Anise vs Diabetes & Menopause
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What A Daily Gram Of Anise Can Do
Anise, specifically the seed of the plant, also called aniseed, is enjoyed for its licorice taste—as well as its medicinal properties.
Let’s see how well the science lives up to the folk medicine…
What medicinal properties does it claim?
The main contenders are:
- Reduces menopause symptoms
- Reduces blood sugar levels
- Reduces inflammation
Does it reduce menopause symptoms?
At least some of them! Including hot flashes and bone density loss. This seems to be due to the estrogenic-like activity of anethole, the active compound in anise that gives it these effects:
Estrogenic activity of isolated compounds and essential oils of Pimpinella species
1g of anise/day yielded a huge reduction in frequency and severity of hot flashes, compared to placebo*:
*you may be wondering what the placebo is for 1g of a substance that has a very distinctive taste. The researchers used capsules, with 3x330g as the dose, either anise seed or potato starch.
❝In the experimental group, the frequency and severity of hot flashes before the treatment were 4.21% and 56.21% and, after that, were 1.06% and 14.44% at the end of the fourth week respectively. No change was found in the frequency and severity of hot flashes in the control group. The frequency and severity of hot flashes was decreased during 4 weeks of follow up period. P. anisum is effective on the frequency and severity of hot flashes in postmenopausal women. ❞
See for yourself: The Study on the Effects of Pimpinella anisum on Relief and Recurrence of Menopausal Hot Flashes
As for bone mineral density, we couldn’t find a good study for anise, but we did find this one for fennel, which is a plant of the same family and also with the primary active compound anethole:
The Prophylactic Effect of Fennel Essential Oil on Experimental Osteoporosis
That was a rat study, though, so we’d like to see studies done with humans.
Summary on this one: it clearly helps against hot flashes (per the very convincing human study we listed above); it probably helps against bone mineral density loss.
Does it reduce blood sugar levels?
This one got a flurry of attention all so recently, on account of this research review:
Review on Anti-diabetic Research on Two Important Spices: Trachyspermum ammi and Pimpinella anisum
If you read this (and we do recommend reading it! It has a lot more information than we can squeeze in here!) one of the most interesting things about the in vivo anti-diabetic activity of anise was that while it did lower the fasting blood glucose levels, that wasn’t the only effect:
❝Over a course of 60 days, study participants were administered seed powders (5 g/d), which resulted in significant antioxidant, anti-diabetic, and hypolipidemic effects.
Notably, significant reductions in fasting blood glucose levels were observed. This intervention also elicited alterations in the lipid profile, LPO, lipoprotein levels, and the high-density lipoprotein (HDL) level.
Moreover, the serum levels of essential antioxidants, such as beta carotene, vitamin C, vitamin A, and vitamin E, which are typically decreased in diabetic patients, underwent a reversal.❞
That’s just one of the studies cited in that review (the comments lightly edited here for brevity), but it stands out, and you can read that study in its entirety (it’s well worth reading).
Rajeshwari et al, bless them, added a “tl;dr” at the top of their already concise abstract; their “tl;dr” reads:
❝Both the seeds significantly influenced almost all the parameters without any detrimental effects by virtue of a number of phytochemicals, vitamins and minerals present in the seeds having therapeutic effects.❞
Shortest answer: yes, yes it does
Does it fight inflammation?
This one’s quick and simple enough: yes it does; it’s full of antioxidants which thus also have an anti-inflammatory effect:
Review of Pharmacological Properties and Chemical Constituents of Pimpinella anisum
…which can also be used an essential oil, applied topically, to fight both pain and the inflammation that causes it—at least in rats and mice:
❝Indomethacin and etodolac were treated reference drugs for the anti-inflammatory activity. Aspirin and morphine hydrochloride were treated reference drugs for the analgesic activity. The results showed that fixed oil of P. anisum has an anti-inflammatory action more than etodolac and this effect was as strong as indomethacin. P. anisum induces analgesic effect comparable to that of 100 mg/kg Aspirin and 10 mg/kg morphine at 30 th min. of the study❞
Summary of this section:
- Aniseeds are a potent source of antioxidants, which fight inflammation.
- Anise essential oil is probably also useful as a topical anti-inflammatory and analgesic agent, but we’d like to see human tests to know for sure.
Is it safe?
For most people, enjoyed in moderation (e.g., within the dosage parameters described in the above studies), anise is safe. However:
- If you’re allergic to it, it won’t be safe
- Its estrogen-mimicking effects could cause problems if you have (or have a higher risk factor for) breast cancer, ovarian cancer, or endometriosis.
- For most men, the main concern is that it may lower sperm count.
Where to get it?
As ever, we don’t sell it (or anything else), but for your convenience, you can buy the seeds in bulk on Amazon, or in case you prefer it, here’s an example of it available as an essential oil.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Does Eating Shellfish Contribute To Gout?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I have a question about seafood as healthy, doesn’t eating shellfish contribute to gout?❞
It can do! Gout (a kind of inflammatory arthritis characterized by the depositing of uric acid crystals in joints) has many risk factors, and diet is one component, albeit certainly the most talked-about one.
First, you may be wondering: isn’t all arthritis inflammatory? Since arthritis is by definition the inflammation of joints, this is a reasonable question, but when it comes to classifying the kinds, “inflammatory” arthritis is caused by inflammation, while “non-inflammatory” arthritis (a slightly confusing name) merely has inflammation as one of its symptoms (and is caused by physical wear-and-tear). For more information, see:
- Tips For Avoiding/Managing Rheumatoid Arthritis ←inflammatory
- Tips For Avoiding/Managing Osteoarthritis ← “non-inflammatory”
As for gout specifically, top risk factors include:
- Increasing age: risk increases with age
- Being male: women do get gout, but much less often
- Hypertension: all-cause hypertension is the biggest reasonably controllable factor
There’s not a lot we can do about age (but of course, looking after our general health will tend to slow biological aging, and after all, diseases only care about the state of our body, not what the date on the calendar is).
As for sex, this risk factor is hormones, and specifically has to do with estrogen and testosterone’s very different effects on the immune system (bearing in mind that chronic inflammation is a disorder of the immune system). However, few if any men would take up feminizing hormone therapy just to lower their gout risk!
That leaves hypertension, which happily is something that we can all (barring extreme personal circumstances) do quite a bit about. Here’s a good starting point:
Hypertension: Factors Far More Relevant Than Salt
…and for further pointers:
How To Lower Your Blood Pressure (Cardiologists Explain)
As for diet specifically (and yes, shellfish):
The largest study into this (and thus, one of the top ones cited in a lot of other literature) looked at 47,150 men with no history of gout at the baseline.
So, with the caveat that their findings could have been different for women, they found:
- Eating meat in general increased gout risk
- Narrowing down specific meats: beef, pork, and lamb were the worst offenders
- Eating seafood in general increased gout risk
- Narrowing down specific seafoods: all seafoods increased gout risk within a similar range
- As a specific quirk of seafoods: the risk was increased if the man had a BMI under 25
- Eating dairy in general was not associated with an increased risk of gout
- Narrowing down specific dairy foods: low-fat dairy products such as yogurt were associated with a decreased risk of gout
- Eating purine-rich vegetables in general was not associated with an increased risk of gout
- Narrowing down to specific purine-rich vegetables: no purine-rich vegetable was associated with an increase in the risk of gout
Dairy products were included in the study, as dairy products in general and non-fermented dairy products in particular are often associated with increased inflammation. However, the association was simply not found to exist when it came to gout risk.
Purine-rich vegetables were included in the study, as animal products highest in purines have typically been found to have the worst effect on gout. However, the association was simply not found to exist when it came to plants with purines.
You can read the full study here:
Purine-Rich Foods, Dairy and Protein Intake, and the Risk of Gout in Men
So, the short answer to your question of “doesn’t eating shellfish contribute to the risk of gout” is:
Yes, it can, but occasional consumption probably won’t result in gout unless you have other risk factors going against you.
If you’re a slim male 80-year-old alcoholic smoker with hypertension, then definitely do consider skipping the lobster, but honestly, there may be bigger issues to tackle there.
And similarly, obviously skip it if you have a shellfish allergy, and if you’re vegan or vegetarian or abstain from shellfish for religious reasons, then you can certainly live very healthily without ever having any.
See also: Do We Need Animal Products, To Be Healthy?
For most people most of the time, a moderate consumption of seafood, including shellfish if you so desire, is considered healthy.
As ever, do speak with your own doctor to know for sure, as your individual case may vary.
For reference, this question was surely prompted by the article:
Lobster vs Crab – Which is Healthier?
Take care!
Share This Post
-
Health & Happiness From Outside & In
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A friend in need…
In a recent large (n=3,486) poll across the US:
- 90% of people aged 50 and older say they have at least one close friend
- 75% say they have enough close friends
- 70% of those with a close friend say they can definitely count on them to provide health-related support
However, those numbers shrink by half when it comes to people whose physical and/or mental health is not so great, resulting in a negative feedback loop of fewer close friends whom one sees less often, and progressively worse physical and/or mental health. In other words, the healthier you are, the more likely you are to have a friend who’ll support you in your health:
Read in full: Friendships promote healthier living in older adults, says new survey
Related: How To Beat Loneliness & Isolation
Kindness makes a difference to healthcare outcomes
Defining kindness as action-oriented, positively focused, and purposeful in nature, this sets kindness apart from compassion and empathy, when it’s otherwise often been conflated with those, and thus overlooked. This also means that kindness can still be effected when clinicians are too burned-out to be compassionate, and/or when patients are not in a state of mind where empathy is useful.
Furthermore, unkindness (again, as defined by this review) was found in large studies to be the root cause of ¾ of patient harm events in hospital settings. This means that far from being a wishy-washy abstraction, kindness/unkindness can be a very serious factor when it comes to healthcare outcomes:
Read in full: Review suggests kindness could make for better health care
Related: The Human Touch vs AI, The Doctor That Never Tires
The gift of health?
🎵 Last Christmas, I gave you my heart
Which turned out to be a silly idea
This year, to save me from tears
I’ll just get you a Fitbit or something🎵Health & happiness go hand in hand, so does that make health stuff a good gift? It can do! But there are also plenty of opportunities for misfires.
For example, getting someone a gym membership when they don’t have time for that may not help them at all, and sports equipment that they’ll use once and then leave to gather dust might not be great either. In contrast, the American Heart Association recommends to first consider what they enjoy doing, and work with that, and ideally make it something versatile and/or portable. Wearable gadgets are a fine option for many, but a gift doesn’t have to be fancy to be good—with a blood pressure monitoring cuff being a suggestion from Dr. Sperling (a professor of preventative cardiology):
Read in full: Oh, there’s no gift like health for the holidays
Related: Here’s Where Activity Trackers Help (And Also Where They Don’t)
How you use social media matters more than how much
A study commissioned by the European Commission’s Joint Research Centre found that while the quantity of time one spends on social media is not associated (positively or negatively) with loneliness, they did find a correlation between passive (as opposed to engaged) use of social media, and loneliness. In other words, people who were chatting with friends less, were more lonely! Shocking news.
While the findings may seem obvious, it does present a call-to-action for anyone who is feeling lonely: to use social media not just to see what everyone else is up to, but also, to reach out to people.
Read in full: Unpacking the link between social media and loneliness
Related: Make Social Media Work For Your Mental Health Rather Than Against It
Gut-only antidepressants
Many antidepressants work by increasing serotonin levels in the brain; a new study suggests that targeting antidepressants to work only in the gut (which is where serotonin is made, not the brain) could not only be an effective treatment for mood disorders, but also cause fewer adverse side-effects:
Read in full: Antidepressants may act in gut to reduce depression and anxiety
Related: Antidepressants: Personalization Is Key!
Take care!
Share This Post
-
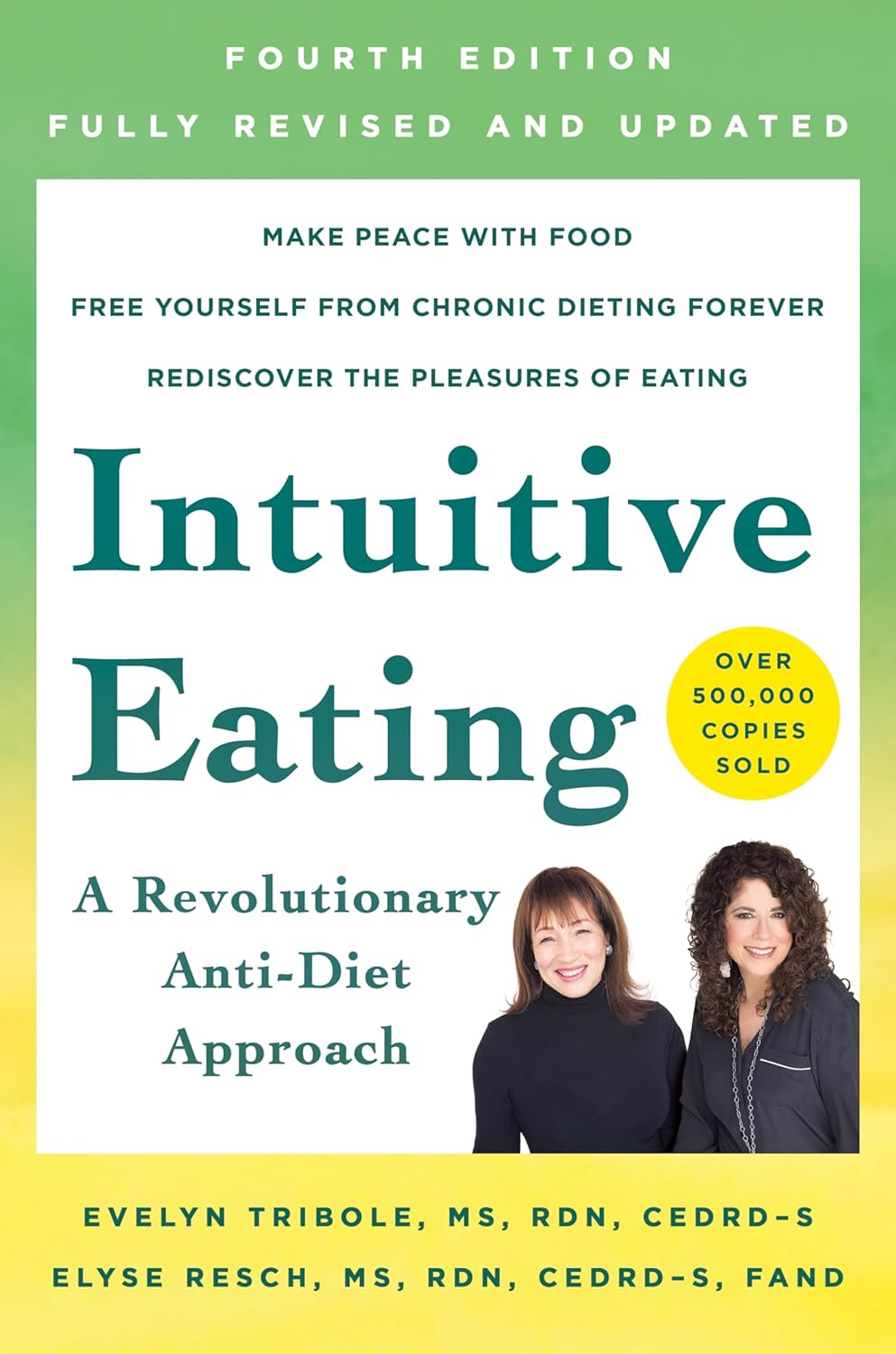
Intuitive Eating – by Evelyn Tribole and Elyse Resch
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be given to wonder: if this is about intuitive eating, and an anti-diet approach, why a whole book?
There’s a clue in the other part of the title: “4th Edition”.
The reason there’s a 4th edition (and before it, a 3rd and 2nd edition) is because this book is very much full of science, and science begets more science, and the evidence just keeps on rolling in.
While neither author is a doctor, each has a sizeable portion of the alphabet after their name (more than a lot of doctors), and this is an incredibly well-evidenced book.
The basic premise from many studies is that restrictive dieting does not work well long-term for most people, and instead, better is to make use of our bodies’ own interoceptive feedback.
You see, intuitive eating is not “eat randomly”. We do not call a person “intuitive” because they speak or act randomly, do we? Same with diet.
Instead, the authors give us ten guiding principles (yes, still following the science) to allow us a consistent “finger on the pulse” of what our body has to say about what we have been eating, and what we should be eating.
Bottom line: if you want to be a lot more in tune with your body and thus better able to nourish it the way it needs, this book is literally on the syllabus for many nutritional science classes, and will stand you in very good stead!
Share This Post
Related Posts
-
How to Use Topical Estrogen Cream For Aging Skin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Sam Ellis, dermatologist, explains:
Tackling the cause
Estrogen is important for very many aspects of health beyond the sexual aspects. When it comes to skin, a drop in estrogen (usually because of menopause) leads to changes like collagen loss, dryness, reduced elasticity, and slower wound healing. Applying estrogen creams to the skin can reverse these changes.
If your estrogen levels are already within normal pre-menopausal female ranges, by the way, there isn’t so much science to indicate its benefit when used topically. If you are already on systemic HRT (i.e., you take estrogen already to raise your blood estrogen levels and affect your body in its entirety), you may or may not gain extra benefits from the topical cream, depending on factors such as your estrogen dose, your route of administration, your cardiovascular health, and other factors.
For those with lower estrogen and not currently on HRT, you may be wondering: can topical estrogen cream affect systemic estrogen levels? And the answer is that it mostly depends on the dose. In other words: it’s definitely possible, but for most people it’s unlikely.
As ever, if thinking of taking up any hormonal treatment, do consult an endocrinologist and/or gynecologist, and if you have an increased breast cancer risk (for example genetically or prior history), then an oncologist too, just to be safe.
That sounds like a lot of scary things, but mostly it’s just to be on the safe side. The dose of estrogen is very low in topical creams, and even then, only a tiny amount is used per day.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- “Why Does It Hurt When I Have Sex?” (And What To Do About It) ← because topical estrogen is not just for your face! Yes, you can use it down there too and it’s commonly prescribed for exactly this use.
- Hormones & Health, Beyond The Obvious
- The Hormone Therapy That Reduces Breast Cancer Risk & More
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Top 5 Anti-Aging Exercises
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are some exercises that get called such things as “The King of Exercises!”, but how well-earned is that title and could it be that actually a mix of the top few is best?
The Exercises
While you don’t have to do all 5, your body will thank you if you are able to:
- Plank: strengthens most of the body, and can reduce back pain while improving posture.
- Squats: another core-strengthening exercise, this time with an emphasis on the lower body, which makes for strong foundations (including strong ankles, knees, and hips). Improves circulation also, and what’s good for circulation is good for the organs, including the brain!
- Push-ups: promotes very functional strength and fitness; great for alternating with planks, as despite their similar appearance, they work the abs and back more, respectively.
- Lunges: these are great for lower body strength and stability, and doing these greatly reduces the risk of falling.
- Glute Bridges: this nicely rounds off one’s core strength, increasing stability and improving posture, as well as reducing lower back pain too.
If the benefits of these seem to overlap a little, it’s because they do! But each does some things that the others don’t, so put together, they make for a very well-balanced workout.
For advice on how to do each of them, plus more about the muscles being used and the benefits, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
I’m feeling run down. Why am I more likely to get sick? And how can I boost my immune system?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It has been a long winter, filled with many viruses and cost-of-living pressures, on top of the usual mix of work, study, life admin and caring responsibilities.
Stress is an inevitable part of life. In short bursts, our stress response has evolved as a survival mechanism to help us be more alert in fight or flight situations.
But when stress is chronic, it weakens the immune system and makes us more vulnerable to illnesses such as the common cold, flu and COVID.
Pexels/Ketut Subiyanto Stress makes it harder to fight off viruses
When the immune system starts to break down, a virus that would normally have been under control starts to flourish.
Once you begin to feel sick, the stress response rises, making it harder for the immune system to fight off the disease. You may be sick more often and for longer periods of time, without enough immune cells primed and ready to fight.
In the 1990s, American psychology professor Sheldon Cohen and his colleagues conducted a number of studies where healthy people were exposed to an upper respiratory infection, through drops of virus placed directly into their nose.
These participants were then quarantined in a hotel and monitored closely to determine who became ill.
One of the most important factors predicting who got sick was prolonged psychological stress.
Cortisol suppresses immunity
“Short-term stress” is stress that lasts for a period of minutes to hours, while “chronic stress” persists for several hours per day for weeks or months.
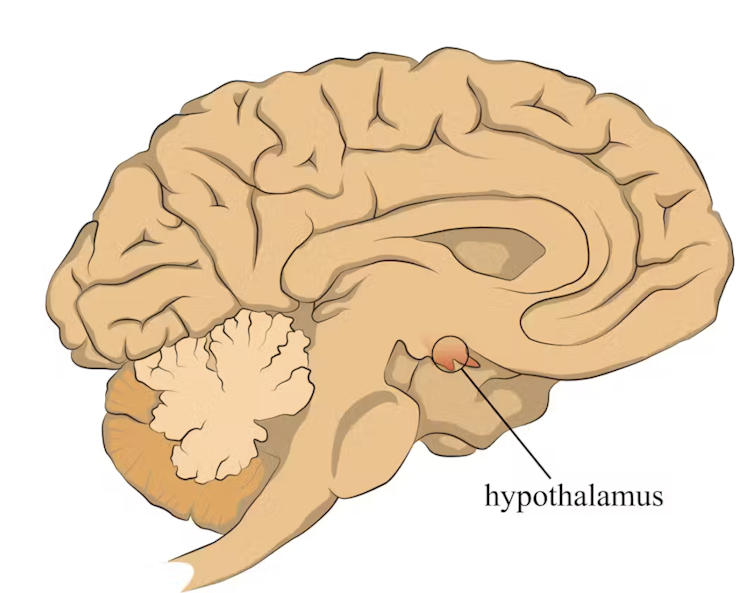
When faced with a perceived threat, psychological or physical, the hypothalamus region of the brain sets off an alarm system. This signals the release of a surge of hormones, including adrenaline and cortisol.
The hypothalamus sets off an alarm system in response to a real or perceived threat. stefan3andrei/Shutterstock In a typical stress response, cortisol levels quickly increase when stress occurs, and then rapidly drop back to normal once the stress has subsided. In the short term, cortisol suppresses inflammation, to ensure the body has enough energy available to respond to an immediate threat.
But in the longer term, chronic stress can be harmful. A Harvard University study from 2022 showed that people suffering from psychological distress in the lead up to their COVID infection had a greater chance of experiencing long COVID. They classified this distress as depression, probable anxiety, perceived stress, worry about COVID and loneliness.
Those suffering distress had close to a 50% greater risk of long COVID compared to other participants. Cortisol has been shown to be high in the most severe cases of COVID.
Stress causes inflammation
Inflammation is a short-term reaction to an injury or infection. It is responsible for trafficking immune cells in your body so the right cells are present in the right locations at the right times and at the right levels.
The immune cells also store a memory of that threat to respond faster and more effectively the next time.
Initially, circulating immune cells detect and flock to the site of infection. Messenger proteins, known as pro-inflammatory cytokines, are released by immune cells, to signal the danger and recruit help, and our immune system responds to neutralise the threat.
During this response to the infection, if the immune system produces too much of these inflammatory chemicals, it can trigger symptoms such as nasal congestion and runny nose.
Our immune response can trigger symptoms such as a runny nose. Alyona Mandrik/Shutterstock What about chronic stress?
Chronic stress causes persistently high cortisol secretion, which remains high even in the absence of an immediate stressor.
The immune system becomes desensitised and unresponsive to this cortisol suppression, increasing low-grade “silent” inflammation and the production of pro-inflammatory cytokines (the messenger proteins).
Immune cells become exhausted and start to malfunction. The body loses the ability to turn down the inflammatory response.
Over time, the immune system changes the way it responds by reprogramming to a “low surveillance mode”. The immune system misses early opportunities to destroy threats, and the process of recovery can take longer.
So how can you manage your stress?
We can actively strengthen our immunity and natural defences by managing our stress levels. Rather than letting stress build up, try to address it early and frequently by:
1) Getting enough sleep
Getting enough sleep reduces cortisol levels and inflammation. During sleep, the immune system releases cytokines, which help fight infections and inflammation.
2) Taking regular exercise
Exercising helps the lymphatic system (which balances bodily fluids as part of the immune system) circulate and allows immune cells to monitor for threats, while sweating flushes toxins. Physical activity also lowers stress hormone levels through the release of positive brain signals.
3) Eating a healthy diet
Ensuring your diet contains enough nutrients – such as the B vitamins, and the full breadth of minerals like magnesium, iron and zinc – during times of stress has a positive impact on overall stress levels. Staying hydrated helps the body to flush out toxins.
4) Socialising and practising meditation or mindfulness
These activities increase endorphins and serotonin, which improve mood and have anti-inflammatory effects. Breathing exercises and meditation stimulate the parasympathetic nervous system, which calms down our stress responses so we can “reset” and reduce cortisol levels.
Sathana Dushyanthen, Academic Specialist & Lecturer in Cancer Sciences & Digital Health| Superstar of STEM| Science Communicator, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: