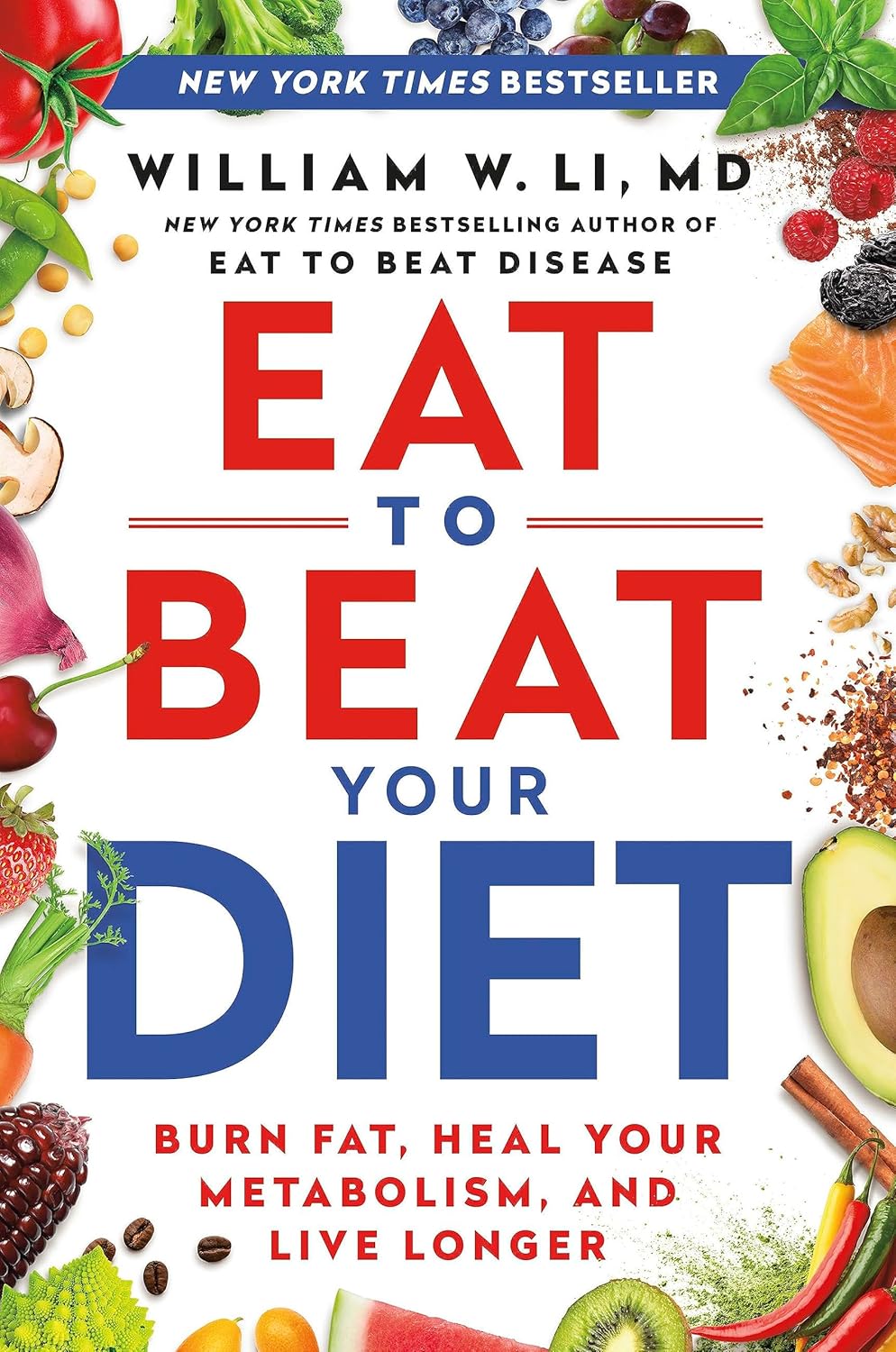
Eat to Beat Your Diet – by Dr. William Li
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed Dr. Li’s excellent “Eat To Beat Disease”, so you may be wondering how much overlap there is. While he does still cover such topics as angiogenesis, organ regeneration, microbiome health, DNA protection, and immunological considerations, and much of the dietary advice is similar, most of the explanation is different.
Because, this time, rather than looking at beating disease in general, there’s a much stronger focus on metabolic disease in particular, and yes, for those who want to do so, losing fat.
The scientific explanations are in-depth, such that you come way with not merely “I should eat an avocado once in a while”, but a comprehensive understanding of the body’s metabolic processes, from the chemistry to the organs involved, from the cellular to the systemic.
The style is on the hard end of pop-science. It’s approachably readable, while having a lot of densely-packed information with minimal fluff. You will be more than getting your money’s worth out of its 496 pages.
Bottom line: if you’d like to perk up your metabolism with a dietary approach that’s enjoyable and very restrictive, then this book will arm you with the knowledge to do that.
Click here to check out Eat To Beat Your Diet, and eat to beat your diet!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tasty Hot-Or-Cold Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Full of fiber as well as vitamins and minerals, this versatile “serve it hot or cold” soup is great whatever the weather—give it a try!
You will need
- 1 quart low-sodium vegetable stock—ideally you made this yourself from vegetable offcuts you kept in the freezer until you had enough to boil in a big pan, but failing that, a large supermarket will generally be able to sell you low-sodium stock cubes.
- 2 medium potatoes, peeled and diced
- 2 leeks, chopped
- 2 stalks celery, chopped
- 1 large onion, diced
- 1 large carrot, diced, or equivalent small carrots, sliced
- 1 zucchini, diced
- 1 red bell pepper, diced
- 1 tsp rosemary
- 1 tsp thyme
- ¼ bulb garlic, minced
- 1 small piece (equivalent of a teaspoon) ginger, minced
- 1 tsp red chili flakes
- 1 tsp black pepper, coarse ground
- ½ tsp turmeric
- Extra virgin olive oil, for frying
- Optional: ½ tsp MSG or 1 tsp low-sodium salt
About the MSG/salt: there should be enough sodium already from the stock and potatoes, but in case there’s not (since not all stock and potatoes are made equal), you might want to keep this on standby.
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a sauté pan, and add the diced onion, frying until it begins to soften.
2) Add the ginger, potato, carrot, and leek, and stir for about 5 minutes. The hard vegetables won’t be fully cooked yet; that’s fine.
3) Add the zucchini, red pepper, celery, and garlic, and stir for another 2–3 minutes.
4) Add the remaining ingredients; seasonings first, then vegetable stock, and let it simmer for about 15 minutes.
5) Check the potatoes are fully softened, and if they are, it’s ready to serve if you want it hot. Alternatively, let it cool, chill it in the fridge, and enjoy it cold:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat More (Of This) For Lower Blood Pressure
- Our Top 5 Spices: How Much Is Enough For Benefits? ← 5/5 in our recipe today!
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
Take care!
Share This Post
-
Age Later – by Dr. Nir Barzilai
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Barzilai discusses why we age, why supercentenarians age more slowly, and even, why it is so often the case that supercentenarians outside of Blue Zones have poor lifestyles (their longevity is because of protective genes that mitigate the harmful effects of those poor lifestyles—the ultimate in “survivorship bias”).
He also talks not just genetics, but also epigenetics, and thus gene expression. Bearing in mind, there’s a scale of modifiability there: with current tech, we can’t easily change a bad gene… But we often can just switch it off (or at least downregulate its expression). This is where studies in supercentenarians are helpful even for those who don’t have such fortunate genes—the supercentenarian studies show us which genes we want on or off, what gene expressions to aim for, etc. Further clinical studies can then show us what lifestyle interventions (exercise, diet, nutraceuticals, etc) can do that for us.
With regard to those lifestyle interventions, he does cover many, and that’s where a lot of the practical value of the book comes from. But it’s not just “do this, do that”; understanding the reasons behind why things work the way they do is important, so as to be more likely to do it right, and also to enjoy greater adherence (we tend to do things we understand more readily than things we have just been told to do).
There are areas definitely within the author’s blind spots—for example, when talking about menopausal HRT, he discusses at great length the results of the discredited WHI study, and considers it the only study of relevance. So, this is a reminder to not believe everything said by someone who sounds confident (Dr. Barzilai’s professional background is mostly in treating diabetes).
In terms of style, it is very much narrative; somewhat pop-science, but more “this doctor wants to tell stories”. So many stories. Now, the stories all have informational value, so this isn’t padding, but it is the style, so we mention it as such. As for citations, there aren’t any, so if you want to look up the science he mentions, you’re going to need a bit of digital sleuthery to find the papers from the clues in the stories.
Bottom line: if you’re interested in the science of aging and how that has been progressing for the past decades and where we’re at, this book will give you so many jumping-off points, and is an engaging read.
Share This Post
-
Accidental falls in the older adult population: What academic research shows
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Accidental falls are among the leading causes of injury and death among adults 65 years and older worldwide. As the aging population grows, researchers expect to see an increase in the number of fall injuries and related health spending.
Falls aren’t unique to older adults. Nealy 684,000 people die from falls each year globally. Another 37.3 million people each year require medical attention after a fall, according to the World Health Organization. But adults 65 and older account for the greatest number of falls.
In the United States, more than 1 in 4 older adults fall each year, according to the National Institute on Aging. One in 10 report a fall injury. And the risk of falling increases with age.
In 2022, health care spending for nonfatal falls among older adults was $80 billion, according to a 2024 study published in the journal Injury Prevention.
Meanwhile, the fall death rate in this population increased by 41% between 2012 and 2021, according to the latest CDC data.
“Unfortunately, fall-related deaths are increasing and we’re not sure why that is,” says Dr. Jennifer L. Vincenzo, an associate professor at the University of Arkansas for Medical Sciences in the department of physical therapy and the Center for Implementation Research. “So, we’re trying to work more on prevention.”
Vincenzo advises journalists to write about how accidental falls can be prevented. Remind your audiences that accidental falls are not an inevitable consequence of aging, and that while we do decline in many areas with age, there are things we can do to minimize the risk of falls, she says. And expand your coverage beyond the national Falls Prevention Awareness Week, which is always during the first week of fall — Sept. 23 to 27 this year.
Below, we explore falls among older people from different angles, including injury costs, prevention strategies and various disparities. We have paired each angle with data and research studies to inform your reporting.
Falls in older adults
In 2020, 14 million older adults in the U.S. reported falling during the previous year. In 2021, more than 38,700 older adults died due to unintentional falls, according to the CDC.
A fall could be immediately fatal for an older adult, but many times it’s the complications from a fall that lead to death.
The majority of hip fractures in older adults are caused by falls, Vincenzo says, and “it could be that people aren’t able to recover [from the injury], losing function, maybe getting pneumonia because they’re not moving around, or getting pressure injuries,” she says.
In addition, “sometimes people restrict their movement and activities after a fall, which they think is protective, but leads to further functional declines and increases in fall risk,” she adds.
Factors that can cause a fall include:
- Poor eyesight, reflexes and hearing. “If you cannot hear as well, anytime you’re doing something in your environment and there’s a noise, it will be really hard for you to focus on hearing what that noise is and what it means and also moving at the same time,” Vincenzo says.
- Loss of strength, balance, and mobility with age, which can lessen one’s ability to prevent a fall when slipping or tripping.
- Fear of falling, which usually indicates decreased balance.
- Conditions such as diabetes, heart disease, or problems with nerves or feet that can affect balance.
- Conditions like incontinence that cause rushed movement to the bathroom.
- Cognitive impairment or certain types of dementia.
- Unsafe footwear such as backless shoes or high heels.
- Medications or medication interactions that can cause dizziness or confusion.
- Safety hazards in the home or outdoors, such as poor lighting, steps and slippery surfaces.
Related Research
Nonfatal and Fatal Falls Among Adults Aged ≥65 Years — United States, 2020–2021
Ramakrishna Kakara, Gwen Bergen, Elizabeth Burns and Mark Stevens. Morbidity and Mortality Weekly Report, September 2023.Summary: Researchers analyzed data from the 2020 Behavioral Risk Factor Surveillance System — a landline and mobile phone survey conducted each year in all 50 U.S. states and the District of Columbia — and data from the 2021 National Vital Statistics System to identify patterns of injury and death due to falls in the U.S. by sex and state for adults 65 years and older. Among the findings:
- The percentage of women who reported falling was 28.9%, compared with 26.1% of men.
- Death rates from falls were higher among white and American Indian or Alaska Native older adults than among older adults from other racial and ethnic groups.
- In 2020, the percentage of older adults who reported falling during the past year ranged from 19.9% in Illinois to 38.0% in Alaska. The national estimate for 18 states was 27.6%.
- In 2021, the unintentional fall-related death rate among older adults ranged from 30.7 per 100,000 older adults in Alabama to 176.5 in Wisconsin. The national estimate for 26 states was 78.
“Although common, falls among older adults are preventable,” the authors write. “Health care providers can talk with patients about their fall risk and how falls can be prevented.”
Trends in Nonfatal Falls and Fall-Related Injuries Among Adults Aged ≥65 Years — United States, 2012-2018
Briana Moreland, Ramakrishna Kakara and Ankita Henry. Morbidity and Mortality Weekly Report, July 2020.Summary: Researchers compared data from the 2018 Behavioral Risk Factor Surveillance System. Among the findings:
- The percentage of older adults reporting a fall increased from 2012 to 2016, then slightly decreased from 2016 to 2018.
- Even with this decrease in 2018, older adults reported 35.6 million falls. Among those falls, 8.4 million resulted in an injury that limited regular activities for at least one day or resulted in a medical visit.
“Despite no significant changes in the rate of fall-related injuries from 2012 to 2018, the number of fall-related injuries and health care costs can be expected to increase as the proportion of older adults in the United States grows,” the authors write.
Understanding Modifiable and Unmodifiable Older Adult Fall Risk Factors to Create Effective Prevention Strategies
Gwen Bergen, et al. American Journal of Lifestyle Medicine, October 2019.Summary: Researchers used data from the 2016 U.S. Behavioral Risk Factor Surveillance System to better understand the association between falls and fall injuries in older adults and factors such as health, state and demographic characteristics. Among the findings:
- Depression had the strongest association with falls and fall injuries. About 40% of older adults who reported depression also reported at least one fall; 15% reported at least one fall injury.
- Falls and depression have several factors in common, including cognitive impairment, slow walking speed, poor balance, slow reaction time, weakness, low energy and low levels of activity.
- Other factors associated with an increased risk of falling include diabetes, vision problems and arthritis.
“The multiple characteristics associated with falls suggest that a comprehensive approach to reducing fall risk, which includes screening and assessing older adult patients to determine their unique, modifiable risk factors and then prescribing tailored care plans that include evidence-based interventions, is needed,” the authors write.
Health care use and cost
In addition to being the leading cause of injury, falls are the leading cause of hospitalization in older adults. Each year, about 3 million older adults visit the emergency department due to falls. More than 1 million get hospitalized.
In 2021, falls led to more than 38,000 deaths in adults 65 and older, according to the CDC.
The annual financial medical toll of falls among adults 65 years and older is expected to be more than $101 billion by 2030, according to the National Council on Aging, an organization advocating for older Americans.
Related research
Healthcare Spending for Non-Fatal Falls Among Older Adults, USA
Yara K. Haddad, et al. Injury Prevention, July 2024.Summary: In 2015, health care spending related to falls among older adults was roughly $50 billion. This study aims to update the estimate, using the 2017, 2019 and 2021 Medicare Current Beneficiary Survey, the most comprehensive and complete survey available on the Medicare population. Among the findings:
- In 2020, health care spending for non-fatal falls among older adults was $80 billion.
- Medicare paid $53.3 billion of the $80 billion, followed by $23.2 billion paid by private insurance or patients and $3.5 billion by Medicaid.
“The burden of falls on healthcare systems and healthcare spending will continue to rise if the risk of falls among the aging population is not properly addressed,” the authors write. “Many older adult falls can be prevented by addressing modifiable fall risk factors, including health and functional characteristics.”
Cost of Emergency Department and Inpatient Visits for Fall Injuries in Older Adults Lisa Reider, et al. Injury, February 2024.
Summary: The researchers analyzed data from the 2016-2018 National Inpatient Sample and National Emergency Department Sample, which are large, publicly available patient databases in the U.S. that include all insurance payers such as Medicare and private insurance. Among the findings:
- During 2016-2018, more than 920,000 older adults were admitted to the hospital and 2.3 million visited the emergency department due to falls. The combined annual cost was $19.2 billion.
- More than half of hospital admissions were due to bone fractures. About 14% of these admissions were due to multiple fractures and cost $2.5 billion.
“The $20 billion in annual acute treatment costs attributed to fall injury indicate an urgent need to implement evidence-based fall prevention interventions and underscores the importance of newly launched [emergency department]-based fall prevention efforts and investments in geriatric emergency departments,” the authors write.
Hip Fracture-Related Emergency Department Visits, Hospitalizations and Deaths by Mechanism of Injury Among Adults Aged 65 and Older, United States 2019
Briana L. Moreland, Jaswinder K. Legha, Karen E. Thomas and Elizabeth R. Burns. Journal of Aging and Health, June 2024.Summary: The researchers calculated hip fracture-related U.S. emergency department visits, hospitalizations and deaths among older adults, using data from the Healthcare Cost and Utilization Project and the National Vital Statistics System. Among the findings:
- In 2019, there were 318,797 emergency department visits, 290,130 hospitalizations and 7,731 deaths related to hip fractures among older adults.
- Nearly 88% of emergency department visits and hospitalizations and 83% of deaths related to hip fractures were caused by falls.
- These rates were highest among those living in rural areas and among adults 85 and older. More specifically, among adults 85 and older, the rate of hip fracture-related emergency department visits was nine times higher than among adults between 65 and 74 years old.
“Falls are common among older adults, but many are preventable,” the authors write. “Primary care providers can prevent falls among their older patients by screening for fall risk annually or after a fall, assessing modifiable risk factors such as strength and balance issues, and offering evidence-based interventions to reduce older adults’ risk of falls.”
Fall prevention
Several factors, including exercising, managing medication, checking vision and making homes safer can help prevent falls among older adults.
“Exercise is one of the best interventions we know of to prevent falls,” Vincenzo says. But “walking in and of itself will not help people to prevent falls and may even increase their risk of falling if they are at high risk of falls.”
The National Council on Aging also has a list of evidence-based fall prevention programs, including activities and exercises that are shown to be effective.
The National Institute on Aging has a room-by-room guide on preventing falls at home. Some examples include installing grab bars near toilets and on the inside and outside of the tub and shower, sitting down while preparing food to prevent fatigue, and keeping electrical cords near walls and away from walking paths.
There are also national and international initiatives to help prevent falls.
Stopping Elderly Accidents, Deaths and Injuries, or STEADI, is an initiative by the CDC’s Injury Center to help health care providers who treat older adults. It helps providers screen patients for fall risk, assess their fall risk factors and reduce their risk by using strategies that research has shown to be effective. STEADI’s guidelines are in line with the American and British Geriatric Societies’ Clinical Practice Guidelines for fall prevention.
“We’re making some iterations right now to STEADI that will come out in the next couple of years based on the World Falls Guidelines, as well as based on clinical providers’ feedback on how to make [STEADI] more feasible,” Vincenzo says.
The World Falls Guidelines is an international initiative to prevent falls in older adults. The guidelines are the result of the work of 14 international experts who came together in 2019 to consider whether new guidelines on fall prevention were needed. The task force then brought together 96 experts from 39 countries across five continents to create the guidelines.
The CDC’s STEADI initiative has a screening questionnaire for consumers to check their risk of falls, as does the National Council on Aging.
On the policy side, U.S. Rep. Carol Miller, R-W.V., and Melanie Stansbury, D-N.M., introduced the Stopping Addiction and Falls for the Elderly (SAFE) Act in March 2024. The bill would allow occupational and physical therapists to assess fall risks in older adults as part of the Medicare Annual Wellness Benefit. The bill was sent to the House Subcommittee on Health in the same month.
Meanwhile, older adults’ attitudes toward falls and fall prevention are also pivotal. For many, coming to terms with being at risk of falls and making changes such as using a cane, installing railings at home or changing medications isn’t easy for all older adults, studies show.
“Fall is a four-letter F-word in a way to older adults,” says Vincenzo, who started her career as a physical therapist. “It makes them feel ‘old.’ So, it’s a challenge on multiple fronts: U.S. health care infrastructure, clinical and community resources and facilitating health behavior change.”
Related research
Environmental Interventions for Preventing Falls in Older People Living in the Community
Lindy Clemson, et al. Cochrane Database of Systematic Reviews, March 2023.Summary: This review includes 22 studies from 10 countries involving a total of 8,463 older adults who live in the community, which includes their own home, a retirement facility or an assisted living facility, but not a hospital or nursing home. Among the findings:
- Removing fall hazards at home reduced the number of falls by 38% among older adults at a high risk of having a fall, including those who have had a fall in the past year, have been hospitalized or need support with daily activities. Examples of fall hazards at home include a stairway without railings, a slippery pathway or poor lighting.
- It’s unclear whether checking prescriptions for eyeglasses, wearing special footwear or installing bed alarm systems reduces the rate of falls.
- It’s also not clear whether educating older adults about fall risks reduces their fall risk.
The Influence of Older Adults’ Beliefs and Attitudes on Adopting Fall Prevention Behaviors
Judy A. Stevens, David A. Sleet and Laurence Z. Rubenstein. American Journal of Lifestyle Medicine. January 2017.Summary: Persuading older adults to adopt interventions that reduce their fall risk is challenging. Their attitudes and beliefs about falls play a large role in how well they accept and adopt fall prevention strategies, the authors write. Among the common attitudes and beliefs:
- Many older adults believe that falls “just happen,” are a normal result of aging or are simply due to bad luck.
- Many don’t acknowledge or recognize their fall risk.
- For many, falls are considered to be relevant only for frail or very old people.
- Many believe that their home environment or daily activities can be a risk for fall, but do not consider biological factors such as dizziness or muscle weakness.
- For many, fall prevention simply consists of “being careful” or holding on to things when moving about the house.
“To reduce falls, health care practitioners have to help patients understand and acknowledge their fall risk while emphasizing the positive benefits of fall prevention,” the authors write. “They should offer patients individualized fall prevention interventions as well as provide ongoing support to help patients adopt and maintain fall prevention strategies and behaviors to reduce their fall risk. Implementing prevention programs such as CDC’s STEADI can help providers discuss the importance of falls and fall prevention with their older patients.”
Reframing Fall Prevention and Risk Management as a Chronic Condition Through the Lens of the Expanded Chronic Care Model: Will Integrating Clinical Care and Public Health Improve Outcomes?
Jennifer L. Vincenzo, Gwen Bergen, Colleen M. Casey and Elizabeth Eckstrom. The Gerontologist, June 2024.Summary: The authors recommend approaching fall prevention from the lens of chronic disease management programs because falls and fall risk are chronic issues for many older adults.
“Policymakers, health systems, and community partners can consider aligning fall risk management with the [Expanded Chronic Care Model], as has been done for diabetes,” the authors write. “This can help translate high-quality research on the effectiveness of fall prevention interventions into daily practice for older adults to alter the trajectory of older adult falls and fall-related injuries.”
Disparities
Older adults face several barriers to reducing their fall risk. Accessing health care services and paying for services such as physical therapy is not feasible for everyone. Some may lack transportation resources to go to and from medical appointments. Social isolation can increase the risk of death from falls. In addition, physicians may not have the time to fit in a fall risk screening while treating older patients for other health concerns.
Moreover, implementing fall risk screening, assessment and intervention in the current U.S. health care structure remains a challenge, Vincenzo says.
Related research
Mortality Due to Falls by County, Age Group, Race, and Ethnicity in the USA, 2000-19: A Systematic Analysis of Health Disparities
Parkes Kendrick, et al. The Lancet Public Health, August 2024.Summary: Researchers analyzed death registration data from the U.S. National Vital Statistics System and population data from the U.S. National Center for Health Statistics to estimate annual fall-related mortality. The data spanned from 2000 to 2019 and includes all age groups. Among the findings:
- The disparities between racial and ethnic populations varied widely by age group. Deaths from falls among younger adults were highest for the American Indian/Alaska Native population, while among older adults it was highest for the white population.
- For older adults, deaths from falls were particularly high in the white population within clusters of counties across states including Florida, Minnesota and Wisconsin.
- One factor that could contribute to higher death rates among white older adults is social isolation, the authors write. “Studies suggest that older Black and Latino adults are more likely to have close social support compared with older white adults, while AIAN and Asian individuals might be more likely to live in multigenerational households,” they write.
“Among older adults, current prevention techniques might need to be restructured to reduce frailty by implementing early prevention and emphasizing particularly successful interventions. Improving social isolation and evaluating the effectiveness of prevention programs among minoritized populations are also key,” the authors write.
Demographic Comparisons of Self-Reported Fall Risk Factors Among Older Adults Attending Outpatient Rehabilitation
Mariana Wingood, et al. Clinical Interventions in Aging, February 2024.Summary: Researchers analyzed the electronic health record data of 108,751 older adults attending outpatient rehabilitation within a large U.S. health care system across seven states, between 2018 and 2022. Among the findings:
- More than 44% of the older adults were at risk of falls; nearly 35% had a history of falls.
- The most common risk factors for falls were diminished strength, gait and balance.
- Compared to white older adults, Native American/Alaska Natives had the highest prevalence of fall history (43.8%) and Hispanics had the highest prevalence of falls with injury (56.1%).
“Findings indicate that rehabilitation providers should perform screenings for these impairments, including incontinence and medication among females, loss of feeling in the feet among males, and all Stay Independent Questionnaire-related fall risk factors among Native American/Alaska Natives, Hispanics, and Blacks,” the authors write.
Resources and articles
- National Institute on Aging
- National Council on Aging
- Gerontological Society of America
- Home Health Agencies Failed To Report Over Half of Falls With Major Injury and Hospitalization Among Their Medicare Patients, a 2023 report from the U.S Department of Health and Human Services’ Office of Inspector General.
- 6 tips for improving new coverage of older people, a tip sheet from The Journalist’s Resource.
- Crosswalk and pedestrian safety: What you need to know from recent research, from The Journalist’s Resource.
- Aging-in-place technology challenges and trends, a resource from the Association of Health Care Journalists.
- Successful aging at home: what reporters should know, a resource from the Association of Health Care Journalists.
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
He Thinks His Wife Died in an Understaffed Hospital. Now He’s Trying to Change the Industry.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For the past year, police Detective Tim Lillard has spent most of his waking hours unofficially investigating his wife’s death.
The question has never been exactly how Ann Picha-Lillard died on Nov. 19, 2022: She succumbed to respiratory failure after an infection put too much strain on her weakened lungs. She was 65.
For Tim Lillard, the question has been why.
Lillard had been in the hospital with his wife every day for a month. Nurses in the intensive care unit had told him they were short-staffed, and were constantly rushing from one patient to the next.
Lillard tried to pitch in where he could: brushing Ann’s shoulder-length blonde hair or flagging down help when her tracheostomy tube gurgled — a sign of possible respiratory distress.
So the day he walked into the ICU and saw staff members huddled in Ann’s room, he knew it was serious. He called the couple’s adult children: “It’s Mom,” he told them. “Come now.”
All he could do then was sit on Ann’s bed and hold her hand, watching as staff members performed chest compressions, desperately trying to save her life.
A minute ticked by. Then another. Lillard’s not sure how long the CPR continued — long enough for the couple’s son to arrive and take a seat on the other side of Ann’s bed, holding her other hand.
Finally, the intensive care doctor called it and the team stopped CPR. Time of death: 12:37 p.m.
Lillard didn’t know what to do in a world without Ann. They had been married almost 25 years. “We were best friends,” he said.
Just days before her death, nurses had told Lillard that Ann could be discharged to a rehabilitation center as soon as the end of the week. Then, suddenly, she was gone. Lillard didn’t understand what had happened.
Lillard said he now believes that overwhelmed, understaffed nurses hadn’t been able to respond in time as Ann’s condition deteriorated. And he has made it his mission to fight for change, joining some nursing unions in a push for mandatory ratios that would limit the number of patients in a nurse’s care. “I without a doubt believe 100% Ann would still be here today if they had staffing levels, mandatory staffing levels, especially in ICU,” Lillard said.
Last year, Oregon became the second state after California to pass hospital-wide nurse ratios that limit the number of patients in a nurse’s care. Michigan, Maine, and Pennsylvania are now weighing similar legislation.
But supporters of mandatory ratios are going up against a powerful hospital industry spending millions of dollars to kill those efforts. And hospitals and health systems say any staffing ratio regulations, however well-intentioned, would only put patients in greater danger.
Putting Patients at Risk
By next year, the United States could have as many as 450,000 fewer nurses than it needs, according to one estimate. The hospital industry blames covid-19 burnout, an aging workforce, a large patient population, and an insufficient pipeline of new nurses entering the field.
But nursing unions say that’s not the full story. There are now 4.7 million registered nurses in the country, more than ever before.
The problem, the unions say, is a hospital industry that’s been intentionally understaffing their units for years in order to cut costs and bolster profits. The unions say there isn’t a shortage of nurses but a shortage of nurses willing to work in those conditions.
The nurse staffing crisis is now affecting patient care. The number of Michigan nurses who say they know of a patient who has died because of understaffing has nearly doubled in recent years, according to a Michigan Nurses Association survey last year.
Just months before Ann Picha-Lillard’s death, nurses and doctors at the health system where she died had asked the Michigan attorney general to investigate staffing cuts they believed were leading to dangerous conditions, including patient deaths, according to The Detroit News.
But Lillard didn’t know any of that when he drove his wife to the hospital in October 2022. She had been feeling short of breath for a few weeks after she and Lillard had mild covid infections. They were both vaccinated, but Ann was immunocompromised. She suffered from rheumatoid arthritis, a condition that had also caused scarring in her lungs.
To be safe, doctors at DMC Huron Valley-Sinai Hospital wanted to keep Ann for observation. After a few days in the facility, she developed pneumonia. Doctors told the couple that Ann needed to be intubated. Ann was terrified but Lillard begged her to listen to the doctors. Tearfully, she agreed.
With Ann on a ventilator in the ICU, it seemed clear to Lillard that nurses were understaffed and overwhelmed. One nurse told him they had been especially short-staffed lately, Lillard said.
“The alarms would go off for the medications, they’d come into the room, shut off the alarm when they get low, run to the medication room, come back, set them down, go to the next room, shut off alarms,” Lillard recalled. “And that was going on all the time.”
Lillard felt bad for the nurses, he said. “But obviously, also for my wife. That’s why I tried doing as much as I could when I was there. I would comb her hair, clean her, just keep an eye on things. But I had no idea what was really going on.”
Finally, Ann’s health seemed to be stabilizing. A nurse told Lillard they’d be able to discharge Ann, possibly by the end of that week.
By Nov. 17, Ann was no longer sedated and she cried when she saw Lillard and her daughter. Still unable to speak, she tried to mouth words to her husband “but we couldn’t understand what she was saying,” Lillard said.
The next day, Lillard went home feeling hopeful, counting down the days until Ann could leave the hospital.
Less than 24 hours later, Ann died.
Lillard couldn’t wrap his head around how things went downhill so fast. Ann’s underlying lung condition, the infection, and her weakened state could have proved fatal in the best of circumstances. But Lillard wanted to understand how Ann had gone from nearly discharged to dying, seemingly overnight.
He turned his dining room table into a makeshift office and started with what he knew. The day Ann died, he remembered her medical team telling him that her heart rate had spiked and she had developed another infection the night before. Lillard said he interviewed two DMC Huron Valley-Sinai nurse administrators, and had his own doctor look through Ann’s charts and test results from the hospital. “Everybody kept telling me: sepsis, sepsis, sepsis,” he said.
Sepsis is when an infection triggers an extreme reaction in the body that can cause rapid organ failure. It’s one of the leading causes of death in U.S. hospitals. Some experts say up to 80% of sepsis deaths are preventable, while others say the percentage is far lower.
Lives can be saved when sepsis is caught and treated fast, which requires careful attention to small changes in vital signs. One study found that for every additional patient a nurse had to care for, the mortality rate from sepsis increased by 12%.
Lillard became convinced that had there been more nurses working in the ICU, someone could have caught what was happening to Ann.
“They just didn’t have the time,” he said.
DMC Huron Valley-Sinai’s director of communications and media relations, Brian Taylor, declined a request for comment about the 2022 staffing complaint to the Michigan attorney general.
Following the Money
When Lillard asked the hospital for copies of Ann’s medical records, DMC Huron Valley-Sinai told him he’d have to request them from its parent company in Texas.
Like so many hospitals in recent years, the Lillards’ local health system had been absorbed by a series of other corporations. In 2011, the Detroit Medical Center health system was bought for $1.5 billion by Vanguard Health Systems, which was backed by the private equity company Blackstone Group.
Two years after that, in 2013, Vanguard itself was acquired by Tenet Healthcare, a for-profit company based in Dallas that, according to its website, operates 480 ambulatory surgery centers and surgical hospitals, 52 hospitals, and approximately 160 additional outpatient centers.
As health care executives face increasing pressure from investors, nursing unions say hospitals have been intentionally understaffing nurses to reduce labor costs and increase revenue. Also, insurance reimbursements incentivize keeping nurse staffing levels low. “Hospitals are not directly reimbursed for nursing services in the same way that a physician bills for their services,” said Karen Lasater, an associate professor of nursing in the Center for Health Outcomes and Policy Research at the University of Pennsylvania. “And because hospitals don’t perceive nursing as a service line, but rather a cost center, they think about nursing as: How can we reduce this to the lowest denominator possible?” she said.
Lasater is a proponent of mandatory nurse ratios. “The nursing shortage is not a pipeline problem, but a leaky bucket problem,” she said. “And the solutions to this crisis need to address the root cause of the issue, which is why nurses are saying they’re leaving employment. And it’s rooted in unsafe staffing. It’s not safe for the patients, but it’s also not safe for nurses.”
A Battle Between Hospitals and Unions
In November, almost one year after Ann’s death, Lillard told a room of lawmakers at the Michigan State Capitol that he believes the Safe Patient Care Act could save lives. The health policy committee in the Michigan House was holding a hearing on the proposed act, which would limit the amount of mandatory overtime a nurse can be forced to work, and require hospitals to make their staffing levels available to the public.
Most significantly, the bills would require hospitals to have mandatory, minimum nurse-to-patient ratios. For example: one nurse for every patient in the ICU; one for every three patients in the emergency room; a nurse for triage; and one nurse for every four postpartum birthing patients and well-baby care.
Efforts to pass mandatory ratio laws failed in Washington and Minnesota last year after facing opposition from the hospital industry. In Minnesota, the Minnesota Nurses Association accused the Mayo Clinic of using “blackmail tactics”: Mayo had told lawmakers it would pull billions of dollars in investment from the state if mandatory ratio legislation passed. Soon afterward, lawmakers removed nurse ratios from the legislation.
While Lillard waited for his turn to speak to Michigan lawmakers about the Safe Patient Care Act in November, members of the Michigan Nurses Association, which says it represents some 13,000 nurses, told lawmakers that its units were dangerously understaffed. They said critical care nurses were sometimes caring for up to 11 patients at a time.
“Last year I coded someone in an ICU for 10 minutes, all alone, because there was no one to help me,” said the nurses association president and registered nurse Jamie Brown, reading from another nurse’s letter.
“I have been left as the only specially trained nurse to take care of eight babies on the unit: eight fragile newborns,” said Carolyn Clemens, a registered nurse from the Grand Blanc area of Michigan.
Nikia Parker said she has left full-time emergency room nursing, a job she believes is her calling. After her friend died in the hospital where she worked, she was left wondering whether understaffing may have contributed to his death.
“If the Safe Patient Care Act passed, and we have ratios, I’m one of those nurses who would return to the bedside full time,” Parker told lawmakers. “And so many of my co-workers who have left would join me.”
But not all nurses agree that mandatory ratios are a good idea.
While the American Nurses Association supports enforceable ratios as an “essential approach,” that organization’s Michigan chapter does not, saying there may not be enough nurses in the state to satisfy the requirements of the Safe Patient Care Act.
For some lawmakers, the risk of collateral damage seems too high. State Rep. Graham Filler said he worries that mandating ratios could backfire.
“We’re going to severely hamper health care in the state of Michigan. I’m talking closed wards because you can’t meet the ratio in a bill. The inability for a hospital to treat an emergent patient. So it feels kind of to me like a gamble we’re taking,” said Filler, a Republican.
Michigan hospitals are already struggling to fill some 8,400 open positions, according to the Michigan Health & Hospital Association. That association says that complying with the Safe Patient Care Act would require hiring 13,000 nurses.
Every major health system in the state signed a letter opposing mandatory ratios, saying it would force them to close as many as 5,100 beds.
Lillard watched the debate play out in the hearing. “That’s a scare tactic, in my opinion, where the hospitals say we’re going to have to start closing stuff down,” he said.
He doesn’t think legislation on mandatory ratios — which are still awaiting a vote in the Michigan House’s health policy committee — are a “magic bullet” for such a complex, national problem. But he believes they could help.
“The only way these hospitals and the administrations are gonna make any changes, and even start moving towards making it better, is if they’re forced to,” Lillard said.
Seated in the center of the hearing room in Lansing, next to a framed photo of Ann, Lillard’s hands shook as he recounted those final minutes in the ICU.
“Please take action so that no other person or other family endures this loss,” he said. “You can make a difference in saving lives.”
Grief is one thing, Lillard said, but it’s another thing to be haunted by doubts, to worry that your loved one’s care was compromised before they ever walked through the hospital doors. What he wants most, he said, is to prevent any other family from having to wonder, “What if?”
This article is from a partnership that includes Michigan Public, NPR, and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
7 Essential Devices For Hand Arthritis: Regain Control of Your Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Diana Girnita is a double board-certified physician in rheumatology and internal medicine. With a PhD in immunology (on top of her MD), and training at Harvard and top universities, she founded Rheumatologist OnCall, offering integrative medicine to broaden rheumatology access. Here’s what she has to say about things that make life easier:
Get your hands on these…
The seven devices that Dr. Girnita recommends are:
- Hand grip strengthener: helps build grip strength with a spring-loaded mechanism. Regular use can improve strength and reduce pain.
- Finger exerciser: different device; similar principle: it strengthens hand and finger muscles using resistance, enhancing hand function.
- Moisturizing paraffin bath: a heated paraffin wax bath that soothes hands, providing heat therapy and moisturizing the skin.
- Weighted silverware: weighted utensils (knives, forks, spoons) make gripping easier and provide stability for eating.
- Foam tubing grips: foam covers to make kitchen tools, toothbrushes, and hairbrushes easier to grip.
- Electric can-opener: reduces strain in opening cans, making meal preparation more accessible.
- Compression gloves: provide gentle compression to reduce swelling and pain, improving hand flexibility and circulation.
- Door knob cover grips: make it easier to turn doorknobs by providing a larger surface to grip.
- Wider-grip pens: ergonomically designed pens with a larger diameter and softer grip reduce hand strain while writing.
This writer, who does not have arthritis but also does not have anything like the grip strength she used to, also recommends a jar opener like this one.
As a bonus, if you spend a lot of time writing at a computer, an ergonomic split keyboard like this one goes a long way to avoiding carpal tunnel syndrome, and logically must be better for arthritis than a regular keyboard; another excellent thing to have (that again this writer uses and swears by) is an ergonomic vertical mouse like this one (aligns the wrist bones correctly; the “normal” horizontal version is woeful for the carpal bones). These things are both also excellent to help avoid worsening peripheral neuropathy (something that troubles this writer’s wrists if she’s not careful, due to old injuries there).
For more on the seven things otherwise listed above, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Avoiding/Managing Rheumatoid Arthritis
- Avoiding/Managing Osteoarthritis
- Managing Chronic Pain (Realistically!)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Brain-Gut Highway: A Two-Way Street
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Brain-Gut Two-Way Highway
This is Dr. Emeran Mayer. He has the rather niche dual specialty of being a gastroenterologist and a neurologist. He has published over 353 peer reviewed scientific articles, and he’s a professor in the Departments of Medicine, Physiology, and Psychiatry at UCLA. Much of his work has been pioneering medical research into gut-brain interactions.
We know the brain and gut are connected. What else does he want us to know?
First, that it is a two-way interaction. It’s about 90% “gut tells the brain things”, but it’s also 10% “brain tells the gut things”, and that 10% can make more like a 20% difference, if for example we look at the swing between “brain using that 10% communication to tell gut to do things worse” or “brain using that 10% communication to tell gut to do things better”, vs the midpoint null hypothesis of “what the gut would be doing with no direction from the brain”.
For example, if we are experiencing unmanaged chronic stress, that is going to tell our gut to do things that had an evolutionary advantage 20,000–200,000 years ago. Those things will not help us now. We do not need cortisol highs and adrenal dumping because we ate a piece of bread while stressed.
Read more (by Dr. Mayer): The Stress That Evolution Has Not Prepared Us For
With this in mind, if we want to look after our gut, then we can start before we even put anything in our mouths. Dr. Mayer recommends managing stress, anxiety, and depression from the head downwards as well as from the gut upwards.
Here’s what we at 10almonds have written previously on how to manage those things:
- No-Frills, Evidence-Based Mindfulness
- How To Set Anxiety Aside
- The Mental Health First-Aid You’ll Hopefully Never Need
Do eat for gut health! Yes, even if…
Unsurprisingly, Dr. Mayer advocates for a gut-friendly, anti-inflammatory diet. We’ve written about these things before:
…but there’s just one problem:
For some people, such as with IBS, Crohn’s, and colitis, the Mediterranean diet that we (10almonds and Dr. Mayer) generally advocate for, is inaccessible. If you (if you have those conditions) eat as we describe, a combination of the fiber in many vegetables and the FODMAPs* in many fruits, will give you a very bad time indeed.
*Fermentable Oligo-, Di-, Monosaccharides And Polyols
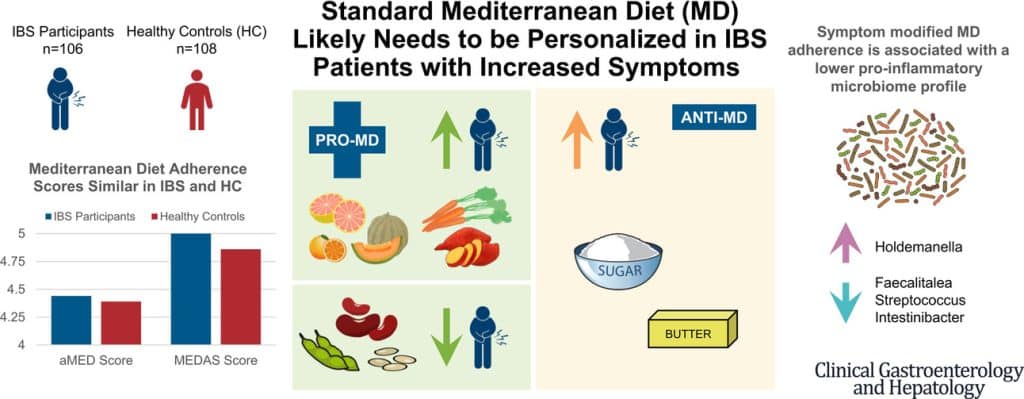
Dr. Mayer has the answer to this riddle, and he’s not just guessing; he and his team did science to it. In a study with hundreds of participants, he measured what happened with adherence (or not) to the Mediterranean diet (or modified Mediterranean diet) (or not), in participants with IBS (or not).
The results and conclusions from that study included:
❝Among IBS participants, a higher consumption of fruits, vegetables, sugar, and butter was associated with a greater severity of IBS symptoms. Multivariate analysis identified several Mediterranean Diet foods to be associated with increased IBS symptoms.
A higher adherence to symptom-modified Mediterranean Diet was associated with a lower abundance of potentially harmful Faecalitalea, Streptococcus, and Intestinibacter, and higher abundance of potentially beneficial Holdemanella from the Firmicutes phylum.
A standard Mediterranean Diet was not associated with IBS symptom severity, although certain Mediterranean Diet foods were associated with increased IBS symptoms. Our study suggests that standard Mediterranean Diet may not be suitable for all patients with IBS and likely needs to be personalized in those with increased symptoms.❞
In graphical form:
And if you’d like to read more about this (along with more details on which specific foods to include or exclude to get these results), you can do so…
- The study itself (full article): The Association Between a Mediterranean Diet and Symptoms of Irritable Bowel Syndrome
- Dr. Mayer’s blog (lay explanation): The Benefits of a Modified Mediterranean Diet for Irritable Bowel Syndrome
Want to know more?
Dr. Mayer offers many resources, including a blog, books, recipes, podcasts, and even a YouTube channel:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: