Chickpeas vs Soybeans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chickpeas to soybeans, we picked the soybeans.
Why?
Both are great! But:
In terms of macros, chickpeas have more than 3x the carbs and only very slightly more fiber, while soybeans have more than 2x the protein. Given the ratio of carbs to fiber in each, soybeans also have the lower glycemic index, so all in all, we’re calling this a win for soybeans.
In the category of vitamins, chickpeas have more of vitamins A, B3, B5, and B9, while soybeans have more of vitamins B1, B2, B6, C, K, and choline—another win for soybeans.
When it comes to minerals, chickpeas have more manganese and zinc, while soybeans have more calcium, copper, iron, magnesium, phosphorus, potassium, and selenium—meaning soybeans win yet again.
Two extra things to know:
- Chickpeas are naturally high in FODMAPs, which can be problematic for a minority of people—however, canned chickpeas are not.
- Soybeans are famously high in phytoestrogens, however, the human body cannot actually use these as estrogen (we are not plants and our physiology is different). This means that on the one hand they won’t help against menopause (aside from the ways in which any nutrient-dense food would help), but on the other, they aren’t a cancer risk, and no, they won’t feminize men/boys in the slightest. You/they would be more at risk from beef and dairy, as the cows have usually been given extra estrogen, and those are animal hormones, not plant hormones.
All in all, chickpeas are a wonderful food, but soybeans beat them by most nutritional metrics.
Want to learn more?
You might like to read:
Why You Can’t Skimp On Amino Acids ← soybeans also have a great amino acid profile!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Antibiotics? Think Thrice
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Antibiotics: Useful Even Less Often Than Previously Believed (And Still Just As Dangerous)
You probably already know that antibiotics shouldn’t be taken unless absolutely necessary. Not only does taking antibiotics frivolously increase antibiotic resistance (which is bad, and kills people), but also…
It’s entirely possible for the antibiotics to not only not help, but instead wipe out your gut’s “good bacteria” that were keeping other things in check.
Those “other things” can include fungi like Candida albicans.
Candida, which we all have in us to some degree, feeds on sugar (including the sugar formed from breaking down alcohol, by the way) and refined carbs. Then it grows, and puts its roots through your intestinal walls, linking with your neural system. Then it makes you crave the very things that will feed it and allow it to put bigger holes in your intestinal walls.
Don’t believe us? Read: Candida albicans-Induced Epithelial Damage Mediates Translocation through Intestinal Barriers
(That’s scientist-speak for “Candida puts holes in your intestines, and stuff can then go through those holes”)
And as for how that comes about, it’s like we said:
See also: Candida albicans as a commensal and opportunistic pathogen in the intestine
That’s not all…
And that’s just C. albicans, never mind things like C. diff. that can just outright kill you easily.
We don’t have room to go into everything here, but you might like to check out:
Four Ways Antibiotics Can Kill You
It gets worse (now comes the new news)
So, what are antibiotics good for? Surely, for clearing up chesty coughs, lower respiratory tract infections, right? It’s certainly one of the two things that antibiotics are most well-known for being good at and often necessary for (the other being preventing/treating sepsis, for example in serious and messy wounds).
But wait…
A large, nationwide (US) observational study of people who sought treatment in primary or urgent care settings for lower respiratory tract infections found…
(drumroll please)
…the use of antibiotics provided no measurable impact on the severity or duration of coughs even if a bacterial infection was present.
Read for yourself:
And in the words of the lead author of that study,
❝Lower respiratory tract infections tend to have the potential to be more dangerous, since about 3% to 5% of these patients have pneumonia. But not everyone has easy access at an initial visit to an X-ray, which may be the reason clinicians still give antibiotics without any other evidence of a bacterial infection.❞
So, what’s to be done about this? On a large scale, Dr. Merenstein recommends:
❝Serious cough symptoms and how to treat them properly needs to be studied more, perhaps in a randomized clinical trial as this study was observational and there haven’t been any randomized trials looking at this issue since about 2012.❞
This does remind us that, while not a RCT, there is a good ongoing observational study that everyone with a smartphone can participate in:
Dr. Peter Small’s medical AI: “The Cough Doctor”
In the meantime, he advises that when COVID and SARS have been ruled out, then “basic symptom-relieving medications plus time brings a resolution to most people’s infections”.
You can read a lot more detail here:
Antibiotics aren’t effective for most lower tract respiratory infections
In summary…
Sometimes, antibiotics really are a necessary and life-saving medication. But most of the time they’re not, and given their great potential for harm, they may be best simultaneously viewed as the very dangerous threat they also are, and used only when those “heavy guns” are truly what’s required.
Take care!
Share This Post
-
Young Mind Young Body – by Sue Ziang
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a very “healthy mind in a healthy body” book, consistent with the author’s status as a holistic health coach. Sometimes that produces a bit of a catch-22 regarding where to start, but for Ziang, the clear answer is to start with the mind, and specifically, one’s perception of one’s own age.
She advocates for building a young mind in a young body, and yes, that’s mind-building much like body-building. This does not mean any kind of wilful self-delusion, but rather, choosing the things that we do get to choose along the way.
The bridge between mind and body, for Ziang, is meditation—which is reasonable, as it’s very much mind-stuff and also very much neurological and has a very real-world impact on the body’s broader health, even simply by such mechanisms as changing breathing, heart rate, neurotransmitter levels, endocrine functions, and the like.
When it comes to the more physical aspects of health, her dietary advice is completely in line with what we write here at 10almonds. Hydrate well, eat more plants, especially beans and greens and whole grains, get good fats in, enjoy spices, practice mindful eating, skip the refined carbohydrates, be mindful of bio-individuality (e.g. one’s own personal dietary quirks that stem from physiology; some of us react differently to this kind of food or that for genetic reasons, and that’s not something to be overlooked).
In the category of exercise, she’s simply about moving more, which while not comprehensive, is not bad advice either.
Bottom line: if you’re looking for an “in” to holistic health and wondering where to start, this book is a fine and very readable option.
Click here to check out “Young Mind Young Body”, and transform yours!
Share This Post
-
Olive oil is healthy. Turns out olive leaf extract may be good for us too
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Olive oil is synonymous with the Mediterranean diet, and the health benefits of both are well documented.
Olive oil reduces the risk of heart disease, cancer, diabetes and premature death. Olives also contain numerous healthy nutrients.
Now evidence is mounting about the health benefits of olive leaves, including from studies in a recent review.
Here’s what’s in olive leaves and who might benefit from taking olive leaf extract.
mtphoto19/Shutterstock What’s in olive leaves?
Olive leaves have traditionally been brewed as a tea in the Mediterranean and drunk to treat fever and malaria.
The leaves contain high levels of a type of antioxidant called oleuropein. Olives and olive oil contain this too, but at lower levels.
Generally, the greener the leaf (the less yellowish) the more oleuropein it contains. Leaves picked in spring also have higher levels compared to ones picked in autumn, indicating levels of oleuropein reduce as the leaves get older.
Olive leaves also contain other antioxidants such as hydroxytyrosol, luteolin, apigenin and verbascoside.
Antioxidants work by reducing the oxidative stress in the body. Oxidative stress causes damage to our DNA, cell membranes and tissues, which can lead to chronic diseases such as cancer and heart disease.
Are olive leaves healthy?
One review and analysis combined data from 12 experimental studies with 819 participants in total. Overall, olive leaf extract improved risk factors for heart disease. This included healthier blood lipids (fats) and lowering blood pressure.
The effect was greater for people who already had high blood pressure.
Most studies in this review gave olive leaf extract as a capsule, with daily doses of 500 milligrams to 5 grams for six to 48 weeks.
Another review and analysis published late last year looked at data from 12 experimental studies, with a total of 703 people. Some of these studies involved people with high blood lipids, people with high blood pressure, people who were overweight or obese, and some involved healthy people.
Daily doses were 250-1,000mg taken as tablets or baked into bread.
Individual studies in the review showed significant benefits in improving blood glucose (sugar) control, blood lipid levels and reducing blood pressure. But when all the data was combined, there were no significant health effects. We’ll explain why this may be the case shortly.
Olive leaves can be brewed into tea. Picture Partners/Shutterstock Another review looked at people who took oleuropein and hydroxytyrosol (the antioxidants in olive leaves). This found significant improvement in body weight, blood lipid profiles, glucose metabolism and improvements in bones, joints and cognitive function.
The individual studies included tested either the two antioxidants or olive leaf incorporated into foods such as bread and cooking oils (but not olive oil). The doses were 6-500mg per day of olive leaf extract.
So what can we make of these studies overall? They show olive leaf extract may help reduce blood pressure, improve blood lipids and help our bodies handle glucose.
But these studies show inconsistent results. This is likely due to differences in the way people took olive leaf extract, how much they took and how long for. This type of inconsistency normally tells us we need some more research to clarify the health effects of olive leaves.
Can you eat olive leaves?
Olive leaves can be brewed into a tea, or the leaves added to salads. Others report grinding olive leaves into smoothies.
However the leaves are bitter, because of the antioxidants, which can make them hard to eat, or the tea unpalatable.
Olive leaf extract has also been added to bread and other baked goods. Researchers find this improves the level of antioxidants in these products and people say the foods tasted better.
Olive leaves can taste bitter, which can put people off. But you can bake the extract into bread. Repina Valeriya/Shutterstock Is olive leaf extract toxic?
No, there seem to be no reported toxic effects of eating or drinking olive leaf extract.
It appears safe up to 1g a day, according to studies that have used olive leaf extract. However, there are no official guidelines about how much is safe to consume.
There have been reports of potential toxicity if taken over 85mg/kg of body weight per day. For an 80kg adult, this would mean 6.8g a day, well above the dose used in the studies mentioned in this article.
Pregnant and breastfeeding women are recommended not to consume it as we don’t know if it’s safe for them.
What should I do?
If you have high blood pressure, diabetes or raised blood lipids you may see some benefit from taking olive leaf extract. But it is important you discuss this with your doctor first and not change any medications or start taking olive leaf extract until you have spoken to them.
But there are plenty of antioxidants in all plant foods, and you should try to eat a wide variety of different coloured plant foods. This will allow you to get a range of nutrients and antioxidants.
Olive leaf and its extract is not going to be a panacea for your health if you’re not eating a healthy diet and following other health advice.
Evangeline Mantzioris, Program Director of Nutrition and Food Sciences, Accredited Practising Dietitian, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
All In Your Head (Which Is Where It’s Supposed To Be)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Today’s news is all about things above the neck, and mostly in the brain. From beating depression to beating cognitive decline, from mindfulness against pain to dentistry nightmares to avoid:
Transcranial ultrasound stimulation
Transcranial magnetic stimulation is one of those treatments that sounds like it’s out of a 1950s sci-fi novel, and yet, it actually works (it’s very well-evidenced against treatment-resistant depression, amongst other things). However, a weakness of it is that it’s difficult to target precisely, making modulation of most neurological disorders impossible. Using ultrasound instead of a magnetic field allows for much more finesse, with very promising initial results across a range of neurological disorders
Read in full: Transcranial ultrasound stimulation: a new frontier in non-invasive brain therapy
Related: Antidepressants: Personalization Is Key!
This may cause more pain and damage, but at least it’s more expensive too…
While socialized healthcare systems sometimes run into the problem of not wanting to spend money where it actually is needed, private healthcare systems have the opposite problem: there’s a profit incentive to upsell to more expensive treatments. Here’s how that’s played out in dentistry:
Read in full: Dentists are pulling healthy and treatable teeth to profit from implants, experts warn
Related: Tooth Remineralization: How To Heal Your Teeth Naturally
Mindfulness vs placebo, for pain
It can be difficult with some “alternative therapies” to test against placebo, for example “and control group B will merely believe that they are being pierced with needles”, etc. However, in this case, mindfulness meditation was tested as an analgesic vs sham meditation (just deep breathing) and also vs placebo analgesic cream, vs distraction (listening to an audiobook). Mindfulness meditation beat all of the other things:
Read in full: Mindfulness meditation outperforms placebo in reducing pain
Related: No-Frills, Evidence-Based Mindfulness
Getting personal with AI doctors
One of the common reasons that people reject AI doctors is the “lack of a human touch”. However, human and AI doctors may be meeting in the middle nowadays, as humans are pressed to see more patients in less time, and AI is trained to be more personal—not just a friendlier affect, but also, such things as remembering the patient’s previous encounters (again, something with which overworked human doctors sometimes struggle). This makes a big difference to patient satisfaction:
Read in full: Personalization key to patient satisfaction with AI doctors
Related: AI: The Doctor That Never Tires?
Combination brain therapy against cognitive decline
This study found that out of various combinations trialled, the best intervention against cognitive decline was a combination of 1) cognitive remediation (therapeutic interventions designed to improve cognitive functioning, like puzzles and logic problems), and 2) transcranial direct current stimulation (tDCS), a form of non-invasive direct brain stimulation, similar to the magnetic or ultrasound methods we mentioned earlier today. Here’s how it worked:
Read in full: Study reveals effective combination therapy to slow cognitive decline in older adults
Related: How To Reduce Your Alzheimer’s Risk
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
NADᐩ Against Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nicotinamide adenine dinucleotide, or “NAD” to its friends, is a coenzyme produced in the human body (amongst other places), and it is critical for cellular energy metabolism, but there’s more to it than that.
Today we’ll be looking mostly at NAD+, of which the + indicates the positive formal charge of one of its nitrogen atoms. We won’t get too much into the chemistry of this, but we will mention that it’s a cofactor with NADH—the former accepting electrons and the latter donating electrons.
Both NAD+ and NADH are critical to good health, but we’re going to focus on NAD+ for the simple reason that it gets depleted with aging.
Note: it gets depleted with aging.
Chronological age is not so important here, but there is a direct relationship between biological aging and NAD+ depletion.
For example, healthy centenarians tend not to have depleted NAD+ levels. Further, its depletion (in those in whom it is depleted) is then a causal factor for many age-related diseases:
❝Remarkably, ageing is accompanied by a gradual decline in tissue and cellular NAD+ levels in multiple model organisms, including rodents and humans.
This decline in NAD+ levels is linked causally to numerous ageing-associated diseases, including cognitive decline, cancer, metabolic disease, sarcopenia and frailty.
Many of these ageing-associated diseases can be slowed down and even reversed by restoring NAD+ levels.❞
~ Dr. Rosalba Perrone et al.
Read in full: NAD+ metabolism and its roles in cellular processes during ageing
As for restoring those NADᐩ levels, that does help in interventional trials, whether by supplementing directly, or with NAD precursors*:
❝NAD+ levels steadily decline with age, resulting in altered metabolism and increased disease susceptibility.
Restoration of NAD+ levels in old or diseased animals can promote health and extend lifespan, prompting a search for safe and efficacious NAD-boosting molecules that hold the promise of increasing the body’s resilience, not just to one disease, but to many, thereby extending healthy human lifespan.❞
~ Dr. David Sinclair et al.
Read more: Therapeutic Potential of NAD-Boosting Molecules: The In Vivo Evidence
*There are actually also other NAD-boosting molecules besides NAD itself and its precursors. For example, the liver will not produce NADᐩ unless it has aminocarboxymuconate-semialdehyde decarboxylase (or “ACMSD”, to its friends), which limits the production of NADᐩ. Why, you ask? The theory is that it is a kind of evolutionary conservativism, much like not lighting a fire without the ability to put it out. In any case, taking ACMSD-blockers will thus result in an increased endogenous production of NADᐩ.
You can read about this here:
De novo NAD+ synthesis enhances mitochondrial function and improves health
Nor is taking supplements or drugs the only way to get more of it; there’s an enzyme nicotinamide phosphoribosyltransferase (“NAMPT”, to its friends) involved in the synthesis of NADᐩ, and exercise boosts levels by 127% (i.e., it more than doubles the levels), based on a modest three-week exercise bike regimen:
Skeletal muscle NAMPT is induced by exercise in humans
And to underline that point, another study found that resistance training (so, a different kind of exercise from that of the previous study) boosts levels of NADᐩ itself by the same 127%:
One way to get more out of NADᐩ
We’ll get straight to the point: it works very well paired with a senolytic agent, i.e. something that kills aging cells so that they get recycled sooner:
NAD+, Senolytics, or Pyruvate for Healthy Aging?
To read more about senolytics, check out:
Fisetin: The Anti-Aging Assassin
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
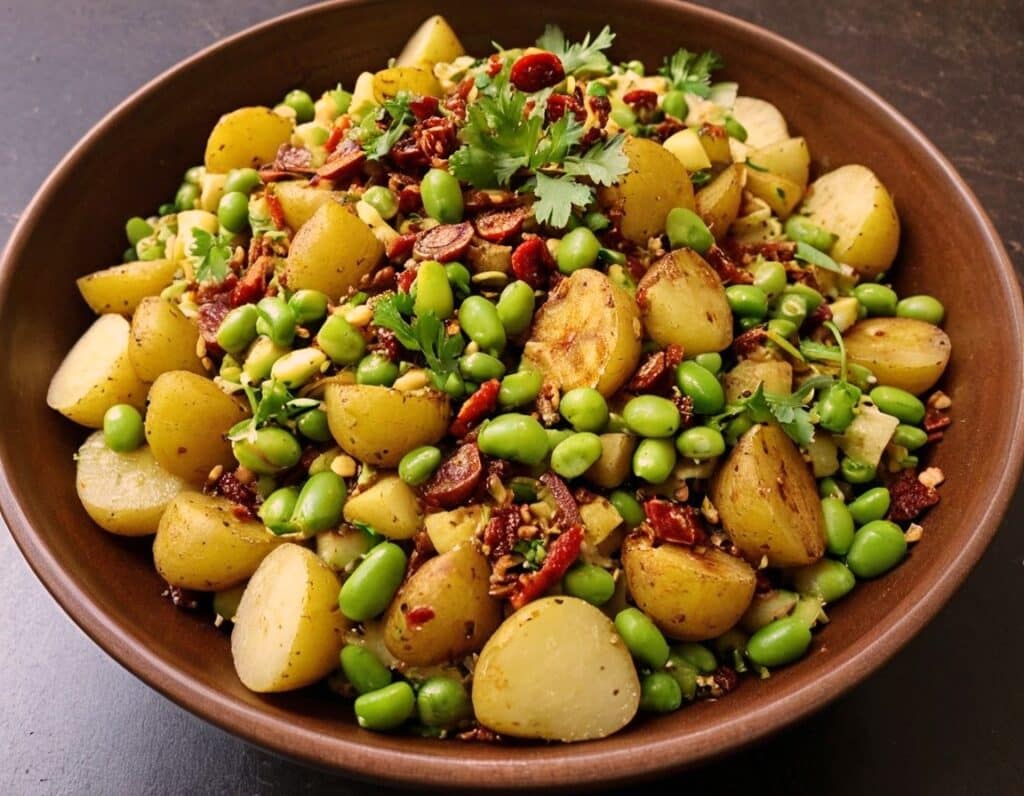
Chaat Masala Spiced Potato Salad With Beans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is an especially gut-healthy dish; the cooked-and-cooled potatoes are not rich with resistant starches (that’s good), the beans bring protein (as well as more fiber and micronutrients), and many of the spices bring their own benefits. A flavorful addition to your table!
You will need
- 1 lb new potatoes, boiled or steamed, with skin on, quartered, cooled ← this is a bit of a “mini recipe”, but we expect you can handle it
- 5 oz blanched broad beans
- 2 oz sun-dried tomatoes, chopped
- ¼ bulb garlic, crushed
- 1 tbsp extra virgin olive oil
- 2 tsp amchoor
- 2 tsp ground cumin
- 2 tsp ground coriander
- 1 tsp ground ginger
- 1 tsp ground asafoetida
- 1 tsp black pepper, coarse ground
- 1 tsp red chili powder
- 1 tsp ground turmeric
- ½ tsp MSG or 1 tsp low-sodium salt
- Juice of ½ lemon
And then…
- To garnish: finely chopped cilantro, or if you have the “cilantro tastes like soap” gene, then substitute with parsley
- To serve: a nice chutney; you can use our Spiced Fruit & Nut Chutney recipe
Method
(we suggest you read everything at least once before doing anything)
1) Mix all the ingredients from the main section, ensuring an even distribution on the spices.
2) Add the garnish, and serve with the chutney. That’s it. There was more work in the prep (and potentially, finding all the ingredients) today.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we scored all five today!
- Lycopene’s Benefits For The Gut, Heart, Brain, & More ← don’t underestimate those sun-dried tomatoes, either!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: