How to Use Topical Estrogen Cream For Aging Skin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Sam Ellis, dermatologist, explains:
Tackling the cause
Estrogen is important for very many aspects of health beyond the sexual aspects. When it comes to skin, a drop in estrogen (usually because of menopause) leads to changes like collagen loss, dryness, reduced elasticity, and slower wound healing. Applying estrogen creams to the skin can reverse these changes.
If your estrogen levels are already within normal pre-menopausal female ranges, by the way, there isn’t so much science to indicate its benefit when used topically. If you are already on systemic HRT (i.e., you take estrogen already to raise your blood estrogen levels and affect your body in its entirety), you may or may not gain extra benefits from the topical cream, depending on factors such as your estrogen dose, your route of administration, your cardiovascular health, and other factors.
For those with lower estrogen and not currently on HRT, you may be wondering: can topical estrogen cream affect systemic estrogen levels? And the answer is that it mostly depends on the dose. In other words: it’s definitely possible, but for most people it’s unlikely.
As ever, if thinking of taking up any hormonal treatment, do consult an endocrinologist and/or gynecologist, and if you have an increased breast cancer risk (for example genetically or prior history), then an oncologist too, just to be safe.
That sounds like a lot of scary things, but mostly it’s just to be on the safe side. The dose of estrogen is very low in topical creams, and even then, only a tiny amount is used per day.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- “Why Does It Hurt When I Have Sex?” (And What To Do About It) ← because topical estrogen is not just for your face! Yes, you can use it down there too and it’s commonly prescribed for exactly this use.
- Hormones & Health, Beyond The Obvious
- The Hormone Therapy That Reduces Breast Cancer Risk & More
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Having an x-ray to diagnose knee arthritis might make you more likely to consider potentially unnecessary surgery
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Osteoarthritis is a leading cause of chronic pain and disability, affecting more than two million Australians.
Routine x-rays aren’t recommended to diagnose the condition. Instead, GPs can make a diagnosis based on symptoms and medical history.
Yet nearly half of new patients with knee osteoarthritis who visit a GP in Australia are referred for imaging. Osteoarthritis imaging costs the health system A$104.7 million each year.
Our new study shows using x-rays to diagnose knee osteoarthritis can affect how a person thinks about their knee pain – and can prompt them to consider potentially unnecessary knee replacement surgery.
pikselstock/Shutterstock What happens when you get osteoarthritis?
Osteoarthritis arises from joint changes and the joint working extra hard to repair itself. It affects the entire joint, including the bones, cartilage, ligaments and muscles.
It is most common in older adults, people with a high body weight and those with a history of knee injury.
Many people with knee osteoarthritis experience persistent pain and have difficulties with everyday activities such as walking and climbing stairs.
How is it treated?
In 2021–22, more than 53,000 Australians had knee replacement surgery for osteoarthritis.
Hospital services for osteoarthritis, primarily driven by joint replacement surgery, cost $3.7 billion in 2020–21.
While joint replacement surgery is often viewed as inevitable for osteoarthritis, it should only be considered for those with severe symptoms who have already tried appropriate non-surgical treatments. Surgery carries the risk of serious adverse events, such as blood clot or infection, and not everyone makes a full recovery.
Most people with knee osteoarthritis can manage it effectively with:
- education and self-management
- exercise and physical activity
- weight management (if necessary)
- medicines for pain relief (such as paracetamol and non-steroidal anti-inflammatory drugs).
Debunking a common misconception
A common misconception is that osteoarthritis is caused by “wear and tear”.
However, research shows the extent of structural changes seen in a joint on an x-ray does not reflect the level of pain or disability a person experiences, nor does it predict how symptoms will change.
Some people with minimal joint changes have very bad symptoms, while others with more joint changes have only mild symptoms. This is why routine x-rays aren’t recommended for diagnosing knee osteoarthritis or guiding treatment decisions.
Instead, guidelines recommend a “clinical diagnosis” based on a person’s age (being 45 years or over) and symptoms: experiencing joint pain with activity and, in the morning, having no joint-stiffness or stiffness that lasts less than 30 minutes.
Despite this, many health professionals in Australia continue to use x-rays to diagnose knee osteoarthritis. And many people with osteoarthritis still expect or want them.
What did our study investigate?
Our study aimed to find out if using x-rays to diagnose knee osteoarthritis affects a person’s beliefs about osteoarthritis management, compared to a getting a clinical diagnosis without x-rays.
We recruited 617 people from across Australia and randomly assigned them to watch one of three videos. Each video showed a hypothetical consultation with a general practitioner about knee pain.
People with knee osteoarthritis can have difficulties getting down stairs. beeboys/Shutterstock One group received a clinical diagnosis of knee osteoarthritis based on age and symptoms, without being sent for an x-ray.
The other two groups had x-rays to determine their diagnosis (the doctor showed one group their x-ray images and not the other).
After watching their assigned video, participants completed a survey about their beliefs about osteoarthritis management.
What did we find?
People who received an x-ray-based diagnosis and were shown their x-ray images had a 36% higher perceived need for knee replacement surgery than those who received a clinical diagnosis (without x-ray).
They also believed exercise and physical activity could be more harmful to their joint, were more worried about their condition worsening, and were more fearful of movement.
Interestingly, people were slightly more satisfied with an x-ray-based diagnosis than a clinical diagnosis.
This may reflect the common misconception that osteoarthritis is caused by “wear and tear” and an assumption that the “damage” inside the joint needs to be seen to guide treatment.
What does this mean for people with osteoarthritis?
Our findings show why it’s important to avoid unnecessary x-rays when diagnosing knee osteoarthritis.
While changing clinical practice can be challenging, reducing unnecessary x-rays could help ease patient anxiety, prevent unnecessary concern about joint damage, and reduce demand for costly and potentially unnecessary joint replacement surgery.
It could also help reduce exposure to medical radiation and lower health-care costs.
Previous research in osteoarthritis, as well as back and shoulder pain, similarly shows that when health professionals focus on joint “wear and tear” it can make patients more anxious about their condition and concerned about damaging their joints.
If you have knee osteoarthritis, know that routine x-rays aren’t needed for diagnosis or to determine the best treatment for you. Getting an x-ray can make you more concerned and more open to surgery. But there are a range of non-surgical options that could reduce pain, improve mobility and are less invasive.
Belinda Lawford, Senior Research Fellow in Physiotherapy, The University of Melbourne; Kim Bennell, Professor of Physiotherapy, The University of Melbourne; Rana Hinman, Professor in Physiotherapy, The University of Melbourne, and Travis Haber, Postdoctoral Research Fellow in Physiotherapy, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
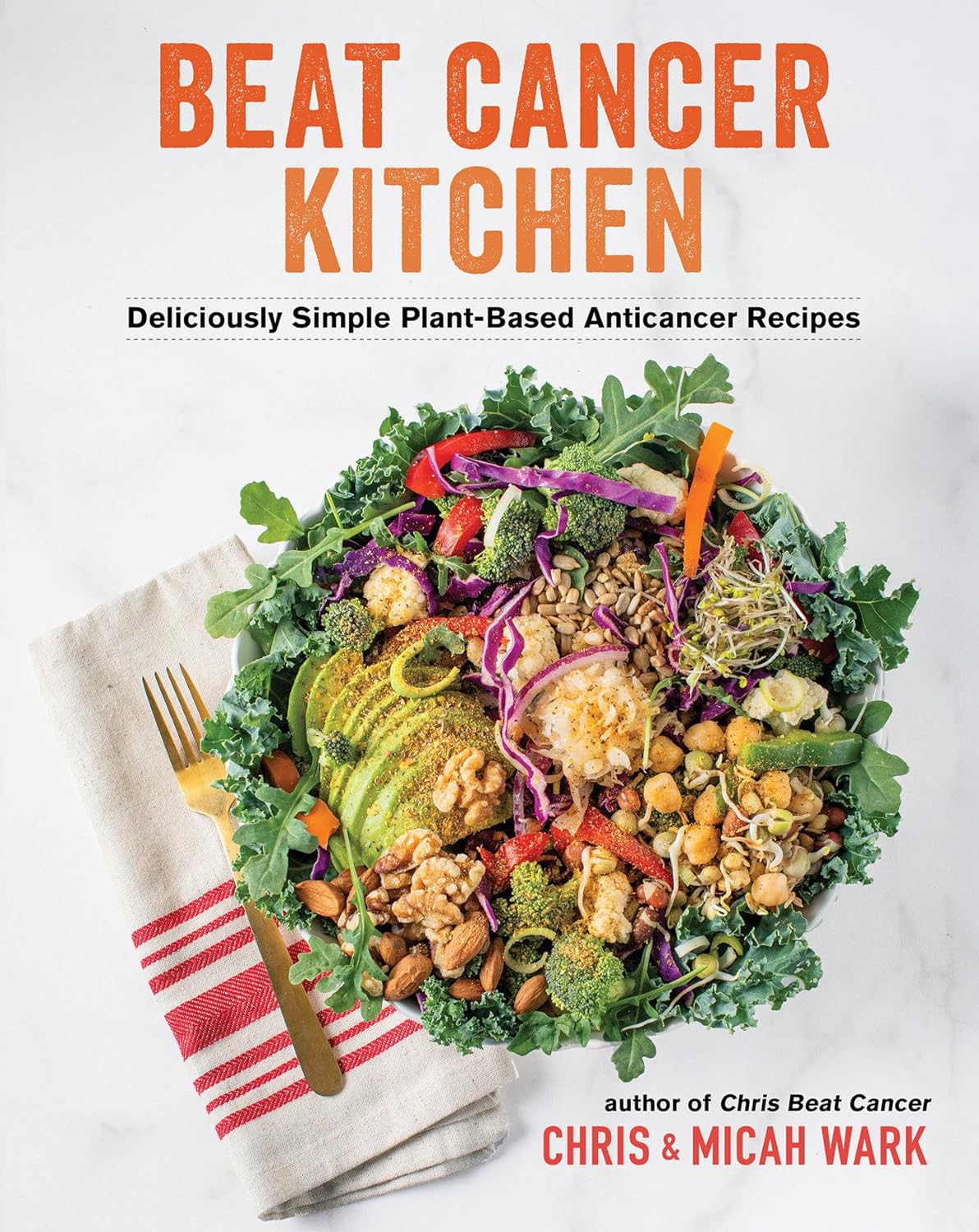
Beat Cancer Kitchen – by Chris Wark & Micah Wark
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When we eat, many things can increase our cancer risk. Some we might remember to avoid, like ultra-processed foods and red meat. Others might be more neutral when it comes to cancer, neither good nor bad.
But! Some foods also have cancer-fighting properties. Which means reducing cancer risk, and/or having an anti-proliferative effect (i.e., shrinks or at least slows growth of tumors), in the event of already having cancer.
That’s what Chris & Micah Wark are offering here; a cookbook built around anti-cancer foods—after the former beat his own cancer with the help of the latter. He had surgery, but skipped chemo, preferring to look to nutrition to keep cancer-free. Now 18 years later, and so far, so good.
The dietary advice here is entirely consistent with what we’d offer at 10almonds; it’s plant-based, and high in anti-cancer phytonutrients.
The recipes themselves (of which there are about 70-ish) are as delicious and simple as the title suggests, and/but you might want to know:
- On the one hand, many recipes are things like sauces, condiments, or dressings, which in a recipe book can sometimes feel like underdelivering on the promise of recipes when we expect full meals
- On the other hand, those things if you just purchase them ready-made are usually the things with the most ultra-processed products, thus, having anticancer homemade versions instead here can actually make a very big difference
- On the third hand, there areplenty of starters/mains/desserts too!
Bottom line: if you’re looking for an anti-cancer cookbook, this is a very good one whose ingredients aren’t obscure (which can otherwise be a problem for some books of this kind)
Click here to check out Beat Cancer Kitchen, and take good care of yourself and your loved ones!
Share This Post
-
Fall Special
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Some fall-themed advice…
It is now, nominally at least, fall. We’re going to talk about the other kind of “fall” though, the kind that results in broken hips and more.
If you’re thinking “not me; that happens to older more infirm people”, rest assured, it can and statistically probably will happen to you at some point. So, how to play the odds?
First, be robust!
We may not be able to make ourselves like children who bounce easily, but we also don’t have to crumble into dust at the slightest knock, either. There are two important ways we can start to make ourselves robust from the inside out, and they are simple: diet and exercise.
- Diet: The Bare-Bones Truth About Osteoporosis
- Exercise: Osteoporosis Exercises
“But I don’t have osteoporosis”—great! But osteoporosis is preceded by osteopenia, which is generally asymptomatic at first, and also if we’re not very careful about it, we will lose about 1% bone density per year from the age of about 35 onwards, with that rate of loss climbing sharply from the age of 50 onwards, and even more steeply in cases of untreated menopause.
So in other words, don’t take your bone strength for granted; there’s a first time for everything, and you don’t want to find out the hard (and yet, dare we say it, brittle) way.
Second, be dynamic!
Be able to fall and get up safely. If your later life is going to be a triathlon of things you need to train for now, then being able to fall and get up safely should be at the top of the list.
Being able to “deep squat” will help you a lot here, in being able to get up with minimal (or no) use of your hands. We shared a great instructional video about this last week.
It also means that the more your lower body can still take your weight while your torso is closer to the ground (without your legs buckling and collapsing, for instance), the softer and gentler you’ll hit the floor if you do fall, because the final “drop” will be from a lower height.
If at all possible, consider taking some classes of a martial art that involves safely falling—aikido is typically the softest and gentlest and is famously great for people of all ages, but judo or jujitsu will suffice if aikido isn’t available where you are. You don’t have to get a black belt (unless you want to), and any decent instructor will be happy to guide you through the basics of safely falling and then send you on your merry way, if that’s all you wanted.
The benefits of this are twofold:
- Obviously, if you fall, you will have better technique and thus be less likely to incur injury
- As you are falling, you will be less afraid, and thus less likely to tense up mid-fall (tensing up will exacerbate any falling injury)
Click here to find an aikido teacher near you (you can search by country, state, and city)
Third, be balanced!
Spending even just a few minutes each day working on your balance can go a long way.
Standing on one leg (and then the other) is a very good obvious starting point. Please, do so safely. The shower is not the best place to take up this practice, for instance. A nice safe grassy area is great. Your carpeted living room or bedroom is next-best.
Another great approach is the practice of bāguàzhǎng circle-walking.
Bāguà is tai chi’s lesser-known cousin, and those arts are two of the three main schools of wǔdāngquán. But, fear not, you don’t have to don orange robes and live atop the Wudang mountains to get what you need in this case.
To give a text-based summary: bāguàzhǎng circle-walking involves walking in a small circle, with a low center of gravity, moving one’s weight very purposefully from one leg to the other, keeping complete stability the whole time that one is (often!) on one leg.
Once you get good at this, you’ll see that this is essentially a super-enhanced version of the “standing on one leg” exercise, because it’s about keeping balance while on one leg, and/but while moving also.
Naturally, if you do get good at this, you’ll be very unlikely to fall in the first place.
Here’s a visual primer. This video will show the basic footwork, and the video that follows it (it’ll prompt you if you want to watch it) shows how to bring it up to a standard walking speed, without losing fluidity of movement:
Share This Post
Related Posts
-
The Hidden Risk of Stretching: Avoiding Hamstring Injuries in Yoga
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What is Yoga Butt
Have you ever experienced a mysterious pain while stretching, or perhaps during yoga? You might be dealing with “yoga butt,” a common—although rarely discussed—injury. In the below video, the Lovely Liv from Livinleggings shares her journey of discovering, and overcoming, “yoga butt”.
Dealing With Yoga Butt
Yoga butt, or proximal hamstring tendinopathy, occurs when the hamstrings are overstretched without adequate strengthening. Many yoga poses help stretch the hamstrings, but often don’t focus on strengthening said hamstrings; this imbalance is what can lead to damage over time.
To help prevent Yoga butt, it’s essential to balance stretching with strengthening. You can look into incorporating hamstring-strengthening exercises like Romanian deadlifts, hamstring curls, and modified yoga poses into your routine.
(If you’re new to strengthening exercises, we recommend reading Women’s Strength Training Anatomy Workouts or Strength Training for Seniors).
Watch the full video to learn more and hopefully protect yourself from long-term injuries:
Let us know your thoughts, and whether you have any other topics you’d like us to cover.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
We looked at 700 plant-based foods to see how healthy they really are. Here’s what we found
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’re thinking about buying plant-based foods, a trip to the supermarket can leave you bewildered.
There are plant-based burgers, sausages and mince. The fridges are loaded with non-dairy milk, cheese and yoghurt. Then there are the tins of beans and packets of tofu.
But how much is actually healthy?
Our nutritional audit of more than 700 plant-based foods for sale in Australian supermarkets has just been published. We found some products are so high in salt or saturated fat, we’d struggle to call them “healthy”.
We took (several) trips to the supermarket
In 2022, we visited two of each of four major supermarket retailers across Melbourne to collect information on the available range of plant-based alternatives to meat and dairy products.
We took pictures of the products and their nutrition labels.
We then analysed the nutrition information on the packaging of more than 700 of these products. This included 236 meat substitutes, 169 legumes and pulses, 50 baked beans, 157 dairy milk substitutes, 52 cheese substitutes and 40 non-dairy yoghurts.
Plant-based meats were surprisingly salty
We found a wide range of plant-based meats for sale. So, it’s not surprising we found large variations in their nutrition content.
Sodium, found in added salt and which contributes to high blood pressure, was our greatest concern.
The sodium content varied from 1 milligram per 100 grams in products such as tofu, to 2,000mg per 100g in items such as plant-based mince products.
This means we could eat our entire daily recommended sodium intake in just one bowl of plant-based mince.
An audit of 66 plant-based meat products in Australian supermarkets conducted in 2014 found sodium ranged from 316mg in legume-based products to 640mg in tofu products, per 100g. In a 2019 audit of 137 products, the range was up to 1,200mg per 100g.
In other words, the results of our audit seems to show a consistent trend of plant-based meats getting saltier.
Looking for plant-based meat? Check the label for the sodium content.
Michael Vi/Shutterstock
What about plant-based milks?
Some 70% of the plant-based milks we audited were fortified with calcium, a nutrient important for bone health.
This is good news as a 2019-2020 audit of 115 plant-based milks from Melbourne and Sydney found only 43% of plant-based milks were fortified with calcium.
Of the fortified milks in our audit, almost three-quarters (73%) contained the recommended amount of calcium – at least 100mg per 100mL.
We also looked at the saturated fat content of plant-based milks.
Coconut-based milks had on average up to six times higher saturated fat content than almond, oat or soy milks.
Previous audits also found coconut-based milks were much higher in saturated fat than all other categories of milks.
Some plant-based milks were healthier than others.
TY Lim/Shutterstock
A first look at cheese and yoghurt alternatives
Our audit is the first study to identify the range of cheese and yoghurt alternatives available in Australian supermarkets.
Calcium was only labelled on a third of plant-based yoghurts, and only 20% of supermarket options met the recommended 100mg of calcium per 100g.
For plant-based cheeses, most (92%) were not fortified with calcium. Their sodium content varied from 390mg to 1,400mg per 100g, and saturated fat ranged from 0g to 28g per 100g.
So, what should we consider when shopping?
As a general principle, try to choose whole plant foods, such as unprocessed legumes, beans or tofu. These foods are packed with vitamins and minerals. They’re also high in dietary fibre, which is good for your gut health and keeps you fuller for longer.
If opting for a processed plant-based food, here are five tips for choosing a healthier option.
1. Watch the sodium
Plant-based meat alternatives can be high in sodium, so look for products that have around 150-250mg sodium per 100g.
2. Pick canned beans and legumes
Canned chickpeas, lentils and beans can be healthy and low-cost additions to many meals. Where you can, choose canned varieties with no added salt, especially when buying baked beans.
3. Add herbs and spices to your tofu
Tofu can be a great alternative to meat. Check the label and pick the option with the highest calcium content. We found flavoured tofu was higher in salt and sugar content than minimally processed tofu. So it’s best to pick an unflavoured option and add your own flavours with spices and herbs.
4. Check the calcium
When choosing a non-dairy alternative to milk, such as those made from soy, oat, or rice, check it is fortified with calcium. A good alternative to traditional dairy will have at least 100mg of calcium per 100g.
5. Watch for saturated fat
If looking for a lower saturated fat option, almond, soy, rice and oat varieties of milk and yoghurt alternatives have much lower saturated fat content than coconut options. Pick those with less than 3g per 100g.
Laura Marchese, PhD Student at the Institute for Physical Activity and Nutrition, Deakin University and Katherine Livingstone, NHMRC Emerging Leadership Fellow and Senior Research Fellow at the Institute for Physical Activity and Nutrition, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Sesame Oil vs Almond Oil – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sesame oil to almond oil, we picked the almond.
Why?
We were curious about this one! Were you, or were you confident? You see, almonds tend to blow away all the other nuts with their nutritional density, but they’re far from the oiliest of nuts, and their greatest strengths include their big dose of protein and fiber (which don’t make it into the oil), vitamins (most of which don’t make it into the oil) and minerals (which don’t make it into the oil). So, a lot will come down to the fat profile!
On which note, looking at the macros first, it’s 100% fat in both cases, but sesame oil has more saturated fat and polyunsaturated fat, while almond oil has more monounsaturated fat. Since the mono- and poly-unsaturated fats are both healthy and each oil has more of one or the other, the deciding factor here is which has the least saturated fat—and that’s the almond oil, which has close to half the saturated fat of sesame oil. As an aside, neither of them are a source of omega-3 fatty acids.
In terms of vitamins, there’s not a lot to say here, but “not a lot” is not nothing: sesame oil has nearly 2x the vitamin K, while almond oil has 28x the vitamin E*, and 2x the choline. So, another win for almond oil.
*which is worth noting, not least of all because seeds are more widely associated with vitamin E in popular culture, but it’s the almond oil that provide much more here. Not to get too distracted into looking at the values of the actual seeds and nuts, almonds themselves do have over 102x the vitamin E compared to sesame seeds.
Now, back to the oils:
In the category of minerals, there actually is nothing to say here, except you can’t get more than the barest trace of any mineral from either of these two oils. So it’s a tie on this one.
Adding up the categories makes for a clear win for almond oil!
Want to learn more?
You might like to read:
Avocado Oil vs Olive Oil – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: