How Much Alcohol Does It Take To Increase Cancer Risk?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Alcohol is, of course, unhealthy. Not even the famous “small glass of red” is recommended:
Alcohol also increases all-cause mortality at any dose (even “low-risk drinking”):
Alcohol Consumption Patterns and Mortality Among Older Adults
…and the World Health Organization has declared that the only safe amount of alcohol is zero:
WHO: No level of alcohol consumption is safe for our health
But what of alcohol and cancer? According to the American Association of Cancer Research’s latest report, more than half of Americans do not know that alcohol increases the risk of cancer:
Source: AACR Cancer Progress Report
Why/how does alcohol increase the risk of cancer?
There’s an obvious aspect and a less obvious but very important aspect:
- The obvious: alcohol damages almost every system in the body, and so it’s little surprise if that includes systems whose job it is to keep us safe from cancer.
- The less obvious: alcohol is largely metabolized by certain enzymes that have an impact on DNA repair, such as alcohol dehydrogenases and aldehyde dehydrogenases, amongst others, and noteworthily, acetaldehyde (the main metabolite of alcohol) is itself genotoxic.
Read more: Alcohol & Cancer
This is important, because it means alcohol also increases the risk of cancers other than the obvious head/neck, laryngeal, esophageal, liver, and colorectal cancers.
However, those cancers are of course the most well-represented of alcohol-related cancers, along with breast cancer (this has to do with alcohol’s effect on estrogen metabolism).
If you’re curious about the numbers, and the changes in risk if one reduces/quits/reprises drinking:
❝The increased alcohol-related cancer incidence was associated with dose; those who changed from nondrinking to mild (adjusted hazard ratio [aHR], 1.03; 95% CI, 1.00-1.06), moderate (aHR, 1.10; 95% CI, 1.02-1.18), or heavy (aHR, 1.34; 95% CI, 1.23-1.45) drinking levels had an associated higher risk than those who did not drink.
Those with mild drinking levels who quit drinking had a lower risk of alcohol-related cancer (aHR, 0.96; 95% CI, 0.92-0.99) than those who sustained their drinking levels.
Those with moderate (aHR, 1.07; 95% CI, 1.03-1.12) or heavy (aHR, 1.07; 95% CI, 1.02-1.12) drinking levels who quit drinking had a higher all cancer incidence than those who sustained their levels, but when quitting was sustained, this increase in risk disappeared.
Results of this study showed that increased alcohol consumption was associated with higher risks for alcohol-related and all cancers, whereas sustained quitting and reduced drinking were associated with lower risks of alcohol-related and all cancers.
Alcohol cessation and reduction should be reinforced for the prevention of cancer.❞
Source: Association Between Changes in Alcohol Consumption and Cancer Risk
Worried it’s too late?
If you’re reading this (and thus, evidently, still alive), it isn’t. It’s never too late (nor too early) to reduce, or ideally stop, drinking. Even if you already have cancer, drinking more alcohol will only exacerbate things, and abstaining from alcohol will improve your chances of recovery.
For a reassuring timeline of recovery from alcohol-related damage, see:
What Happens To Your Body When You Stop Drinking Alcohol
Want to stop, but have tried before and find it daunting?
There are a few ways to make it a lot easier:
Rethinking Drinking: How To Reduce Or Quit Alcohol
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Behaving During the Holidays
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝It’s hard to “behave” when it comes to holiday indulging…I’m on a low sodium, sugar restricted regimen from my doctor. Trying to get interested in bell peppers as a snack…wish me luck!❞
Good luck! Other low sodium, low sugar snacks include:
- Nuts! Unsalted, of course. We’re biased towards almonds 😉
- Mixed nuts are an especially healthy way to snack, though (assuming you don’t have an allergy, obviously)
- Air-popped popcorn (you can season it, just not with salt/sugar!)
- Fruit (but not fruit juice; it has to be in solid form)
- Peas (not a classic snack food, we know, but they can be enjoyed many ways)
- Seriously, try them frozen or raw! Frozen/raw peas are a great sweet snack.
- Chickpeas are great dried/roasted, by the way, and give much of the same pleasure as a salty snack without being salty! Obviously, this means cooking them without salt, but that’s fine, or if using tinned, choose “in water” rather than “in brine”
- Hummus is also a great healthy snack (check the ingredients for salt if not making it yourself, though) and can be enjoyed as a dip using raw vegetables (celery, carrot sticks, cruciferous vegetables, whatever you prefer)
Enjoy!
Share This Post
- Nuts! Unsalted, of course. We’re biased towards almonds 😉
-
The Best Exercise to Stop Your Legs From Giving Out
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Doug Weiss, seniors-specialist physio, has an exercise that stops your knees from being tricked into collapsing (which is very common) by a misfiring (also common) reflex.
Step up…
Setup to step up thus:
- Use a sturdy support like a countertop or chair.
- Have an aerobic step or similar firm surface to step onto.
When you’re ready:
- Stand facing away from the step.
- Place one hand on the support for stability.
- Step backwards up onto the step with your right leg, then your left leg, so both feet are on the step.
- Step forward to come back down.
Once you’re confident of the series of movements, do it without the support, and do it for a few minutes each day. Don’t worry about how easy it becomes; this is not, first and foremost, a strength-training exercise; you don’t have to start adding weights or anything (although of course you can if you want).
How it works: there’s a part of you called the Golgi tendon organ, and it can trigger a Golgi tendon reflex, which is one of the body’s equivalents of a steam valve. However, instead of letting off steam to avoid a boiler explosion, it collapses a joint to save it from overload. However, if not exercised regularly, it can get overly sensitive, causing it to mistake your mere bodyweight for an overload. So, it collapses, thinking it is saving you from snapping a tendon, but it’s not. By exercising in the way described, the Golgi tendon reflex will go back to only being triggered by an actual overload, not the mere act of stepping.
Writer’s note: this one’s interesting to me as I have a) a strong lower body b) hypermobile joints that thus occasionally just fold like laundry regardless. Could it be that this will fix that? I guess I’ll find out 🙂
Meanwhile, for more on all of the above plus a visual demonstration, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
What Nobody Teaches You About Strengthening Your Knees
Take care!
Share This Post
-
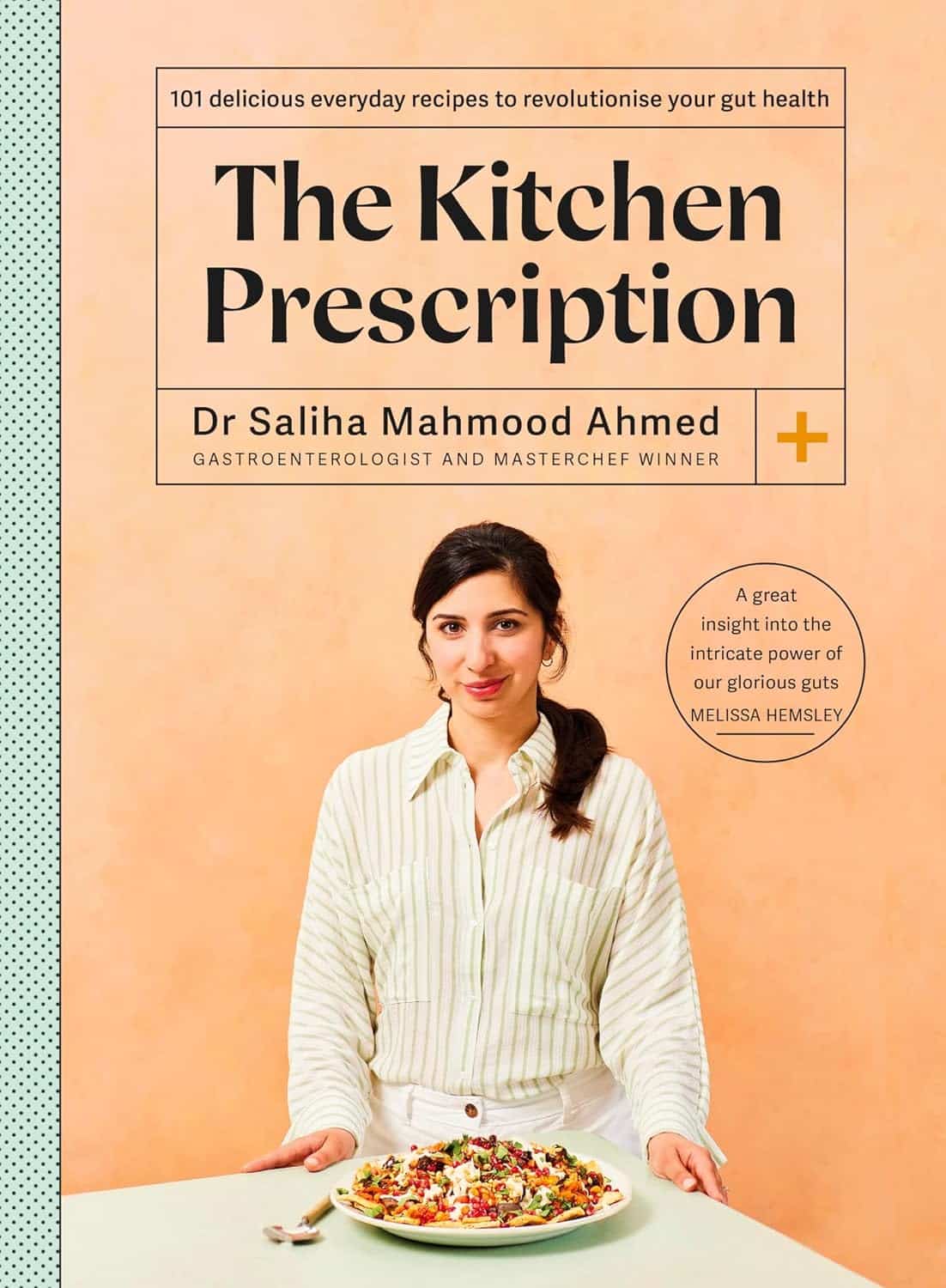
The Kitchen Prescription – by Saliha Mahmood Ahmed
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the biggest challenges facing anyone learning to cook more healthily, is keeping it tasty. What to cook when your biggest comfort foods all contain things you “should” avoid?
Happily for us, Dr. Ahmed is here with a focus on comfort food that’s good for your gut health. It’s incidentally equally good for the heart and good against diabetes… but Dr. Ahmed is a gastroenterologist, so that’s where she’s coming from with these.
There’s a wide range of 101 recipes here, including many tagged vegetarian, vegan, and/or gluten-free, as appropriate.
While this is not a vegetarian cookbook, Dr. Ahmed does consider the key components of a good diet to be, in order of quantity that should be consumed:
- Fruits and vegetables
- Whole grains
- Legumes
- Pulses
- Nuts and seeds
…and as such, the recipes are mostly plant-based.
The recipes are from all around the world, and/but the ingredients are mostly things that are almost universal. In the event that something might be hard-to-get, she suggests an appropriate substitution.
The recipes are straightforward and clear, as well as being beautifully illustrated.
All in all, a fine addition to anyone’s kitchen!
Get your copy of The Kitchen Prescription from Amazon today!
Share This Post
Related Posts
-
Hazelnuts vs Chestnuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing hazelnuts to chestnuts, we picked the hazelnuts.
Why?
This one’s not close.
In terms of macros, we have some big difference to start with, since chestnuts contain a lot more water and carbs whereas hazelnuts contain a lot more protein, fats, and fiber. The fats, as with most nuts, are healthy; in this case mostly being monounsaturated fat.
Because of the carbs and fiber being so polarized (i.e., chestnuts have most of the carbs and hazelnuts have most of the fiber), there’s a big difference in glycemic index; hazelnuts have a GI of 15 while chestnuts have a GI of 52.
In the category of vitamins, hazelnuts contain more of vitamins A, B1, B2, B3, B5, B6, and B9, while chestnuts contain more vitamin C.
When it comes to minerals, the story is similar: hazelnuts contain a lot more calcium, copper, iron, magnesium, manganese, phosphorus, and zinc, while chestnuts contain a tiny bit more potassium.
All in all, enjoy either or both, but nutritionally speaking, hazelnuts are a lot better in almost every way.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Superfood-Stuffed Squash
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This stuffed squash recipe is packed with so many nutrient-dense ingredients, yet it feels delightfully decadent—a great recipe to have up your sleeve ready for fall.
You will need
- 1 large or two medium butternut squashes, halved lengthways and seeds removed (keep them; they are full of nutrients! You can sprout them, or dry them to use them at your leisure), along with some of the flesh from the central part above where the seeds are, so that there is room for stuffing
- 2 cups low-sodium vegetable stock
- 1 cup wild rice, rinsed
- 1 medium onion, finely chopped
- ½ cup walnuts, roughly chopped
- ½ cup dried
cranberriesgoji berries ← why goji berries? They have even more healthful properties than cranberries, and cranberries are hard to buy without so much added sugar that the ingredients list looks like “cranberries (51%), sugar (39%), vegetable oil (10%)”, whereas when buying goji berries, the ingredients list says “goji berries”, and they do the same culinary job. - ¼ cup pine nuts
- ½ bulb garlic, minced
- 1 tbsp dried thyme or 2 tsp fresh thyme, destalked
- 1 tbsp dried rosemary or 2 tsp fresh rosemary, destalked
- 1 generous handful fresh parsley, chopped
- 1 tbsp chia seeds
- 1 tbsp nutritional yeast
- 1 tbsp black pepper, coarse ground
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil, for brushing and frying
- Aged balsamic vinegar, to serve (failing this, make a balsamic vinegar reduction and use that; it should have a thicker texture but still taste acidic and not too sweet; the thickness should come from the higher concentration of grape must and its natural sugars; no need to add sugar)
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400°F / 200°C.
2) Brush the cut sides of the squash with olive oil; sprinkle with a pinch of MSG/salt and a little black pepper (grind it directly over the squash if you are using a grinder; hold the grinder high though so that it distributes evenly—waiters in restaurants aren’t just being dramatic when they do that with pepper or Parmesan or such)
3) Arrange them cut-sides-down on a baking tray lined with baking paper, and roast for at least 30 minutes or until tender.
4) While that is roasting, add the chia seeds to the wild rice, and cook them in the low-sodium vegetable stock, using a rice cooker if available. It should take about the same length of time, but if the rice is done first, set it aside, and if the squash is done first, turn the oven down low to keep it warm.
5) Heat some oil in a sauté pan (not a skillet without high sides; we’re going to need space in a bit), and fry the chopped onion until translucent and soft. We could say “about 5 minutes” but honestly it depends on your pan as well as the heat and other factors.
6) Add the seasonings (herbs, garlic, black pepper, MSG/salt, nooch), and cook for a further 2 minutes, stirring thoroughly to distribute evenly.
7) Add the rice, berries, and nuts, cooking for a further 2 minutes, stirring constantly, ensuring everything is heated evenly.
8) Remove the squash halves from the oven, turn them over, and spoon the mixture we just made into them, filling generously.
9) Drizzle a lashing of the aged balsamic vinegar (or balsamic vinegar reduction), to serve.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Brown Rice vs Wild Rice – Which is Healthier?
- Why You Should Diversify Your Nuts!
- Goji Berries: Which Benefits Do They Really Have?
- Chia: The Tiniest Seeds With The Most Value
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- 10 Ways To Balance Blood Sugars
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Astrology, Mental health and the Economics of Well Being
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ultimately can the mental health system single-handedly address the concerns of inequality and economic access in society?
Around 75 per cent of the Indian population lives in rural areas, but their access to quality mental health care is limited and traditional approaches continue to be in use. The shortage is to such a large extent that there are only 0.7 physicians per 1000 population and only one psychiatrist for every 343,000 Indians. While over the years the mental health sector has seen major developments, like the 2017 mental health care act. This act establishes equal access for all citizens, to avail government-run or funded mental health services in the country. However, it does not bridge the gap in society as the majority of the population remains deeply unaware or unable to access these services.
While the uncertainties of the pandemic brought mental wellbeing to the forefront, the national budget for the sector dropped, making this an issue of human rights. This accessibility to services is further corroborated by the recurring financial expenses of medications and frequent visits to government clinics. The cost of sessions is steep and a single session is not ideal. Spending exorbitant amounts on healthcare is a burden most families can’t afford leading to debt. In the absence of insurance and healthcare schemes and provisions, therapy remains a luxury to many Indians.
Economic struggles are only one of the causes of this discerning gap in the mental health sector. Barriers caused by sexuality, gender, caste and religion also play a major role in mediating people’s perception and access to therapeutic services. The persistent stigma surrounding mental health, especially in India continues to be a hindrance to seeking help. The supernatural inhibitions and disparity in knowledge across communities only create more confusion. The notion that mental well being is an optional expense is popular, even though the country’s population is in a dire state. Data collected in a WHO report found that nearly 15 per cent of Indian adults need active intervention for one or more mental health issues.
The population disregards the very prevalence of such mental disorders and more than often finds it fruitless to receive treatment. Some who are open-minded fail to afford the hiked fees that therapists in urban settings charge, leaving them with no option. While for years Indians attributed the systemic weakness of the mental health system to the people’s attitudes, a 2016 survey showed more than 42% of people have positive attitudes toward mental wellbeing and treatment. While the skeptics remain, these underprivileged sections of society too struggle to gain the accessibility they deserve.
This is where astrology, tarot card reading and other spiritual practices, have created a market for themselves in the well-being industry. The sceptics, and those from poor socio-economic backgrounds resort to these local and easily accessible ways of coping, to instil the faith they so desperately need. Astrology is a layman’s substitute for therapy, or for some even a supplement when they cannot afford extended periods of treatment. Visiting a local astrologer in many ways breeds the self-awareness one would expect from a session in therapy. These practices even hold certain similarities to actual psychotherapy settings, in the way they define, and alleviate aspects of one’s personality and behaviour.
Very often one simply needs an explanation, or an answer to the ‘why’ no matter how scientifically rooted that response truly is. Astrologers impart a level of faith, that things will get better. For those in rural areas, struggling to provide the bare necessities to their family affording therapy is impossible, so their local psychic, astrologer or pandit becomes their anchor during emotional duress. Tarot cards and other practices primarily focus on the future and act as a guide point for how to deal with the things ahead. For a farmer coping with anxiety, access to anti-anxiety medication is strained, and so is therapy. His best bet remains to consult his next-door jyotish about his burdens.
A famous clinician Caroline Hexdall in an interview said that “ Part of the popularity of astrology and tarot today has to do with their universal nature”. With growing technology and the pervasiveness of social media, people can gain easy access to self-care and astrology resources. Apps and web pages provide daily tarot cards, zodiac signs readings and astrological predictions for people, and almost serve the purpose of a therapist. Is reading the lines on our palm, and checking the alignment of the stars enough to cure the mental illness they undergo? Is it a solution or a quick fix as a consequence of an ignorant healthcare system?
Several studies have also shown the deteriorating effects of depending on astrology. Cases of worsening and onset of depression, anxiety and personality disorders are common for those who use astrology as more than just a temporary coping mechanism. It also becomes a source of losing control, as every feeling is attributed to fate and destiny, instilling a sense of helplessness. Ultimately can the mental health system single-handedly address the concerns of inequality and economic access in society?
Maahira Jain is a third-year student at Ashoka University studying Psychology and Media studies. She is a movie buff and is extremely passionate about writing and traveling.
This article is republished from OpenAxis under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: