. The latter, by the way, is usually the case when one’s partner is socially considered to be giving cause for jealousy, but the primary concern is not actually relational loss or any kind of infidelity, but rather, looking like one cannot keep one’s partner’s full attention romantically/sexually. This drives a lot of people to act on jealousy for the sake of appearances, in situations where they might otherwise, if they didn’t feel like they’d be adversely judged for it, be considerably more chill.
Thus, while monogamy certainly has its fine merits, there can also be a kind of “toxic monogamy” at hand, where a relationship becomes unhealthy because one partner is just trying to live up to social expectations of keeping the other partner in check.
This, by the way, is something that people in polyamorous and/or open relationships typically handle quite neatly, even if a lot of the following still applies. But today, we’re making the statistically safe assumption of a monogamous relationship, and talking about that!
How to deal with the social aspect
If you sit down with your partner and work out in advance the acceptable parameters of your relationship, you’ll be ahead of most people already. For example…
- What counts as cheating? Is it all and any sex acts with all and any people? If not, where’s the line?
- What about kissing? What about touching other body parts? If there are boundaries that are important to you, talk about them. Nothing is “too obvious” because it’s astonishing how many times it will happen that later someone says (in good faith or not), “but I thought…”
- What about being seen in various states of undress? Or seeing other people in various states of undress?
- Is meaningless flirting between friends ok, and if so, how do we draw the line with regard to what is meaningless? And how are we defining flirting, for that matter? Talk about it and ensure you are both on the same page.
- If a third party is possibly making moves on one of us under the guise of “just being friendly”, where and how do we draw the line between friendliness and romantic/sexual advances? What’s the difference between a lunch date with a friend and a romantic meal out for two, and how can we define the difference in a way that doesn’t rely on subjective “well I didn’t think it was romantic”?
If all this seems like a lot of work, please bear in mind, it’s a lot more fun to cover this cheerfully as a fun couple exercise in advance, than it is to argue about it after the fact!
See also: Boundary-Setting Beyond “No”
How to deal with the more intrinsic insecurities
For example, when jealousy is a sign of a partner fearing not being good enough, not measuring up, or perhaps even losing their partner.
The key here might not shock you: communication
Specifically, reassurance. But critically, the correct reassurance!
A partner who is jealous will often seek the wrong reassurance, for example wanting to read their partner’s messages on their phone, or things like that. And while a natural desire when experiencing jealousy, it’s not actually helpful. Because while incriminating messages could confirm infidelity, it’s impossible to prove a negative, and if nothing incriminating is found, the jealous partner can just go on fearing the worst regardless. After all, their partner could have a burner phone somewhere, or a hidden app for cheating, or something else like that. So, no reassurance can ever be given/gained by such requests (which can also become unpleasantly controlling, which hopefully nobody wants).
A quick note on “if you have nothing to fear, you have nothing to hide”: rhetorically that works, but practically it doesn’t.
Writer’s example: when my late partner and I formalized our relationship, we discussed boundaries, and I expressed “so far as I am concerned, I have no secrets from you, except secrets that are not mine to share. For example, if someone has confided in me and asked that I not share it, I won’t. Aside from that, you have access-all-areas in my life; me being yours has its privileges” and this policy itself would already pre-empt any desire to read my messages.
Now indeed, I had nothing to hide. I am by character devoted to a fault. But my friends may well sometimes have things they don’t want me to share, which made that a necessary boundary to highlight (which my partner, an absolute angel by the way and not prone to unhealthy manifestations of jealousy in any case, understood completely).
So, it is best if the partner of a jealous person can explain the above principles as necessary, and offer the correct reassurance instead. Which could be any number of things, but for example:
- I am yours, and nobody else has a chance
- I fully intend to stay with you for life
- You are the best partner I have ever had
- Being with you makes my life so much better
…etc. Note that none of these are “you don’t have to worry about so-and-so”, or “I am not cheating on you”, etc, because it’s about yours and your partner’s relationship. If they ask for reassurances with regard to other people or activities, by all means state them as appropriate, but try to keep the focus on you two.
And if your partner (or you, if it’s you who’s jealous) can express the insecurity in the format…
“I’m afraid of _____ because _____”
…then the “because” will allow for much more specific reassurance. We all have insecurities, we all have reasons we might fear not being good enough for our partner, or losing their affection, and the best thing we can do is choose to trust our partners at least enough to discuss those fears openly with each other.
See also: Save Time With Better Communication ← this can avoid a lot of time-consuming arguments
What about if the insecurity is based in something demonstrably correct?
By this we mean, something like a prior history of cheating, or other reasons for trust issues. In such a case, the jealous partner may well have a reason for their jealousy that isn’t based on a personal insecurity.
In our previous article about boundaries, we talked about relationships (romantic or otherwise) having a “price of entry”. In this case, you each have a “price of entry”:
- The “price of entry” to being with the person who has previously cheated (or similar), is being able to accept that.
- And for the person who cheated (or similar), very likely their partner will have the “price of entry” of “don’t do that again, and also meanwhile accept in good grace that I might be jittery about it”.
And, if the betrayal of trust was something that happened between the current partners in the current relationship, most likely that was also traumatic for the person whose trust was betrayed. Many people in that situation find that trust can indeed be rebuilt, but slowly, and the pain itself may also need treatment (such as therapy and/or couples therapy specifically).
See also: Relationships: When To Stick It Out & When To Call It Quits ← this covers both sides
And finally, to finish on a happy note:
Only One Kind Of Relationship Promotes Longevity This Much!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Foods for Stronger Bones
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Q: Foods that help build stronger bones and cut inflammation? Thank you!
We’ve got you…
For stronger bones / To cut inflammation
That “stronger bones” article is about the benefits of collagen supplementation for bones, but there’s definitely more to say on the topic of stronger bones, so we’ll do a main feature on it sometime soon!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: