Hero Homemade Hummus
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you only have store-bought hummus at home, you’re missing out. The good news is that hummus is very easy to make, and highly customizable—so once you know how to make one, you can make them all, pretty much. And of course, it’s one of the healthiest dips out there!
You will need
- 2 x 140z/400g tins chickpeas
- 4 heaped tbsp tahini
- 3 tbsp extra virgin olive oil
- Juice of 1 lemon
- 1 tsp black pepper, coarse ground
- Optional, but recommended: your preferred toppings/flavorings. Examples to get you started include olives, tomatoes, garlic, red peppers, red onion, chili, cumin, paprika (please do not put everything in one hummus; if unsure about pairings, select just one optional ingredient per hummus for now)
Method
(we suggest you read everything at least once before doing anything)
1) Drain the chickpeas, but keep the chickpea water from them (also called aquafaba; it has many culinary uses beyond the scope of today’s recipe, but for now, just keep it to one side).
2) Add the chickpeas, ⅔ of the aquafaba, the tahini, the olive oil, the lemon juice, the black pepper, and any optional extra flavoring(s) that you don’t want to remain chunky. Blend until smooth; if it becomes to thick, add a little more aquafaba and blend again until it’s how you want it.
3) Transfer the hummus to a bowl, and add any extra toppings.
4) Repeat the above steps for each different kind of hummus you want to make.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat More (Of This) For Lower Blood Pressure
- All About Olive Oils
- Tasty Polyphenols
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
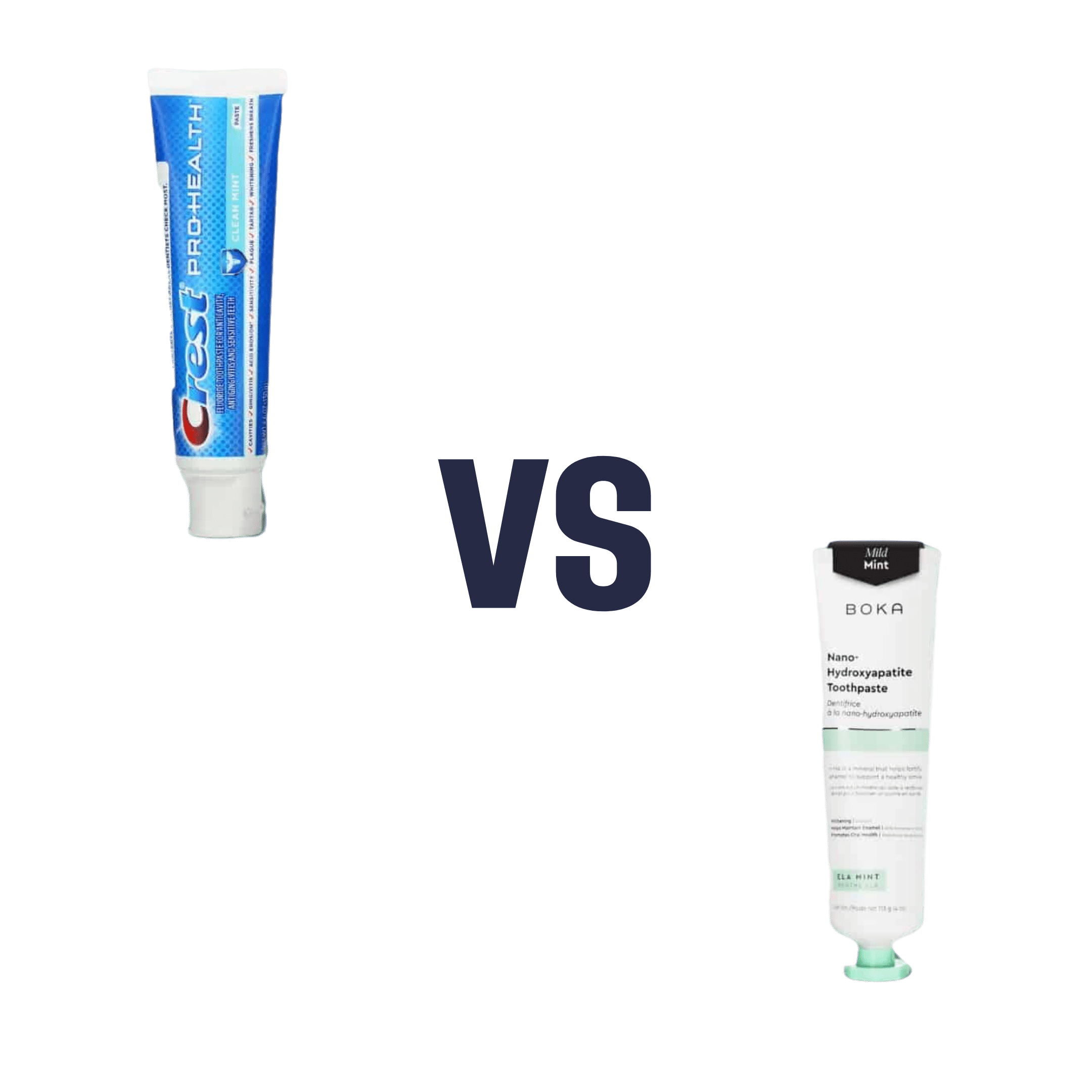
Fluoride Toothpaste vs Non-Fluoride Toothpaste – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing fluoride toothpaste to non-fluoride toothpaste, we picked the fluoride.
Why?
Fluoride is indeed toxic; that’s why it’s in toothpaste (to kill things; namely, bacteria whose waste products would harm our teeth). However, we are much bigger than those bacteria.
Given the amount of fluoride in toothpaste (usually under 1mg per strip of toothpaste to cover a toothbrush head), the amount that people swallow unintentionally (about 1/20th of that, so about 0.1mg daily if brushing teeth twice daily), and the toxicity level of fluoride (32–64mg/kg), then even if we take the most dangerous ends of all those numbers (and an average body size), to suffer ill effects from fluoride due to brushing your teeth, would require that you brush your teeth more than 23,000 times per day.
Alternatively, if you were to ravenously eat the toothpaste instead of spitting it out, you’d only need to brush your teeth a little over 1,000 times per day.
All the same, please don’t eat toothpaste; that’s not the message here.
However! In head-to-head tests, fluoride toothpaste has almost always beaten non-fluoride toothpaste.
Almost? Yes, almost: hydroxyapatite performed equally in one study, but that’s not usually an option on as many supermarket shelves.
We found some on Amazon, though, which is the one we used for today’s head-to-head. Here it is:
However, before you rush to buy it, do be aware that the toxicity of hydroxyapatite appears to be about twice that of fluoride:
Scientific Committee on Consumer Safety Opinion On Hydroxyapatite (Nano)
…which is still very safe (you’d need to brush your teeth, and eat all the toothpaste, about 500 times per day, to get to toxic levels, if we run with the same numbers we discussed before. Again, please do not do that, though).
But, since the science so far suggests it’s about twice as toxic as fluoride, then regardless of that still being very safe, the fluoride is obviously (by the same metric) twice as safe, hence picking the fluoride.
Want more options?
Check out our previous main feature:
Less Common Oral Hygiene Options
(the above article also links back to our discussion of different toothpastes and mouthwashes, by the way)
Take care!
Share This Post
-
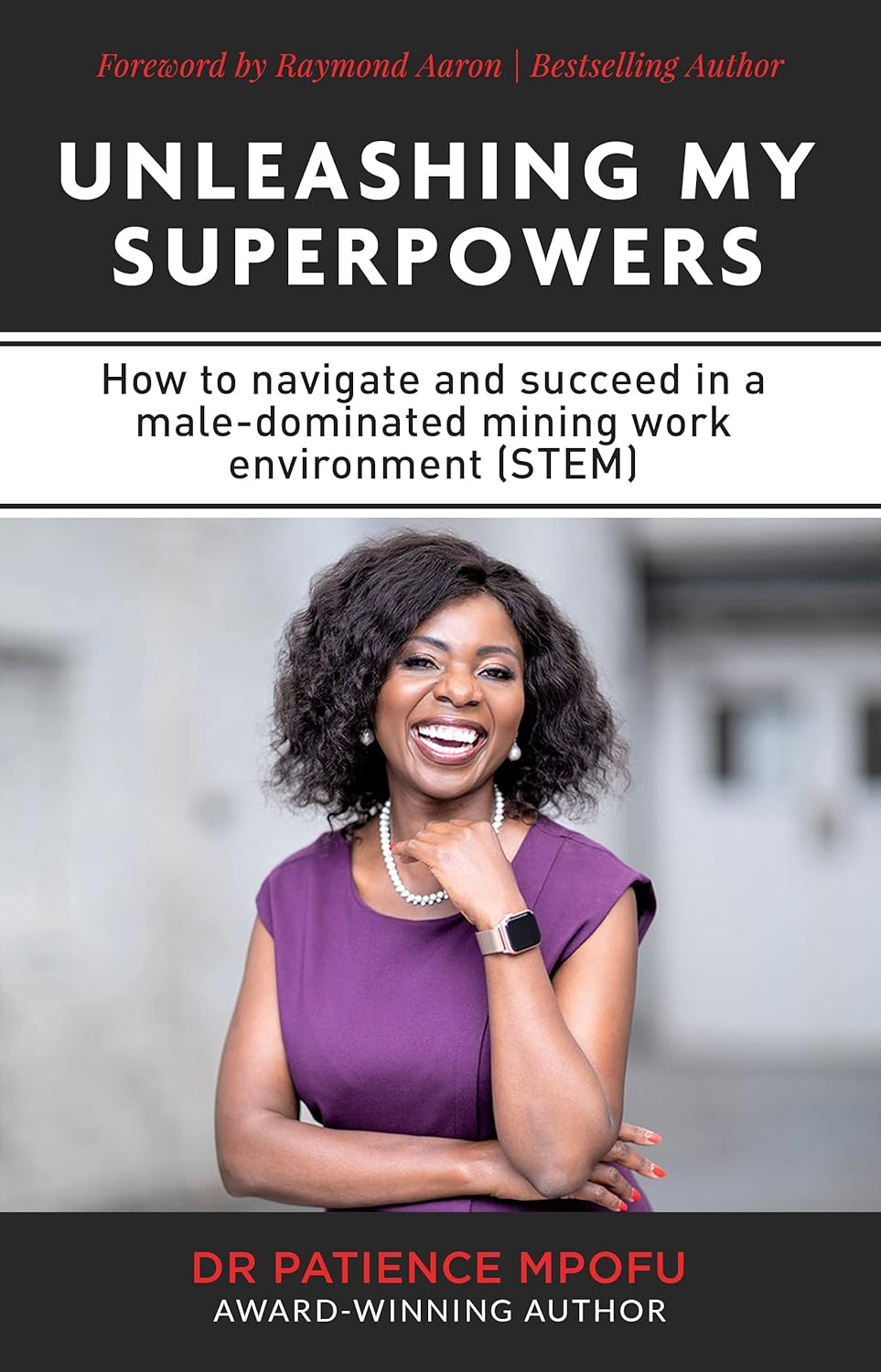
Unleashing My Superpowers – by Dr. Patience Mpofu
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Patience Mpofu is on a mission to provide women and girls with the inside-information, knowledge, resources, and strategies to break through the glass ceiling. She writes from her experience in STEM, but her lessons are applicable in any field.
Her advices range from the internal (how to deal with imposter syndrome) to the external (how to overcome cultural biases); she also explains and illustrates the importance of both role models and mentors.
While a lot of the book is half instruction manual, half memoir of her incredible life and career (to illustrate her points), and is well-worth reading—and/or perhaps worth gifting to a girl you know with ambitions in STEM?
Share This Post
-
The Power of Fun – by Catherine Price
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s said that nobody’s dying regret is to wish they’d spent more time at the office, yet many of don’t make enough time for fun.
This book has been published with two different subtitles:
- Why fun is the key to a happy and healthy life
- How to feel alive again
One offers a sensible reason to read this book; the other offers a deeply emotional reason. Both are entirely valid.
Catherine Price sets out in this work to identify what fun actually is (she puts it at the intersection of playfulness, connection and flow) and how to have more of it (she gives a five-step method to build and integrate it into life).
In the category of criticism, this 334-page book is (in this reviewer’s opinion) a little padded and could have been an article instead. But the advice contained within it is sound, and the impact it can have might be profound.
Bottom line: if you find you’ve settled into a routine that’s perhaps comfortable, but not actually that much fun, this book will help you to liven things up.
Click here to check out The Power Of Fun, and feel more alive!
Share This Post
Related Posts
-
Healthy Harissa Falafel Patties
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You can make these as regular falafel balls if you prefer, but patties are quicker and easier to cook, and are great for popping in a pitta.
You will need
For the falafels:
- 1 can chickpeas, drained, keep the chickpea water (aquafaba)
- 1 red onion, roughly chopped
- 2 tbsp chickpea flour (also called gram flour or garbanzo bean flour)
- 1 bunch parsley
- 1 tbsp harissa paste
- Extra virgin olive oil for frying
For the harissa sauce:
- ½ cup crème fraîche or plant-based equivalent (you can use our Plant-Based Healthy Cream Cheese recipe and add the juice of 1 lemon)*
- 1 tbsp harissa paste (or adjust this quantity per your heat preference)
*if doing this, rather than waste the zest of the lemon, you can add the zest to the falafels if you like, but it’s by no means necessary, just an option
For serving:
- Wholegrain pitta or other flatbread (you can use our Healthy Homemade Flatbreads recipe)
- Salad (your preference; we recommend some salad leaves, sliced tomato, sliced cucumber, maybe some sliced onion, that sort of thing)
Method
(we suggest you read everything at least once before doing anything)
1) Blend the chickpeas, 1 oz of the aquafaba, the onion, the parsley, and the harissa paste, until smooth. Then add in the chickpea flour until you get a thick batter. If you overdo it with the chickpea flour, add a little more of the aquafaba to equalize. Refrigerate the mixture for at least 30 minutes.
2) Heat some oil in a skillet, and spoon the falafel mixture into the pan to make the patties, cooking on both sides (you can use a spatula to gently turn them), and set them aside.
3) Mix the harissa sauce ingredients in a small bowl.
4) Assemble; best served warm, but enjoy it however you like!
Enjoy!
Want to learn more?
For those interested in more of what we have going on today:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Capsaicin For Weight Loss And Against Inflammation
- Hero Homemade Hummus ← another great option
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Basic Baked Tofu
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the main criticisms of tofu is that it is tasteless. Well, so is flour, but you’re not supposed to eat it plain, and the same goes for tofu. It’s a blank canvas that you get to decide what to do with—not to mention, it’s a canvas that’s very high in protein, and is a complete protein too, containing all essential amino acids. Anyway, here’s a starter recipe that elevates tofu from “nutrition” to “nutritious tasty snack”!
We were going to do a fancier recipe today, but considered that it might be judicious to cover this basic element first, that can be incorporated into a larger recipe later, a bit like we have done with recipes such as our Tasty Versatile Rice, and Plant-Based Healthy Cream Cheese (amongst others).
You will need
- 1 block of extra-firm tofu; these are quite standardized in size; it should be about 12oz; don’t worry if it’s a little more or less.
- 2 tbsp arrowroot powder (or potato starch if you don’t have arrowroot)
- 1½ tbsp extra virgin olive oil
- 1 tbsp nutritional yeast
- 1 tsp black pepper
- ½ tsp MSG or 1 tsp low-sodium salt
- Optional: ½ tsp garlic powder
- Optional: ½ tsp ground turmeric
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 425ºF / 220ºC.
2) Press the tofu for about 15 minutes (to remove excess moisture), using a tofu press if you have one. If you don’t, then here is an example product on Amazon, or alternatively, you can go with the time-honored tradition of cutting the tofu lengthways into slabs, and wrapping it in a lint-free kitchen towel or muslin cloth, and pressing it with heavy books. We don’t recommend pressing for more than about 15 minutes, as you are going to bake the tofu so you don’t want it too dry going in.
3) Cut the tofu into cubes. Size is up to you, but half-inch cubes are very respectable.
4) Combine the tofu cubes in a big bowl with the oil and seasonings, including the nutritional yeast but not the arrowroot powder or potato starch yet. You will need to toss them gently (very gently; they are fragile!) to combine.
5) Add the arrowroot powder or potato starch, and again toss gently to combine. We do this last, because it would stop the other things from sticking properly if we did it earlier.
6) Arrange the tofu on a baking tray lined with baking paper, in a single layer so that the cubes don’t touch. Bake for 15 minutes, turn them over, and bake for a further 15 minutes on the other side. They should now be golden and crisp, but if they’re not, just give them a little more time.
7) Serve as a snack, or set aside for whatever else you’re going to do with them in a larger more complex recipe.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Tofu vs Seitan – Which is Healthier?
- Plant vs Animal Protein: Head to Head
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Led by RFK Jr., Conservatives Embrace Raw Milk. Regulators Say It’s Dangerous.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In summertime, cows wait under a canopy to be milked at Mark McAfee’s farm in Fresno, California. From his Cessna 210 Centurion propeller plane, the 63-year-old can view grazing lands of the dairy company he runs that produces products such as unpasteurized milk and cheese for almost 2,000 stores.
Federal regulators say it’s risky business. Samples of raw milk can contain bird flu virus and other pathogens linked to kidney disease, miscarriages, and death.
McAfee, founder and CEO of the Raw Farm, who also leads the Raw Milk Institute, says he plans to soon be in a position to change that message.
Robert F. Kennedy Jr., the anti-vaccine activist President Donald Trump has tapped to run the Department of Health and Human Services, recruited McAfee to apply for a job as the FDA’s raw milk standards and policy adviser, McAfee said. McAfee has already written draft proposals for possible federal certification of raw dairy farms, he said.
Virologists are alarmed. The Centers for Disease Control and Prevention recommends against unpasteurized dairy that hasn’t been heated to kill pathogens such as bird flu. Interstate raw milk sales for human consumption are banned by the FDA. A Trump administration that weakens the ban or extols raw milk, the scientists say, could lead to more foodborne illness. It could also, they say, raise the risk of the highly pathogenic H5N1 bird flu virus evolving to spread more efficiently, including between people, possibly fueling a pandemic.
“If the FDA says raw milk is now legal and the CDC comes through and says it advises drinking raw milk, that’s a recipe for mass infection,” said Angela Rasmussen, a virologist and co-editor-in-chief of the medical journal Vaccine and an adjunct professor at Stony Brook University in New York.
The raw milk controversy reflects the broader tensions President Donald Trump will confront when pursuing his second-administration agenda of rolling back regulations and injecting more consumer choice into health care.
Many policies Kennedy has said he wants to revisit — from the fluoridation of tap water to nutrition guidance to childhood vaccine requirements — are backed by scientific research and were established to protect public health. Some physician groups and Democrats are gearing up to fight initiatives they say would put people at risk.
Raw milk has gained a following among anti-regulatory conservatives who are part of a burgeoning health freedom movement.
“The health freedom movement was adopted by the tea party, and conspiracy websites gave it momentum,” said Paul Offit, director of the Vaccine Education Center at Children’s Hospital of Philadelphia, who has studied the history of the anti-vaccine movement.
Once-fringe ideas are edging into the mainstream. Vaccine hesitancy is growing.
Arkansas, Utah, and Kentucky are weighing legislation that would relax or end requirements for fluoride in public water. And 30 states now allow for the sale of raw milk in some form within their borders.
While only an estimated 3% of the U.S. population consumes raw milk or cheese, efforts to try to restrict its sales have riled Republicans and provided grist for conservative podcasts.
Many conservatives denounced last year’s execution of a search warrant when Pennsylvania agriculture officials and state troopers arrived at an organic farm tucked off a two-lane road on Jan. 4, 2024. State inspectors were investigating cases of two children sickened by E. coli bacteria and sales of raw dairy from the operation owned by Amish farmer Amos Miller, according to a complaint filed by the state’s agricultural department.
Bundled in flannel shirts and winter jackets, the inspectors put orange stickers on products detaining them from sale, and they left toting product samples in large blue-and-white coolers, online videos show. The 2024 complaint against Miller alleged that he and his wife sold dairy products in violation of state law.
The farm was well known to regulators. They say in the complaint that a Florida consumer died after being sickened in 2014 with listeria bacteria found in raw dairy from Miller’s farm. The FDA said a raw milk sample from the farm indicates it was the “likely source” of the infection, based on the complaint.
Neither Miller’s farm nor his lawyer returned calls seeking comment.
The Millers’ attorney filed a preliminary objection that said “shutting down Defendants would cause inequitable harm, exceed the authority of the agency, constitute an excessive fine as well as disparate, discriminatory punishment, and contravene every essential Constitutional protection and powers reserved to the people of Pennsylvania.”
Regulators in Pennsylvania said in a press release they must protect the public, and especially children, from harm. “We cannot ignore the illnesses and further potential harm posed by distribution of these unregulated products,” the Pennsylvania agricultural department and attorney general said in a joint statement.
Unpasteurized dairy products are responsible for almost all the estimated 761 illnesses and 22 hospitalizations in the U.S. that occur annually because of dairy-related illness, according to a study published in the June 2017 issue of Emerging Infectious Diseases.
But conservatives say raiding an Amish farm is government overreach. They’re “harassing him and trying to make an example of him. Our government is really out of control,” Pennsylvania Republican Sen. Doug Mastriano said in a video he posted to Facebook.
Videos show protesters at a February 2024 hearing on Miller’s case included Amish men dressed in black with straw hats and locals waving homemade signs with slogans such as “FDA Go Away.” A court in March issued a preliminary injunction that barred Miller from marketing and selling raw dairy products within the commonwealth pending appeal, but the order did not preclude sales of raw milk to customers out of state. The case is ongoing.
With Kennedy, the raw milk debate is poised to go national. Kennedy wrote on X in October that the “FDA’s war on public health is about to end.” In the post, he pointed to the agency’s “aggressive suppression” of raw milk, as one example.
McAfee is ready. He wants to see a national raw milk ordinance, similar to one that exists for pasteurized milk, that would set minimal national standards. Farmers could attain certification through training, continuing education, and on-site pathogen testing, with one standard for farms that sell to consumers and another for retail sales.
The Trump administration didn’t return emails seeking comment.
McAfee has detailed the system he developed to ensure his raw dairy products are safe. He confirmed the process for KFF Health News: cows with yellow-tagged ears graze on grass pastures and are cleansed in washing pens before milking. The raw dairy is held back from consumer sale until it’s been tested and found clear of pathogens.
His raw dairy products, such as cheese and milk, are sold by a variety of stores, including health, organic, and natural grocery chains, according to the company website, as well as raw dairy pet products, which are not for human consumption.
He said he doesn’t believe the raw milk he sells could contain or transmit viable bird flu virus. He also said he doesn’t believe regulators’ warnings about raw milk and the virus.
“The pharmaceutical industry is trying to create a new pandemic from bird flu to get their stock back up,” said McAfee, who says he counts Kennedy as a customer. His view is not shared by leading virologists.
In December, the state of California secured a voluntary recall of all his company’s raw milk and cream products due to possible bird flu contamination.
Five indoor cats in the same household died or were euthanized in December after drinking raw milk from McAfee’s farm, and tests on four of the animals found they were infected with bird flu, according to the Los Angeles County Department of Health.
In an unrelated case, Joseph Journell, 56, said three of his four indoor cats drank McAfee’s raw milk. Two fell sick and died, he said. His third cat, a large tabby rescue named Big Boy, temporarily lost the use of his hind legs and had to use a specialized wheelchair device, he said. Urine samples from Big Boy were positive for bird flu, according to a copy of the results from Cornell University and the U.S. Department of Agriculture.
McAfee dismissed connections between the cats’ illnesses and his products, saying any potential bird flu virus would no longer be viable by the time his raw milk gets to stores. He also said he believes that any sick cats got bird flu from recalled pet food.
Journell said he has hired a lawyer to try to recover his veterinary costs but remains a staunch proponent of raw milk.
“Raw milk is good for you, just not if it has bird flu in it,” he said. “I do believe in its healing powers.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: