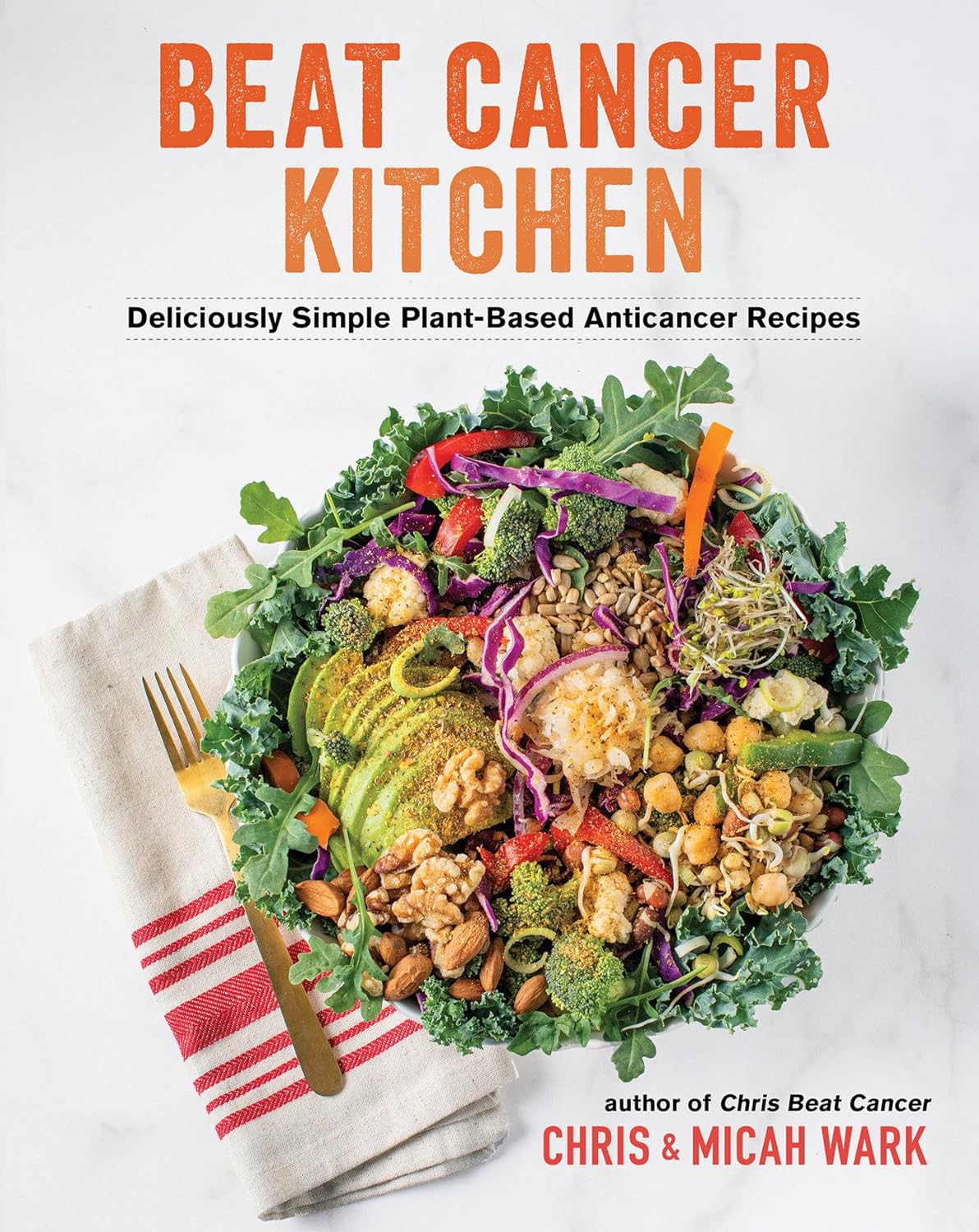
Beat Cancer Kitchen – by Chris Wark & Micah Wark
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When we eat, many things can increase our cancer risk. Some we might remember to avoid, like ultra-processed foods and red meat. Others might be more neutral when it comes to cancer, neither good nor bad.
But! Some foods also have cancer-fighting properties. Which means reducing cancer risk, and/or having an anti-proliferative effect (i.e., shrinks or at least slows growth of tumors), in the event of already having cancer.
That’s what Chris & Micah Wark are offering here; a cookbook built around anti-cancer foods—after the former beat his own cancer with the help of the latter. He had surgery, but skipped chemo, preferring to look to nutrition to keep cancer-free. Now 18 years later, and so far, so good.
The dietary advice here is entirely consistent with what we’d offer at 10almonds; it’s plant-based, and high in anti-cancer phytonutrients.
The recipes themselves (of which there are about 70-ish) are as delicious and simple as the title suggests, and/but you might want to know:
- On the one hand, many recipes are things like sauces, condiments, or dressings, which in a recipe book can sometimes feel like underdelivering on the promise of recipes when we expect full meals
- On the other hand, those things if you just purchase them ready-made are usually the things with the most ultra-processed products, thus, having anticancer homemade versions instead here can actually make a very big difference
- On the third hand, there areplenty of starters/mains/desserts too!
Bottom line: if you’re looking for an anti-cancer cookbook, this is a very good one whose ingredients aren’t obscure (which can otherwise be a problem for some books of this kind)
Click here to check out Beat Cancer Kitchen, and take good care of yourself and your loved ones!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Can You Repair Your Own Teeth At Home?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I liked your article on tooth remineralization, I saw a “home tooth repair kit”, and wondered if it is as good as what dentists do, or at least will do the job well enough to save a dentist visit?❞
Firstly, for any wondering about the tooth remineralization, here you go:
Tooth Remineralization: How To Heal Your Teeth Naturally
Now, to answer your question, we presume you are talking about something like this kit available on Amazon. In which case, some things to bear in mind:
- This kind of thing is generally intended as a stop-gap measure until you see a dentist, because you cracked your tooth or lost a filling or something today, and will see the dentist next week, say.
- This kind of thing is not what Dr. Michelle Jorgensen was talking about in another video* that we wrote about; rather, it is using a polymer filler to rebuild what is missing. The key difference is: this is using plastic, which is not what your teeth are made of, so it will never “take” as part of the tooth, as some biomimetic dentistry options can do.
- Yes, this does also mean you are putting microplastics (because the powder is usually micronized polymer beads with zinc oxide, to which you add a liquid to create a paste that will set) in your mouth and quite possibly right next to an open blood supply depending on what’s damaged and whether capillaries were reaching it.
- Because of the different material and application method, the adhesion is nothing like professional fillings (be they metal or resin), and thus the chances of it coming out again or so high that it’s more a question of when, rather than if.
- If you have damage under there (as we presume you do in any scenario where you are using this), then if it’s not professionally cleaned before the filling goes in, then it can get infected, and (less dramatically, but still importantly) any extant decay can also get worse. We say “professionally”, because you will not be able to do an adequate job with your toothbrush, floss, etc at home, and even if you got dentist’s tools (which you can buy, by the way, but we don’t recommend), you will no more be able to do the same quality job as a dentist who has done that many times a day every day for the past 20 years, as buying expensive paintbrushes would make you able to restore a Renaissance painting without messing it up.
*See: Dangers Of Root Canals And Crowns, & What To Do Instead ← what she recommends instead is biomimetic dentistry, which is also more prosaically called “conservative restorative dentistry”, i.e. it tries to conserve as much as possible, replace lost material on a like-for-like basis, and generally end up with a result that’s as close to natural as possible.
In other words, the short answer to your question is “no, sorry, it isn’t and it won’t”
However! A just like it’s good to have a first aid kit in the house even if it won’t do the same job as an ambulance crew, it can be good to have a tooth repair kit (essentially, a tooth first-aid kit) in the house, precisely to use it just as a stop-gap measure in the event that you one day crack a tooth or lose a filling or such, and don’t want to leave it open to all things in the meantime.
(The results of this sort of kit are so not long-term in nature that it will be quick and easy for your dentist to remove it to do their own job once you get there)
If in doubt, always see your dentist as soon as possible, as many things are a lot less work to treat now, than to treat later. Just, make sure to advocate for yourself and what you actually want/need, and don’t let them upsell you on something you didn’t come in for while you’re sitting in their chair—that’s a conversation to be had in advance with a clear head and no pressure (and nobody’s hands in your mouth)!
See also: Dentists Are Pulling ‘Healthy’ and Treatable Teeth To Profit From Implants, Experts Warn
Take care!
Share This Post
-
The Many Faces Of Cosmetic Surgery
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cosmetic Surgery: What’s The Truth?
In Tuesday’s newsletter, we asked you your opinion on elective cosmetic surgeries, and got the above-depicted, below-described, set of responses:
- About 48% said “Everyone should be able to get what they want, assuming informed consent”
- About 28% said “It can ease discomfort to bring features more in line with normalcy”
- 15% said “They should be available in the case of extreme disfigurement only”
- 10% said “No elective cosmetic surgery should ever be performed; needless danger”
Well, there was a clear gradient of responses there! Not so polarizing as we might have expected, but still enough dissent for discussion
So what does the science say?
The risks of cosmetic surgery outweigh the benefits: True or False?
False, subjectively (but this is important).
You may be wondering: how is science subjective?
And the answer is: the science is not subjective, but people’s cost:worth calculations are. What’s worth it to one person absolutely may not be worth it to another. Which means: for those for whom it wouldn’t be worth it, they are usually the people who will not choose the elective surgery.
Let’s look at some numbers (specifically, regret rates for various surgeries, elective/cosmetic or otherwise):
- Regret rate for elective cosmetic surgery in general: 20%
- Regret rate for knee replacement (i.e., not cosmetic): 17.1%
- Regret rate for hip replacement (i.e., not cosmetic): 4.8%
- Regret rate for gender-affirming surgeries (for transgender patients): 1%
So we can see, elective surgeries have an 80–99% satisfaction rate, depending on what they are. In comparison, the two joint replacements we mentioned have a 82.9–95.2% satisfaction rate. Not too dissimilar, taken in aggregate!
In other words: if a person has studied the risks and benefits of a surgery and decides to go ahead, they’re probably going to be happy with the results, and for them, the benefits will have outweighed the risks.
Sources for the above numbers, by the way:
- What is the regret rate for plastic surgery?
- Decision regret after primary hip and knee replacement surgery
- A systematic review of patient regret after surgery—a common phenomenon in many specialties but rare within gender-affirmation surgery
But it’s just a vanity; therapy is what’s needed instead: True or False?
False, generally. True, sometimes. Whatever the reasons for why someone feels the way they do about their appearance—whether their face got burned in a fire or they just have triple-J cups that they’d like reduced, it’s generally something they’ve already done a lot of thinking about. Nevertheless, it does also sometimes happen that it’s a case of someone hoping it’ll be the magical solution, when in reality something else is also needed.
How to know the difference? One factor is whether the surgery is “type change” or “restorative”, and both have their pros and cons.
- In “type change” (e.g. rhinoplasty), more psychological adjustment is needed, but when it’s all over, the person has a new nose and, statistically speaking, is usually happy with it.
- In “restorative” (e.g. facelift), less psychological adjustment is needed (as it’s just a return to a previous state), so a person will usually be happy quickly, but ultimately it is merely “kicking the can down the road” if the underlying problem is “fear of aging”, for example. In such a case, likely talking therapy would be beneficial—whether in place of, or alongside, cosmetic surgery.
Here’s an interesting paper on that; the sample sizes are small, but the discussion about the ideas at hand is a worthwhile read:
Does cosmetic surgery improve psychosocial wellbeing?
Some people will never be happy no matter how many surgeries they get: True or False?
True! We’re going to refer to the above paper again for this one. In particular, here’s what it said about one group for whom surgeries will not usually be helpful:
❝There is a particular subgroup of people who appear to respond poorly to cosmetic procedures. These are people with the psychiatric disorder known as “body dysmorphic disorder” (BDD). BDD is characterised by a preoccupation with an objectively absent or minimal deformity that causes clinically significant distress or impairment in social, occupational, or other areas of functioning.
For several reasons, it is important to recognise BDD in cosmetic surgery settings:
Firstly, it appears that cosmetic procedures are rarely beneficial for these people. Most patients with BDD who have had a cosmetic procedure report that it was unsatisfactory and did not diminish concerns about their appearance.
Secondly, BDD is a treatable disorder. Serotonin-reuptake inhibitors and cognitive behaviour therapy have been shown to be effective in about two-thirds of patients with BDD❞
~ Dr. David Castle et al. (lightly edited for brevity)
Which is a big difference compared to, for example, someone having triple-J breasts that need reducing, or the wrong genitals for their gender, or a face whose features are distinct outliers.
Whether that’s a reason people with BDD shouldn’t be able to get it is an ethical question rather than a scientific one, so we’ll not try to address that with science.
After all, many people (in general) will try to fix their woes with a haircut, a tattoo, or even a new sportscar, and those might sometimes be bad decisions, but they are still the person’s decision to make.
And even so, there can be protectionist laws/regulations that may provide a speed-bump, for example:
Take care!
Share This Post
-
What You Don’t Know Can Kill You
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Knowledge Is Power!
This is Dr. Simran Malhotra. She’s triple board-certified (in lifestyle medicine, internal medicine, and palliative care), and is also a health and wellness coach.
What does she want us to know?
Three things:
Wellness starts with your mindset
Dr. Malhotra shifted her priorities a lot during the initial and perhaps most chaotic phase of the COVID pandemic:
❝My husband, a critical care physician, was consumed in the trenches of caring for COVID patients in the ICU. I found myself knee-deep in virtual meetings with families whose loved ones were dying of severe COVID-related illnesses. Between the two of us, we saw more trauma, suffering, and death, than we could have imagined.
The COVID-19 pandemic opened my eyes to how quickly life can change our plans and reinforced the importance of being mindful of each day. Harnessing the power to make informed decisions is important, but perhaps even more important is focusing on what is in our control and taking action, even if it is the tiniest step in the direction we want to go!❞
~ Dr. Simran Malhotra
We can only make informed decisions if we have good information. That’s one of the reasons we try to share as much information as we can each day at 10almonds! But a lot will always depend on personalized information.
There are one-off (and sometimes potentially life-saving) things like health genomics:
The Real Benefit Of Genetic Testing
…but also smaller things that are informative on an ongoing basis, such as keeping track of your weight, your blood pressure, your hormones, and other metrics. You can even get fancy:
Track Your Blood Sugars For Better Personalized Health
Lifestyle is medicine
It’s often said that “food is medicine”. But also, movement is medicine. Sleep is medicine. In short, your lifestyle is the most powerful medicine that has ever existed.
Lifestyle encompasses very many things, but fortunately, there’s an “80:20 rule” in play that simplifies it a lot because if you take care of the top few things, the rest will tend to look after themselves:
These Top Few Things Make The Biggest Difference To Overall Health
Gratitude is better than fear
If we receive an unfavorable diagnosis (and let’s face it, most diagnoses are unfavorable), it might not seem like something to be grateful for.
But it is, insofar as it allows us to then take action! The information itself is what gives us our best chance of staying safe. And if that’s not possible e.g. in the worst case scenario, a terminal diagnosis, (bearing in mind that one of Dr. Malhotra’s three board certifications is in palliative care, so she sees this a lot), it at least gives us the information that allows us to make the best use of whatever remains to us.
See also: Managing Your Mortality
Which is very important!
…and/but possibly not the cheeriest note on which to end, so when you’ve read that, let’s finish today’s main feature on a happier kind of gratitude:
How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
Want to hear more from Dr. Malhotra?
Showing how serious she is about how our genes do not determine our destiny and knowledge is power, here she talks about her “previvor’s journey”, as she puts it, with regard to why she decided to have preventative cancer surgery in light of discovering her BRCA1 genetic mutation:
Click Here If The Embedded Video Doesn’t Load Automatically
Take care!
Share This Post
Related Posts
-
Mental illness, psychiatric disorder or psychological problem. What should we call mental distress?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We talk about mental health more than ever, but the language we should use remains a vexed issue.
Should we call people who seek help patients, clients or consumers? Should we use “person-first” expressions such as person with autism or “identity-first” expressions like autistic person? Should we apply or avoid diagnostic labels?
These questions often stir up strong feelings. Some people feel that patient implies being passive and subordinate. Others think consumer is too transactional, as if seeking help is like buying a new refrigerator.
Advocates of person-first language argue people shouldn’t be defined by their conditions. Proponents of identity-first language counter that these conditions can be sources of meaning and belonging.
Avid users of diagnostic terms see them as useful descriptors. Critics worry that diagnostic labels can box people in and misrepresent their problems as pathologies.
Underlying many of these disagreements are concerns about stigma and the medicalisation of suffering. Ideally the language we use should not cast people who experience distress as defective or shameful, or frame everyday problems of living in psychiatric terms.
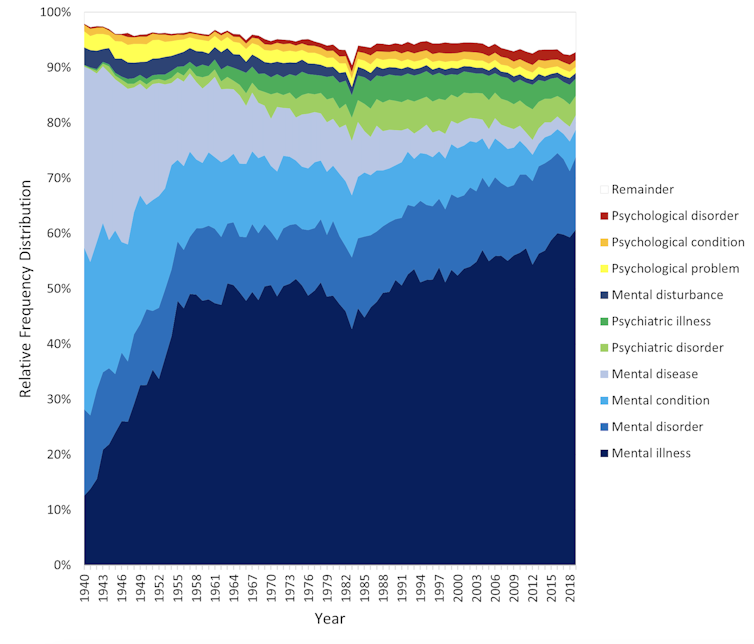
Our new research, published in the journal PLOS Mental Health, examines how the language of distress has evolved over nearly 80 years. Here’s what we found.
Engin Akyurt/Pexels Generic terms for the class of conditions
Generic terms – such as mental illness, psychiatric disorder or psychological problem – have largely escaped attention in debates about the language of mental ill health. These terms refer to mental health conditions as a class.
Many terms are currently in circulation, each an adjective followed by a noun. Popular adjectives include mental, mental health, psychiatric and psychological, and common nouns include condition, disease, disorder, disturbance, illness, and problem. Readers can encounter every combination.
These terms and their components differ in their connotations. Disease and illness sound the most medical, whereas condition, disturbance and problem need not relate to health. Mental implies a direct contrast with physical, whereas psychiatric implicates a medical specialty.
Mental health problem, a recently emerging term, is arguably the least pathologising. It implies that something is to be solved rather than treated, makes no direct reference to medicine, and carries the positive connotations of health rather than the negative connotation of illness or disease.
Is ‘mental health problem’ actually less pathologising? Monkey Business Images/Shutterstock Arguably, this development points to what cognitive scientist Steven Pinker calls the “euphemism treadmill”, the tendency for language to evolve new terms to escape (at least temporarily) the offensive connotations of those they replace.
English linguist Hazel Price argues that mental health has increasingly come to replace mental illness to avoid the stigma associated with that term.
How has usage changed over time?
In the PLOS Mental Health paper, we examine historical changes in the popularity of 24 generic terms: every combination of the nouns and adjectives listed above.
We explore the frequency with which each term appears from 1940 to 2019 in two massive text data sets representing books in English and diverse American English sources, respectively. The findings are very similar in both data sets.
The figure presents the relative popularity of the top ten terms in the larger data set (Google Books). The 14 least popular terms are combined into the remainder.
Relative popularity of alternative generic terms in the Google Books corpus. Haslam et al., 2024, PLOS Mental Health. Several trends appear. Mental has consistently been the most popular adjective component of the generic terms. Mental health has become more popular in recent years but is still rarely used.
Among nouns, disease has become less widely used while illness has become dominant. Although disorder is the official term in psychiatric classifications, it has not been broadly adopted in public discourse.
Since 1940, mental illness has clearly become the preferred generic term. Although an assortment of alternatives have emerged, it has steadily risen in popularity.
Does it matter?
Our study documents striking shifts in the popularity of generic terms, but do these changes matter? The answer may be: not much.
One study found people think mental disorder, mental illness and mental health problem refer to essentially identical phenomena.
Other studies indicate that labelling a person as having a mental disease, mental disorder, mental health problem, mental illness or psychological disorder makes no difference to people’s attitudes toward them.
We don’t yet know if there are other implications of using different generic terms, but the evidence to date suggests they are minimal.
The labels we use may not have a big impact on levels of stigma. Pixabay/Pexels Is ‘distress’ any better?
Recently, some writers have promoted distress as an alternative to traditional generic terms. It lacks medical connotations and emphasises the person’s subjective experience rather than whether they fit an official diagnosis.
Distress appears 65 times in the 2022 Victorian Mental Health and Wellbeing Act, usually in the expression “mental illness or psychological distress”. By implication, distress is a broad concept akin to but not synonymous with mental ill health.
But is distress destigmatising, as it was intended to be? Apparently not. According to one study, it was more stigmatising than its alternatives. The term may turn us away from other people’s suffering by amplifying it.
So what should we call it?
Mental illness is easily the most popular generic term and its popularity has been rising. Research indicates different terms have little or no effect on stigma and some terms intended to destigmatise may backfire.
We suggest that mental illness should be embraced and the proliferation of alternative terms such as mental health problem, which breed confusion, should end.
Critics might argue mental illness imposes a medical frame. Philosopher Zsuzsanna Chappell disagrees. Illness, she argues, refers to subjective first-person experience, not to an objective, third-person pathology, like disease.
Properly understood, the concept of illness centres the individual and their connections. “When I identify my suffering as illness-like,” Chappell writes, “I wish to lay claim to a caring interpersonal relationship.”
As generic terms go, mental illness is a healthy option.
Nick Haslam, Professor of Psychology, The University of Melbourne and Naomi Baes, Researcher – Social Psychology/ Natural Language Processing, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Foods Linked To Urinary Incontinence In Middle-Age (& Foods That Avert It)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Incontinence is an inconvenience associated with aging, especially for women. Indeed, as the study we’re going to talk about today noted:
❝Estrogen deficiency during menopause, aging, reproductive history, and factors increasing intra-abdominal pressure may lead to structural and functional failure in the pelvic floor.❞
However, that was just the “background”, before they got the study going, because…
❝Lifestyle choices, such as eating behavior, may contribute to pelvic floor disorders. The objective of the study was to investigate associations of eating behavior with symptoms of pelvic floor disorders, that is, stress urinary incontinence, urgency urinary incontinence, fecal incontinence, and constipation or defecation difficulties among middle-aged women.❞
~ Ibid.
How the study went
The researchers examined 1,098 Finnish women aged 47–55. It was a cross-sectional observational study, so no intervention was made, just: gathering data and analysing it. They examined:
- Eating behavior (i.e. what one’s diet is like; their questionnaire was quite comprehensive and the simplified conclusion doesn’t do that justice)
- Food consumption frequency (i.e. temporal patterns of eating)
- Demographic variables (e.g. age, education, etc)
- Gynecological variables (e.g. menopause status, hysterectomy, etc)
- Physical activity variables (e.g. light, moderate, heavy, previous history of no exercise, regular, competitive sport, etc)
With those things taken into account, the researchers crunched the numbers to assess the associations of dietary factors with pelvic floor disorders.
What they found
Adjusting for possible confounding variables…
- those with disordered eating patterns (e.g. overeating, restrictive eating, swinging between the two behaviors) were 50% higher chance of developing urinary incontinence than the norm
- those who more frequently consumed ready-made foods got 50% higher chance of developing urinary incontinence than the norm
- those who ate fruits daily enjoyed a 20% lower chance of urinary incontinence than the norm
So, in practical terms:
- practice mindful eating
- avoid ready-made foods
- enjoy fruit
You can read the paper in full here (it obviously goes into a lot more detail, and also covers other things beyond the scope of this article, such as fecal incontinence or, conversely, constipation—needless to say, the same advice stands in any case):
As for why this works the way it does: the study focused on the association and only hypothesized the question of “how”, but they did write a bit about that too, and it is almost certainly mostly a matter of gut health vs inflammation.
We really only have room for that kind of one-line summary here, but do read the paper if you’re interested, as it also talks about other dietary factors that had an impact, with the above-listed items being the topmost impactful factors, but for example (to take just one snippet of many possible ones):
❝In particular, saturated fatty acids (SFA) and cholesterol increased the risk for symptoms❞
~ Ibid. ← so do read it, for many more snippets like this!
What else does and doesn’t work
We covered a little while back the question of whether it is strengthening to hold one’s pee, or better to go whenever one feels the urge, and the answer is clear:
Meanwhile, supplements on the other hand are a mixed bag; there are some that probably help, and others, not so much:
What’s in the supplements that claim to help you cut down on bathroom breaks? And do they work?
Want to do more?
Check out these previous articles of ours:
Pelvic Floor Exercises (Not Kegels!) To Prevent Urinary Incontinence
and
Keeping Your Kidneys Happy: It’s About More Than Just Hydration! ← important at all ages, but especially relevant after 60
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Real Reason Most Women Don’t Lose Belly Fat
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Notwithstanding the title, this does also go for men too, by the way—while hormones count, they count differently. People with an estrogen-based metabolism (so usually: women) will usually have more body fat, which can make it harder to get visible muscletone, for those who want that. But people with a testosterone-based metabolism (so usually: men) will have different fat storage patterns, and belly-fat is more testosterone-directed than estrogen-directed (estrogen will tend to put it more to the thighs, butt, back, breasts, etc).
So the advice here is applicable to all…
Challenges and methods
The biggest barrier to success: many people give up when results are not immediate, especially if our body has been a certain way without change for a long time.
- “Oh, I guess it’s just genetics”
- “Oh, I guess it’s just age”
- “Oh, I guess it’s just because of [chronic condition]”
…and such things can be true! And yet, in each of the cases, persisting is still usually what the body needs.
So, should we give ourselves some “tough love” and force ourselves through discomfort?
Yes and no, Lefkowith says. It is important to be able to push through some discomfort, but it’s also important that whatever we’re doing should be sustainable—which means we do need to push, while also allowing ourselves adequate recovery time, and not taking unnecessary risks.
In particular, she advises to:
- remember that at least half the work is in the kitchen not the gym, and to focus more on adding protein than reducing calories
- enjoy a regular but varied core exercise routine
- stimulate blood flow to stubborn areas, which can aid in fat mobilization
- focus on getting nutrient-dense foods
- prioritize recovery and strategic rest
For more details on these things and more, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Visceral Belly Fat: What It Is & How To Lose It
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: