Hair Growth: Caffeine and Minoxidil Strategies
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Questions and Answers at 10almonds
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Hair growth strategies for men combing caffeine and minoxidil?
Well, the strategy for that is to use caffeine and minoxidil! Some more specific tips, though:
- Both of those things need to be massaged (gently!) into your scalp especially around your hairline.
- In the case of caffeine, that boosts hair growth. No extra thought or care needed for that one.
- In the case of minoxidil, it reboots the hair growth cycle, so if you’ve only recently started, don’t be surprised (or worried) if you see more shedding in the first three months. It’s jettisoning your old hairs because new ones were just prompted (by the minoxidil) to start growing behind them. So: it will get briefly worse before it gets better, but then it’ll stay better… provided you keep using it.
- If you’d like other options besides minoxidil, finasteride is a commonly prescribed oral drug that blocks the conversion of testosterone to DHT, which latter is what tells your hairline to recede.
- If you’d like other options besides prescription drugs, saw palmetto performs comparably to finasteride (and works the same way).
- You may also want to consider biotin supplementation if you don’t already enjoy that
- Consider also using a dermaroller on your scalp. If you’re unfamiliar, this is a device that looks like a tiny lawn aerator, with many tiny needles, and you roll it gently across your skin.
- It can be used for promoting hair growth, as well as for reducing wrinkles and (more slowly) healing scars.
- It works by breaking up the sebum that may be blocking new hair growth, and also makes the skin healthier by stimulating production of collagen and elastin (in response to the thousands of microscopic wounds that the needles make).
- Sounds drastic, but it doesn’t hurt and doesn’t leave any visible marks—the needles are that tiny. Still, practise good sterilization and ensure your skin is clean when using it.
See: How To Use A Dermaroller ← also explains more of the science of it
PS: this question was asked in the context of men, but the information goes the same for women suffering from androgenic alepoceia—which is a lot more common than most people think!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Reason You’re Alone
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you are feeling lonely, then there are likely reasons why, as Kurtzgesagt explains:
Why it happens and how to fix it
Many people feel lonely and disconnected, often not knowing how to make new friends. And yet, social connection strongly predicts happiness, while lack of it is linked to diseases and a shorter life.
One mistake that people make is thinking it has to be about shared interests; that can help, but proximity and shared time are much more important.
Another stumbling block for many is that adult responsibilities and distractions (work, kids, technology) often take priority over friendships—but loneliness is surprisingly highest among young people, worsened by the pandemic’s impact on social interactions.
And even when friendships are made, they fade without attention, often accidentally, impacting both people involved. Other friendships can be lost following big life changes such as moving house or the end of a relationship. And for people above a certain advanced age, friendship groups can shrink due to death, if one’s friends are all in the same age group.
But, all is not lost. We can make friends with people of any age, and old friendships can be revived by a simple invitation. We can also take a “build it and they will come” approach, by organizing events and being the one who invites others.
It’s easy to fear rejection—most people do—but it’s worth overcoming for the potential rewards. That said, building friendships requires time, patience, caring about others, and being open about yourself, which can involve a degree of vulnerability too.
In short: be laid-back while still prioritizing friendships, show genuine interest, and stay open to social opportunities.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Beat Loneliness & Isolation
Take care!
Share This Post
-
We’re only using a fraction of health workers’ skills. This needs to change
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Roles of health professionals are still unfortunately often stuck in the past. That is, before the shift of education of nurses and other health professionals into universities in the 1980s. So many are still not working to their full scope of practice.
There has been some expansion of roles in recent years – including pharmacists prescribing (under limited circumstances) and administering a wider range of vaccinations.
But the recently released paper from an independent Commonwealth review on health workers’ “scope of practice” identifies the myriad of barriers preventing Australians from fully benefiting from health professionals’ skills.
These include workforce design (who does what, where and how roles interact), legislation and regulation (which often differs according to jurisdiction), and how health workers are funded and paid.
There is no simple quick fix for this type of reform. But we now have a sensible pathway to improve access to care, using all health professionals appropriately.
A new vision for general practice
I recently had a COVID booster. To do this, I logged onto my general practice’s website, answered the question about what I wanted, booked an appointment with the practice nurse that afternoon, got jabbed, was bulk-billed, sat down for a while, and then went home. Nothing remarkable at all about that.
But that interaction required a host of facilitating factors. The Victorian government regulates whether nurses can provide vaccinations, and what additional training the nurse requires. The Commonwealth government has allowed the practice to be paid by Medicare for the nurse’s work. The venture capitalist practice owner has done the sums and decided allocating a room to a practice nurse is economically rational.
The future of primary care is one involving more use of the range of health professionals, in addition to GPs.
It would be good if my general practice also had a physiotherapist, who I could see if I had back pain without seeing the GP, but there is no Medicare rebate for this. This arrangement would need both health professionals to have access to my health record. There also needs to be trust and good communication between the two when the physio might think the GP needs to be alerted to any issues.
This vision is one of integrated primary care, with health professionals working in a team. The nurse should be able to do more than vaccination and checking vital signs. Do I really need to see the GP every time I need a prescription renewed for my regular medication? This is the nub of the “scope of practice” issue.
How about pharmacists?
An integrated future is not the only future on the table. Pharmacy owners especially have argued that pharmacists should be able to practise independently of GPs, prescribing a limited range of medications and dispensing them.
This will inevitably reduce continuity of care and potentially create risks if the GP is not aware of what other medications a patient is using.
But a greater role for pharmacists has benefits for patients. It is often easier and cheaper for the patient to see a pharmacist, especially as bulk billing rates fall, and this is one of the reasons why independent pharmacist prescribing is gaining traction.
It’s often easier for a patient to see a pharmacist than a GP. PeopleImages.com – Yuri A/Shutterstock Every five years or so the government negotiates an agreement with the Pharmacy Guild, the organisation of pharmacy owners, about how much pharmacies will be paid for dispensing medications and other services. These agreements are called “Community Pharmacy Agreements”. Paying pharmacists independent prescribing may be part of the next agreement, the details of which are currently being negotiated.
GPs don’t like competition from this new source, even though there will be plenty of work around for GPs into the foreseeable future. So their organisations highlight the risks of these changes, reopening centuries old turf wars dressed up as concerns about safety and risk.
Who pays for all this?
Funding is at the heart of disputes about scope of practice. As with many policy debates, there is merit on both sides.
Clearly the government must increase its support for comprehensive general practice. Existing funding of fee-for-service medical benefits payments must be redesigned and supplemented by payments that allow practices to engage a range of other health professionals to create health-care teams.
This should be the principal direction of primary care reform, and the final report of the scope of practice review should make that clear. It must focus on the overall goal of better primary care, rather than simply the aspirations of individual health professionals, and working to a professional’s full scope of practice in a team, not a professional silo.
In parallel, governments – state and federal – must ensure all health professionals are used to their best of their abilities. It is a waste to have highly educated professionals not using their skills fully. New funding arrangements should facilitate better access to care from all appropriately qualified health professionals.
In the case of prescribing, it is possible to reconcile the aspirations of pharmacists and the concerns of GPs. New arrangements could be that pharmacists can only renew medications if they have agreements with the GP and there is good communication between them. This may be easier in rural and suburban areas, where the pharmacists are better known to the GPs.
The second issues paper points to the complexity of achieving scope of practice reforms. However, it also sets out a sensible path to improve access to care using all health professionals appropriately.
Stephen Duckett, Honorary Enterprise Professor, School of Population and Global Health, and Department of General Practice and Primary Care, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
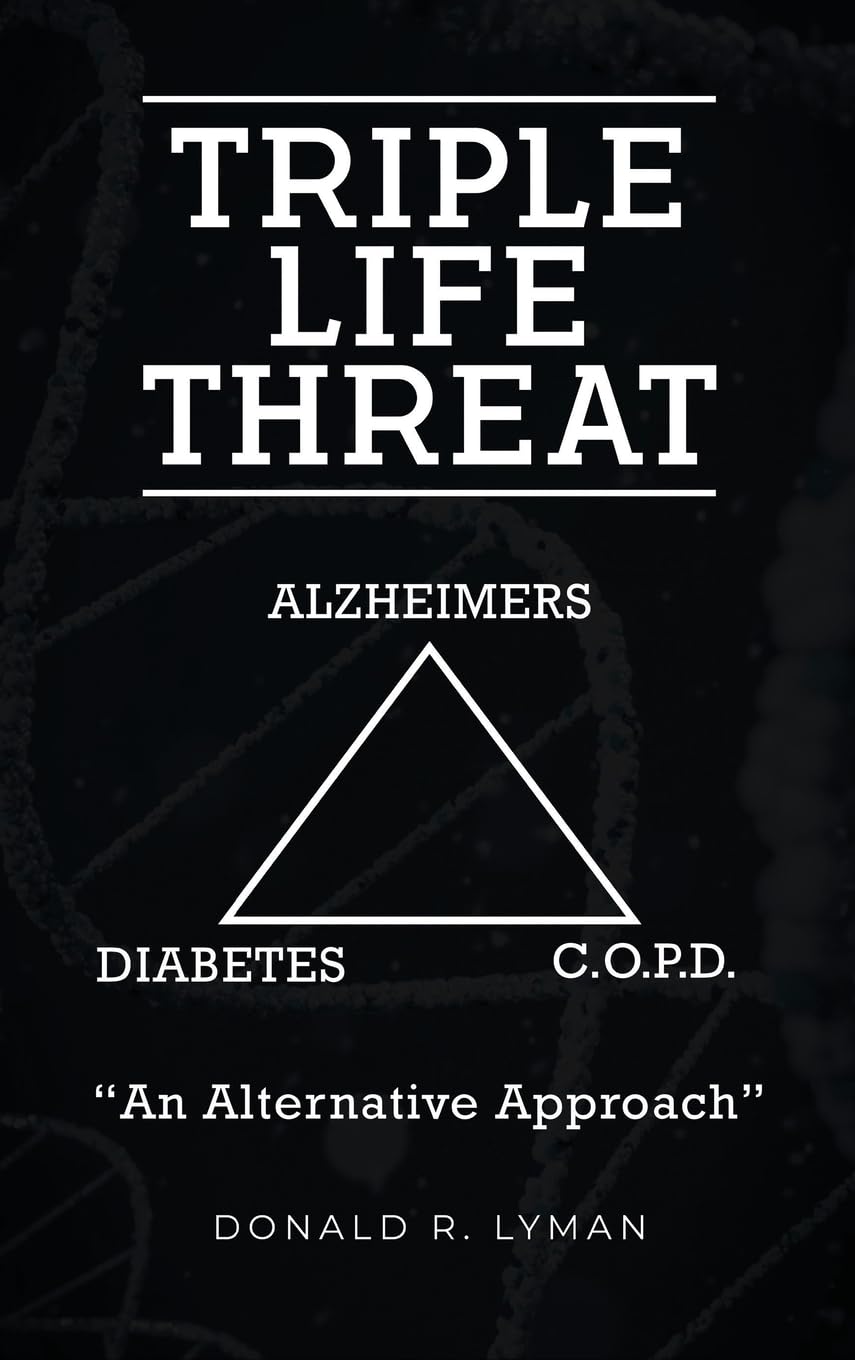
Triple Life Threat – by Donald R. Lyman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book takes a similar approach to “How Not To Die” (which we featured previously), but focussed specifically on three things, per the title: chronic pulmonary obstructive disease (CPOD), diabetes (type 2), and Alzheimer’s disease.
Lyman strikes a great balance of being both information-dense and accessible; there’s a lot of reference material in here, and the reader is not assumed to have a lot of medical knowledge—but we’re not patronized either, and this is an informative manual, not a sensationalized scaremongering piece.
All in all… if you have known risk factors for one or more of three diseases this book covers, the information within could well be a lifesaver.
Share This Post
Related Posts
-
Ayurveda’s Contributions To Science
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ayurveda’s Contributions To Science (Without Being Itself Rooted in Scientific Method)
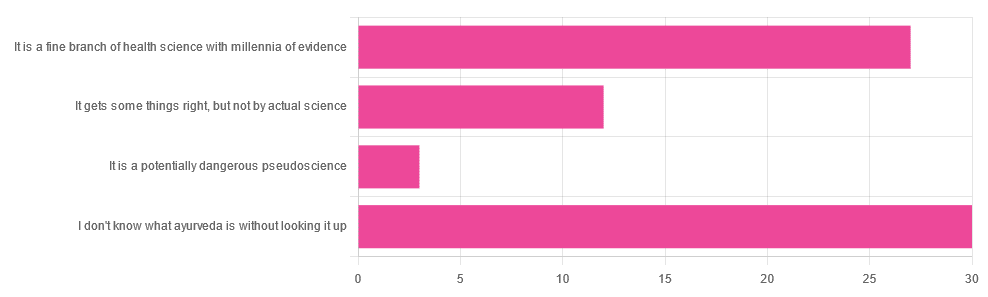
Yesterday, we asked you for your opinions on ayurveda, and got the above-depicted, below-described, set of responses. Of those who responded…
- A little over 41% said “I don’t know what ayurveda is without looking it up”
- A little over 37% said “It is a fine branch of health science with millennia of evidence”
- A little over 16% said “It gets some things right, but not by actual science”
- A little over 4% said “It is a potentially dangerous pseudoscience”
So, what does the science say?
Ayurveda is scientific: True or False?
False, simply. Let’s just rip the band-aid off in this case. That doesn’t mean it’s necessarily without merit, though!
Let’s put it this way:
- If you drink coffee to feel more awake because scientific method has discerned that caffeine has vasoconstrictive and adenosine-blocking effects while also promoting dopaminergic activity, then your consumption of coffee is evidence-based and scientific. Great!
- If you drink coffee to feel more awake because somebody told you that that somebody told them that it energizes you by balancing the elements fire (the heat of the coffee), air (the little bubbles on top), earth (the coffee grinds), water (the water), and ether (steam), then that is neither evidence-based nor scientific, but it will still work exactly the same.
Ayurveda is a little like that. It’s an ancient traditional Indian medicine, based on a combination of anecdotal evidence and supposition.
- The anecdotal evidence from ayurveda has often resulted in herbal remedies that, in modern scientific trials, have been found to have merit.
- Ayurvedic meditative practices also have a large overlap with modern mindfulness practices, and have also been found to have merit
- Ayurveda also promotes the practice of yoga, which is indeed a very healthful activity
- The supposition from ayurveda is based largely in those five elements we mentioned above, as well as a “balancing of humors” comparable to medieval European medicine, and from a scientific perspective, is simply a hypothesis with no evidence to support it.
Note: while ayurveda is commonly described as a science by its practitioners in the modern age, it did not originally claim to be scientific, but rather, wisdom handed down directly by the god Dhanvantari.
Ayurveda gets some things right: True or False?
True! Indeed, we covered some before in 10almonds; you may remember:
Bacopa Monnieri: A Well-Evidenced Cognitive Enhancer
(Bacopa monnieri is also known by its name in ayurveda, brahmi)
There are many other herbs that have made their way from ayurveda into modern science, but the above is a stand-out example. Others include:
- Ashwagandha: The Root of All Even-Mindedness?
- Boswellia serrata (Frankincense) Against Pain and Depression/Anxiety
Yoga and meditation are also great, and not only that, but great by science, for example:
- NCCIH | Yoga for Health: Clinical Guidelines, Scientific Literature, Info for Patients
- The Neuroscience of Mindfulness: How Mindfulness Alters the Brain and Facilitates Emotion Regulation
Ayurveda is a potentially dangerous pseudoscience: True or False?
Also True! We covered why it’s a pseudoscience above, but that doesn’t make it potentially dangerous, per se (you’ll remember our coffee example).
What does, however, make it potentially dangerous (dose-dependent) is its use of heavy metals such as lead, mercury, and arsenic:
Heavy Metal Content of Ayurvedic Herbal Medicine Products
Some final thoughts…
Want to learn more about the sometimes beneficial, sometimes uneasy relationship between ayurveda and modern science?
A lot of scholarly articles trying to bridge (or further separate) the two were very biased one way or the other.
Instead, here’s one that’s reasonably optimistic with regard to ayurveda’s potential for good, while being realistic about how it currently stands:
Development of Ayurveda—Tradition to trend
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What You Should Have Been Told About The Menopause Beforehand
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What You Should Have Been Told About Menopause Beforehand
This is Dr. Jen Gunter. She’s a gynecologist, specializing in chronic pain and vulvovaginal disorders. She’s also a woman on a mission to demystify things that popular culture, especially in the US, would rather not talk about.
When was the last time you remember the menopause being referenced in a movie or TV show? If you can think of one at all, was it just played for laughs?
And of course, the human body can be funny, so that’s not necessarily the problem, but it sure would be nice if that weren’t all that there is!
So, what does Dr. Gunter want us to know?
It’s a time of changes, not an end
The name “menopause” is misleading. It’s not a “pause”, and those menses aren’t coming back.
And yet, to call it a “menostop” would be differently misleading, because there’s a lot more going on than a simple cessation of menstruation.
Estrogen levels will drop a lot, testosterone levels may rise slightly, mood and sleep and appetite and sex drive will probably be affected (progesterone can improve all these things!) and
not to mention butwe’re going to mention: vaginal atrophy, which is very normal and very treatable with a topical estrogen cream. Untreated menopause can also bring a whole lot of increased health risks (for example, heart disease, osteoporosis, and, counterintuitively given the lower estrogen levels, breast cancer).However, with a little awareness and appropriate management, all these things can usually be navigated with minimal adverse health outcomes.
Dr Gunter, for this reason, refers to it interchangeably as “the menopausal transition”. She describes it as being less like a cliff edge we fall off, and more like a bridge we cross.
Bridges can be dangerous to cross! But they can also get us safely where we’re going.
Ok, so how do we manage those things?
Dr. Gunter is a big fan of evidence-based medicine, so we’ll not be seeing any yonic crystals or jade eggs. Or “goop”.
See also: Meet Goop’s Number One Enemy
For most people, she recommends Menopausal Hormone Therapy (MHT), which falls under the more general category of Hormone Replacement Therapy (HRT).
This is the most well-evidenced, science-based way to avoid most of the risks associated with menopause.
Nevertheless, there are scare-stories out there, ranging from painful recommencement of bleeding, to (once again) increased risk of breast cancer. However, most of these are either misunderstandings, or unrelated to menopause and MHT, and are rather signs of other problems that should not be ignored.
To get a good grounding in this, you might want to read her Hormone Therapy Guide, freely available as a standalone section on her website. This series of posts is dedicated to hormone therapy. It starts with some basics and builds on that knowledge with each post:
Dr. Gunter’s Guide To The Hormone Menoverse
What about natural therapies?
There are some non-hormonal things that work, but these are mostly things that:
- give a statistically significant reduction in symptoms
- give the same statistically significant reduction in symptoms as placebo
As Dr. Gunter puts it:
❝While most of the studies of prescription medications for hot flashes have an appropriate placebo arm, this is rarely the case with so-called alternative therapies.
In fact, the studies here are almost always low quality, so it’s often not possible to conclude much.
Many reviews that look at these studies often end with a line that goes something like, “Randomized trials with a placebo arm, a low risk of bias, and adequate sample sizes are urgently needed.”
You should interpret this kind of conclusion as the polite way of saying, “We need studies that aren’t BS to say something constructive.”❞
However, if it works, it works, whatever its mechanism. It’s just good, when making medical decisions, to do so with the full facts!
For that matter, even Dr. Gunter acknowledges that while MHT can be lifechanging (in a positive way) for many, it’s not for everyone:
Informed Decisions: When Menopause Hormone Therapy Isn’t Recommended
Want to know more?
Dr. Gunter also has an assortment of books available, including The Menopause Manifesto (which we’ve reviewed previously), and some others that we haven’t, such as “Blood” and “The Vagina Bible”.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s the difference between heat exhaustion and heat stroke? One’s a medical emergency
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When British TV doctor Michael Mosley died last year in Greece after walking in extreme heat, local police said “heat exhaustion” was a contributing factor.
Since than a coroner could not find a definitive cause of death but said this was most likely due to an un-identified medical reason or heat stroke.
Heat exhaustion and heat stroke are two illnesses that relate to heat.
So what’s the difference?
Studio Nut/Shutterstock A spectrum of conditions
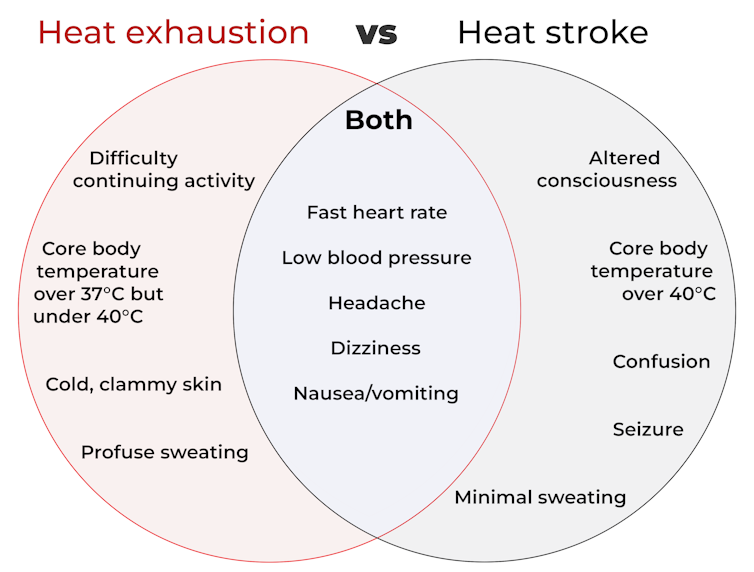
Heat-related illnesses range from mild to severe. They’re caused by exposure to excessive heat, whether from hot conditions, physical exertion, or both. The most common ones include:
- heat oedema: swelling of the hands, feet and ankles
- heat cramps: painful, involuntary muscle spasms usually after exercise
- heat syncope: fainting due to overheating
- heat exhaustion: when the body loses water due to excessive sweating, leading to a rise in core body temperature (but still under 40°C). Symptoms include lethargy, weakness and dizziness, but there’s no change to consciousness or mental clarity
- heat stroke: a medical emergency when the core body temperature is over 40°C. This can lead to serious problems related to the nervous system, such as confusion, seizures and unconsciousness including coma, leading to death.
As you can see from the diagram below, some symptoms of heat stroke and heat exhaustion overlap. This makes it hard to recognise the difference, even for medical professionals.
CC BY-SA How does this happen?
The human body is an incredibly efficient and adaptable machine, equipped with several in-built mechanisms to keep our core temperature at an optimal 37°C.
But in healthy people, regulation of body temperature begins to break down when it’s hotter than about 31°C with 100% humidity (think Darwin or Cairns) or about 38°C with 60% humidity (typical of other parts of Australia in summer).
This is because humid air makes it harder for sweat to evaporate and take heat with it. Without that cooling effect, the body starts to overheat.
Once the core temperature rises above 37°C, heat exhaustion can set in, which can cause intense thirst, weakness, nausea and dizziness.
If the body heat continues to build and the core body temperature rises above 40°C, a much more severe heat stroke could begin. At this point, it’s a life-threatening emergency requiring immediate medical attention.
At this temperature, our proteins start to denature (like an egg on a hotplate) and blood flow to the intestines stops. This makes the gut very leaky, allowing harmful substances such as endotoxins (toxic substances in some bacteria) and pathogens (disease causing microbes) to leak into the bloodstream.
The liver can’t detoxify these fast enough, leading to the whole body becoming inflamed, organs failing, and in the worst-case scenario, death.
Who’s most at risk?
People doing strenuous exercise, especially if they’re not in great shape, are among those at risk of heat exhaustion or heat stroke. Others at risk include those exposed to high temperatures and humidity, particularly when wearing heavy clothing or protective gear.
Outdoor workers such as farmers, firefighters and construction workers are at higher risk too. Certain health conditions, such as diabetes, heart disease, or lung conditions (such as COPD or chronic obstructive pulmonary disease), and people taking blood pressure medications, can also be more vulnerable.
Adults over 65, infants and young children are especially sensitive to heat as they are less able to physically cope with fluctuations in heat and humidity.
Firefighters are among those at risk of heat-related illness. structuresxx/Shutterstock How are these conditions managed?
The risk of serious illness or death from heat-related conditions is very low if treatment starts early.
For heat exhaustion, have the individual lie down in a cool, shady area, loosen or remove excess clothing, and cool them by fanning, moistening their skin, or immersing their hands and feet in cold water.
As people with heat exhaustion almost always are dehydrated and have low electrolytes (certain minerals in the blood), they will usually need to drink fluids.
However, emergency hospital care is essential for heat stroke. In hospital, health professionals will focus on stabilising the patient’s:
- airway (ensure no obstructions, for instance, vomit)
- breathing (look for signs of respiratory distress or oxygen deprivation)
- circulation (check pulse, blood pressure and signs of shock).
Meanwhile, they will use rapid-cooling techniques including immersing the whole body in cold water, or applying wet ice packs covering the whole body.
Take home points
Heat-related illnesses, such as heat stroke and heat exhaustion, are serious health conditions that can lead to severe illness, or even death.
With climate change, heat-related illness will become more common and more severe. So recognising the early signs and responding promptly are crucial to prevent serious complications.
Matthew Barton, Senior lecturer, School of Nursing and Midwifery, Griffith University and Michael Todorovic, Associate Professor of Medicine, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: