The Circadian Rhythm: Far More Than Most People Know
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Circadian Rhythm: Far More Than Most People Know
This is Dr. Satchidananda (Satchin) Panda, the scientist behind the discovery of the blue-light sensing cell type in the retina, and the many things it affects. But, he’s discovered more…
First, what you probably know (with a little more science)
Dr. Panda discovered that melanopsin, a photopigment, is “the primary candidate for photoreceptor-mediated entrainment”.
To put that in lay terms, it’s the brain’s go-to for knowing approximately what time of day or night it is, according to how much light there is (or isn’t), and how long it has (or hasn’t) been there.
But… the brain’s “go-to” isn’t the only method. By creating mice without melanopsin, he was able to find that they still keep a circadian rhythm, even in complete darkness:
Melanopsin (Opn4) Requirement for Normal Light-Induced Circadian Phase Shifting
In other words, it was a helpful, but not completely necessary, means of keeping a circadian rhythm.
So… What else is going on?
Dr. Panda and his team did a lot of science that is well beyond the scope of this main feature, but to give you an idea:
- With jargon: it explored the mechanisms and transcription translation negative feedback loops that regulate chronobiological processes, such as a histone lysine demathlyase 1a (JARID1a) that enhances Clock-Bmal1 transcription, and then used assorted genomic techniques to develop a model for how JARID1a works to moderate the level of Per transcription by regulating the transition between its repression and activation, and discovered that this heavily centered on hepatic gluconeogenesis and glucose homeostasis, facilitated by the protein cryptochrome regulating the fasting signal that occurs when glucagon binds to a G-protein coupled receptor, triggering CREB activation.
- Without jargon: a special protein tells our body how to respond to eating/fasting at different times of day—and conversely, certain physiological responses triggered by eating/fasting help us know what time of day it is.
- Simplest: our body keeps on its best cycle if we eat at the same time every day
This is important, because our circadian rhythm matters for a lot more than sleeping/waking! Take hormones, for example:
- Obvious hormones: testosterone and estrogen peak in the mornings around 9am, progesterone peaks between 10pm and 2am
- Forgotten hormones: cortisol peaks in the morning around 8:30am, melatonin peaks between 10pm and 2am
- More hormones: ghrelin (hunger hormone) peaks around 10am, leptin (satiety hormone) peaks 20 minutes after eating a certain amount of satiety-triggering food (protein does this most quickly), insulin is heavily tied to carbohydrate intake, but will still peak and trough according to when the body expects food.
What does this mean for us in practical terms?
For a start, it means that intermittent fasting can help guard against metabolic and related diseases (including inflammation, and thus also cancer, diabetes, arthritis, and more) a lot more if we practice it with our circadian rhythm in mind.
So that “8-hour window” for eating, that many intermittent fasting practitioners adhere to, is going to do much, much better if it’s 10am to 6pm, rather than, say, 4pm to midnight.
Additionally, Dr. Panda and his team found that a 12-hour eating window wasn’t sufficient to help significantly.
Some other take-aways:
- For reasons beyond the scope of this article, it’s good to exercise a) early b) before eating, so getting in some exercise between 8.30am and 10am is ideal
- It also means it’s beneficial to “front-load” eating, so a large breakfast at 10am, and smaller meals/snacks afterwards, is best.
- It also means that getting sunlight (even if cloud-covered) around 8.30am helps guard against metabolic disorders a lot, since the light remains the body’s go-to way of knowing the time.
- We realize that sunlight is not available at 8.30am at all latitudes at all times of year. Artificial is next-best.
- It also means sexual desire will typically peak in men in the mornings (per testosterone) and women in the evenings (per progesterone), but this is just an interesting bit of trivia, and not so relevant to metabolic health
What to do next…
Want to stabilize your own circadian rhythm in the best way, and also help Dr. Panda with his research?
His team’s (free!) app, “My Circadian Clock”, can help you track and organize all of the body’s measurable-by-you circadian events, and, if you give permission, will contribute to what will be the largest-yet human study into the topics covered today, to refine the conclusions and learn more about what works best.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
From immunotherapy to mRNA vaccines – the latest science on melanoma treatment explained
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More than 16,000 Australians will be diagnosed with melanoma each year. Most of these will be caught early, and can be cured by surgery.
However, for patients with advanced or metastatic melanoma, which has spread from the skin to other organs, the outlook was bleak until the advent of targeted therapies (that attack specific cancer traits) and immune therapies (that leverage the immune system). Over the past decade, these treatments have seen a significant climb in the number of advanced melanoma patients surviving for at least five years after diagnosis, from less than 10% in 2011 to around 50% in 2021.
While this is great news, there are still many melanoma patients who cannot be treated effectively with current therapies. Researchers have developed two exciting new therapies that are being evaluated in clinical trials for advanced melanoma patients. Both involve the use of immunotherapy at different times and in different ways.
The first results from these trials are now being shared publicly, offering insight into the future of melanoma treatment.
Svitlana Hulko/Shutterstock Immunotherapy before surgery
Immunotherapy works by boosting the power of a patient’s immune system to help kill cancer cells. One type of immunotherapy uses something called “immune checkpoint inhibitors”.
Immune cells carry “immune checkpoint” proteins, which control their activity. Cancer cells can interact with these checkpoints to turn off immune cells and hide from the immune system. Immune checkpoint inhibitors block this interaction and help keep the immune system activated to fight the cancer.
Results from an ongoing phase 3 trial using immune checkpoint inhibitors were recently published in the New England Journal of Medicine.
This trial used two types of immune checkpoint inhibitors: nivolumab, which blocks an immune checkpoint called PD-1, and ipilimumab, which blocks CTLA-4.
More than 16,000 Australians are diagnosed with melanoma each year. Delovely Pics/Shutterstock Some 423 patients (including many from Australia) were enrolled in the trial, and participants were randomly assigned to one of two groups.
The first group had surgery to remove their melanoma, and were then given immunotherapy (nivolumab) to help kill any remaining cancer cells. Giving a systemic (whole body) therapy such as immunotherapy after surgery is a standard way of treating melanoma. The second group received immunotherapy first (nivolumab plus ipilimumab) and then underwent surgery. This is a new approach to treating these cancers.
Based on previous observations, the researchers had predicted that giving patients immunotherapy while the whole tumour was still present would activate the tumour-fighting abilities of the patient’s immune system much better than giving it once the tumour had been removed.
Sure enough, 12 months after starting therapy, 83.7% of patients who received immunotherapy before surgery remained cancer-free, compared to 57.2% in the control group who received immunotherapy after surgery.
Based on these results, Australian of the year Georgina Long – who co-led the trial with Christian Blank from The Netherlands Cancer Institute – has suggested this method of immunotherapy before surgery should be considered a new standard of treatment for higher risk stage 3 melanoma. She also said a similar strategy should be evaluated for other cancers.
The promising results of this phase 3 trial suggest we might see this combination treatment being used in Australian hospitals within the next few years.
mRNA vaccines
Another emerging form of melanoma therapy is the post-surgery combination of a different checkpoint inhibitor (pembrolizumab, which blocks PD-1), with a messenger RNA vaccine (mRNA-4157).
While checkpoint inhibitors like pembrolizumab have been around for more than a decade, mRNA vaccines like mRNA-4157 are a newer phenomenon. You might be familiar with mRNA vaccines though, as the biotechnology companies Pfizer-BioNTech and Moderna released COVID vaccines based on mRNA technology.
mRNA-4157 works basically the same way – the mRNA is injected into the patient and produces antigens, which are small proteins that train the body’s immune system to attack a disease (in this case, cancer, and for COVID, the virus).
However, mRNA-4157 is unique – literally. It’s a type of personalised medicine, where the mRNA is created specifically to match a patient’s cancer. First, the patient’s tumour is genetically sequenced to figure out what antigens will best help the immune system to recognise their cancer. Then a patient-specific version of mRNA-4157 is created that produces those antigens.
The latest results of a three-year, phase 2 clinical trial which combined pembrolizumab and mRNA-4157 were announced this past week. Overall, 2.5 years after starting the trial, 74.8% of patients treated with immunotherapy combined with mRNA-4157 post-surgery remained cancer-free, compared to 55.6% of those treated with immunotherapy alone. These were patients who were suffering from high-risk, late-stage forms of melanoma, who generally have poor outcomes.
It’s worth noting these results have not yet been published in peer-reviewed journals. They’re available as company announcements, and were also presented at some cancer conferences in the United States.
Based on the results of this trial, the combination of pembrolizumab and the vaccine progressed to a phase 3 trial in 2023, with the first patients being enrolled in Australia. But the final results of this trial are not expected until 2029.
It is hoped this mRNA-based anti-cancer vaccine will blaze a trail for vaccines targeting other types of cancer, not just melanoma, particularly in combination with checkpoint inhibitors to help stimulate the immune system.
Despite these ongoing advances in melanoma treatment, the best way to fight cancer is still prevention which, in the case of melanoma, means protecting yourself from UV exposure wherever possible.
Sarah Diepstraten, Senior Research Officer, Blood Cells and Blood Cancer Division, WEHI (Walter and Eliza Hall Institute of Medical Research) and John (Eddie) La Marca, Senior Research Officer, Blood Cells and Blood Cancer, WEHI (Walter and Eliza Hall Institute of Medical Research)
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
The Stress Prescription (Against Aging!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Stress Prescription (Against Aging!)
This is Dr. Elissa Epel, whose work has for the past 20 years specialized in the effect of stress on aging. She’s led groundbreaking research on cortisol, telomeres, and telomerase, all in the context of aging, especially in women, as well as the relationship between stress and weight gain. She was elected member of the National Academy of Medicine for her work on stress pathways, and has been recognized as a key “Influencer in Aging” by the Alliance for Aging Research.
Indeed, she’s also been named in the top 0.1% of researchers globally, in terms of publication impact.
What’s that about stress and aging?
In her words,
❝Women with the highest levels of perceived stress have telomeres shorter on average by the equivalent of at least one decade of additional aging compared to low stress women❞
Source: Accelerated telomere shortening in response to life stress
We say “in her words”, as she is the top-listed author on this paper—an honour reserved for the lead researcher of any given study/paper.
However, we’d be remiss not to note that the second-listed author is Nobel Prize Laureate Dr. Elizabeth Blackburn. What a team! Maybe we’ll do a spotlight feature on Dr. Blackburn’s work one of these days, but for now, back to Dr. Epel…
What does she want us to do about it?
She has the following advice for us:
Let go of what we can’t control
This one is simple enough, and can be as simple as learning how to set anxiety aside, and taking up the practice of radical acceptance of what we cannot control.
Be challenged, not afraid
This is about eustress, and being the lion, not the gazelle. Dr. Epel uses the example of how when lions are hunting gazelles, both are stressed, but both are feeling the physiological effects of that stress in terms of the augmentation to their immediate abilities, but only one of them is suffering by it.
We’ll let her explain how to leverage this:
TED ideas | Here’s how you can handle stress like a lion, not a gazelle | Dr. Elissa Epel
Build resilience through controlled discomfort
Don’t worry, you don’t have to get chased by lions. A cold shower will do it! This is about making use of hormesis, the body’s ability to build resilience to stressors by small doses of controlled cortisol release—as for example when one undergoes thermal shock, which sounds drastic, but for most people, a cold shower (or even an ice bath) is safe enough.
You can read more about this here:
A Cold Shower A Day Keeps The Doctor Away
Connect with nature
You don’t have to hug a tree, but you do have get to a natural (or at least, natural-seeming) environment once in a while. Simply put, we did not evolve to be in the urban or even suburban settings where most of us spend most of our time. Getting to be around greenery with at least some kind of regularity is hugely beneficial. It doesn’t have to be a national park; a nice garden or local park can suffice, and potted plants at home are better than nothing. Even spending time in virtual reality “nature” is an option:
(you can see an example there, of the kind of scenery this study used)
Breathe deeply, and rest deeply
Mindful breathing, and good quality sleep, are very strongly evidence-based approaches to reduce stress, for example:
Practice gratitude to build optimism
Optimism has a huge positive impact on health outcomes, even when other factors (including socioeconomic factors, pre-existing conditions, and general reasons for one person to be more optimistic than another) are controlled for.
Read: Optimism and Cause-Specific Mortality: A Prospective Cohort Study
There are various ways to increase optimism, and practising gratitude is one of them—but that doesn’t necessarily mean abandoning realism, either:
How To Practise (Non-Toxic) Positivity
There are other ways too, though, and Dr. Epel discusses some with her friend and colleague, Dr. Elizabeth Blackburn, here:
Want to learn more from Dr. Epel?
We reviewed one of her books, The Telomere Effect, previously. It’s about what we can do to lengthen our telomeres (a key factor in health aging; effectively, being biologically younger). You also might enjoy her newer book, The Stress Prescription, as well as her blog.
Enjoy!
Share This Post
-
Beet “Kvass” With Ginger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Kvass is a popular drink throughout Eastern Europe, with several countries claiming it, but the truth is, kvass is older than nations (as in: nations, in general, any of them; nation states are a newer concept than is often realized), and its first recorded appearance was in the city state of Kyiv.
This one is definitely not a traditional recipe, as kvass is usually made from rye, but keeping true to its Eastern European roots with (regionally popular) beetroot, it’s nevertheless a great fermented drink, full of probiotic benefits, and this time, with antioxidants too.
It’s a little saltier than most things we give recipes for here, so enjoy it on hot sunny days as a great way to replenish electrolytes!
You will need (for 1 quart / 1 liter)
- 2¾ cups filtered or spring water
- 2 beets, roughly chopped
- 1 tbsp chopped fresh ginger
- 2 tsp salt (do not omit or substitute)
Method
(we suggest you read everything at least once before doing anything)
1) Sterilize a 1-quart jar with boiling water (carefully please)
2) Put all the ingredients in the jar and stir until the salt dissolves
3) Close the lid tightly and store in a cool dark place to ferment for 2 weeks
4) Strain the beets and ginger (they are now pickled and can be enjoyed in a salad or as a kimchi-like snack), pouring the liquid into a clean jar/bottle. This can be kept in the fridge for up to a month. Next time you make it, if you use ¼ cup of this as a “starter” to replace an equal volume of water in the original recipe, the fermentation will take days instead of weeks.
5) Serve! Best served chilled, but without ice, on a hot sunny day.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- What To Eat, Take, And Do Before A Workout
- Ginger Does A Lot More Than You Think
Take care!
Share This Post
Related Posts
-
What’s the difference between period pain and endometriosis pain?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Menstruation, or a period, is the bleeding that occurs about monthly in healthy people born with a uterus, from puberty to menopause. This happens when the endometrium, the tissue that lines the inside of the uterus, is shed.
Endometriosis is a condition that occurs when endometrium-like tissue is found outside the uterus, usually within the pelvic cavity. It is often considered a major cause of pelvic pain.
Pelvic pain significantly impacts quality of life. But how can you tell the difference between period pain and endometriosis?
Polina Zimmerman/Pexels Periods and period pain
Periods involve shedding the 4-6 millimetre-thick endometrial lining from the inside of the uterus.
As the lining detaches from the wall of the uterus, the blood vessels which previously supplied the lining bleed. The uterine muscles contract, expelling the blood and crumbled endometrium.
The crumbled endometrium and blood mostly pass through the cervix and vagina. But almost everyone back-bleeds via their fallopian tubes into their pelvic cavity. This is known as “retrograde menstruation”.
Most of the lining is shed through the vagina. Andrey_Popov/Shutterstock The process of menstrual shedding is caused by inflammatory substances, which also cause nausea, vomiting, diarrhoea, headaches, aches, pains, dizziness, feeling faint, as well as stimulating pain receptors.
These inflammatory substances are responsible for the pain and symptoms in the week before a period and the first few days.
For women with heavy periods, their worst days of pain are usually the heaviest days of their period, coinciding with more cramps to expel clots and more retrograde bleeding.
Many women also have pain when they are releasing an egg from their ovary at the time of ovulation. Ovulation or mid-cycle pain can be worse in those who bleed more, as those women are more likely to bleed into the ovulation follicle.
Around 90% of adolescents experience period pain. Among these adolescents, 20% will experience such severe period pain they need time off from school and miss activities. These symptoms are too often normalised, without validation or acknowledgement.
What about endometriosis?
Many symptoms have been attributed to endometriosis, including painful periods, pain with sex, bladder and bowel-related pain, low back pain and thigh pain.
Other pain-related conditions such migraines and chronic fatigue have also been linked to endometriosis. But these other pain-related symptoms occur equally often in people with pelvic pain who don’t have endometriosis.
One in five adolescents who menstrate experience severe symptoms. CGN089/Shutterstock Repeated, significant period and ovulation pain can eventually lead some people to develop persistent or chronic pelvic pain, which lasts longer than six months. This appears to occur through a process known as central sensitisation, where the brain becomes more sensitive to pain and other sensory stimuli.
Central sensitisation can occur in people with persistent pain, independent of the presence or absence of endometriosis.
Eventually, many people with period and/or persistent pelvic pain will have an operation called a laparoscopy, which allows surgeons to examine organs in the pelvis and abdomen, and diagnose and treat endometriosis.
Yet only 50% of those with identical pain symptoms who undergo a laparoscopy will end up having endometriosis.
Endometriosis is also found in pain-free women. So we cannot predict who does and doesn’t have endometriosis from symptoms alone.
How is this pain managed?
Endometriosis surgery usually involves removing lesions and adhesions. But at least 30% of people return to pre-surgery pain levels within six months or have more pain than before.
After surgery, emergency department presentations for pain are unchanged and 50% have repeat surgery within a few years.
Suppressing periods using hormonal therapies (such as continuous oral contraceptive pills or progesterone-only approaches) can suppress endometriosis and reduce or eliminate pain, independent of the presence or absence of endometriosis.
Not every type or dose of hormonal medications suits everyone, so medications need to be individualised.
The current gold-standard approach to manage persistent pelvic pain involves a multidisciplinary team approach, with the aim of achieving sustained remission and improving quality of life. This may include:
- physiotherapy for pelvic floor and other musculoskeletal problems
- management of bladder and bowel symptoms
- support for self-managing pain
- lifestyle changes including diet and exercise
- psychological or group therapy, as our moods, stress levels and childhood events can affect how we feel and experience pain.
Whether you have period pain, chronic pelvic pain or pain you think is associated with endometriosis, if you feel pain, it’s real. If it’s disrupting your life, you deserve to be taken seriously and treated as the whole person you are.
Sonia R. Grover, Senior Research Fellow, Murdoch Children’s Research Institute; Clinical Professor of Gynaecology, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
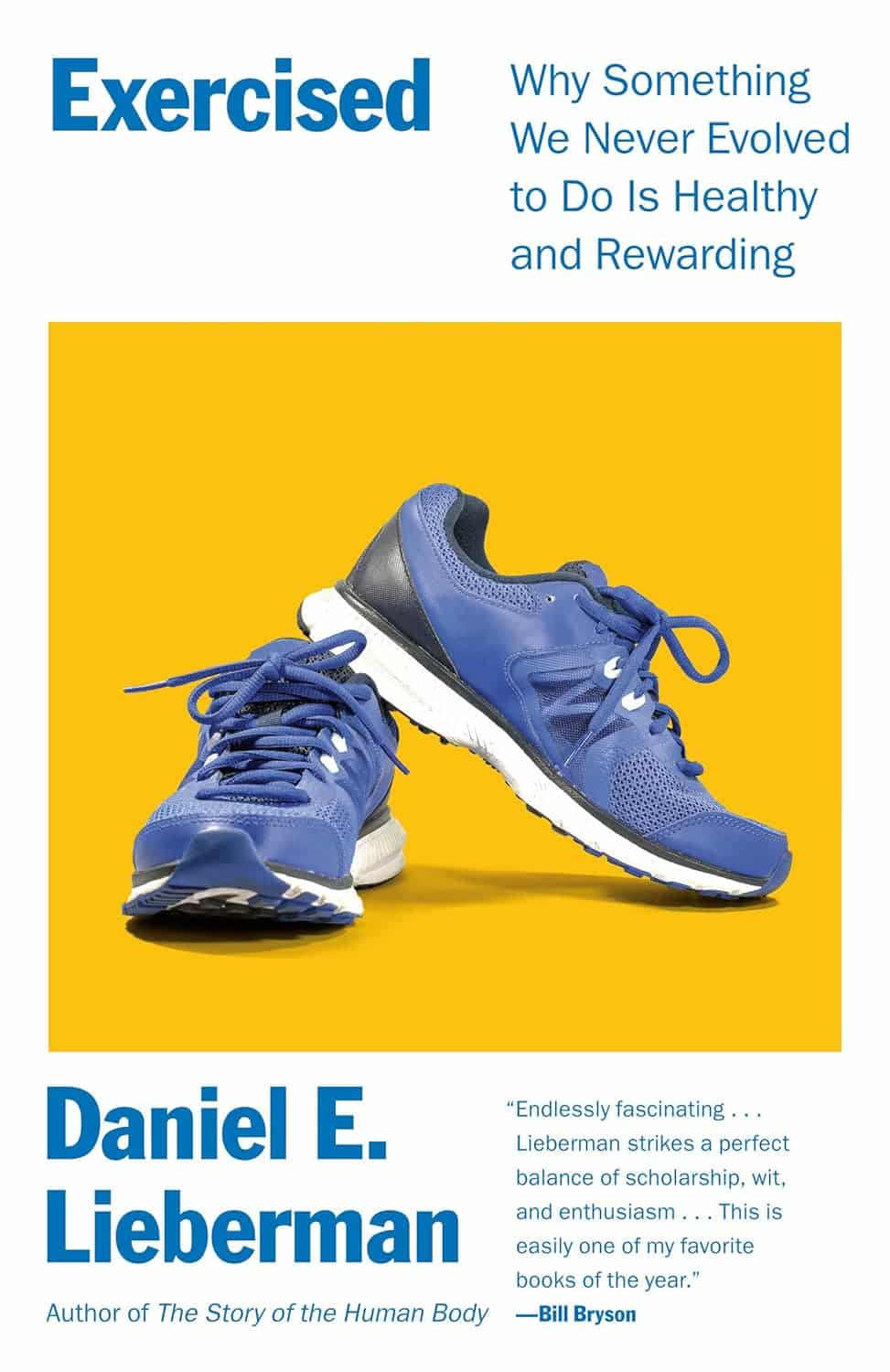
Exercised – by Dr. Daniel Lieberman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Surely the title is taking liberties? We must have evolved to exercise, right? Not exactly.
We evolved to conserve energy. Our strength-to-weight ratio is generally unimpressive, we cannot casually hang in trees, and we spend a third of our lives asleep.
Strengths that we do have, however, include a large brain and a versatile gut perfect for opportunism. Again, not the indicators of being evolved for exercise.
So, Dr. Lieberman tells us, if we’re not inclined to get up and go, that’s quite natural. So, why does it feel good when we do get up and go?
This book covers a lot of the “this not that” aspects of exercise. By this we mean: ways that we can work with or against our bodies, for both physical and psychological fulfilment.
There’s an emphasis on such things as:
- movement without excessive exertion
- persistence being more important than power
- strength-building but only so far as is helpful to us
…and many other factors that you won’t generally see on your gym’s motivational posters
Bottom line: this book is for all those who have felt “exercise is not for me” but would also like the benefits of exercise. It turns out that there’s a best-of-both-worlds sweet spot!
Click here to check out Exercised and get working with your body rather than against it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Engage Your Whole Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
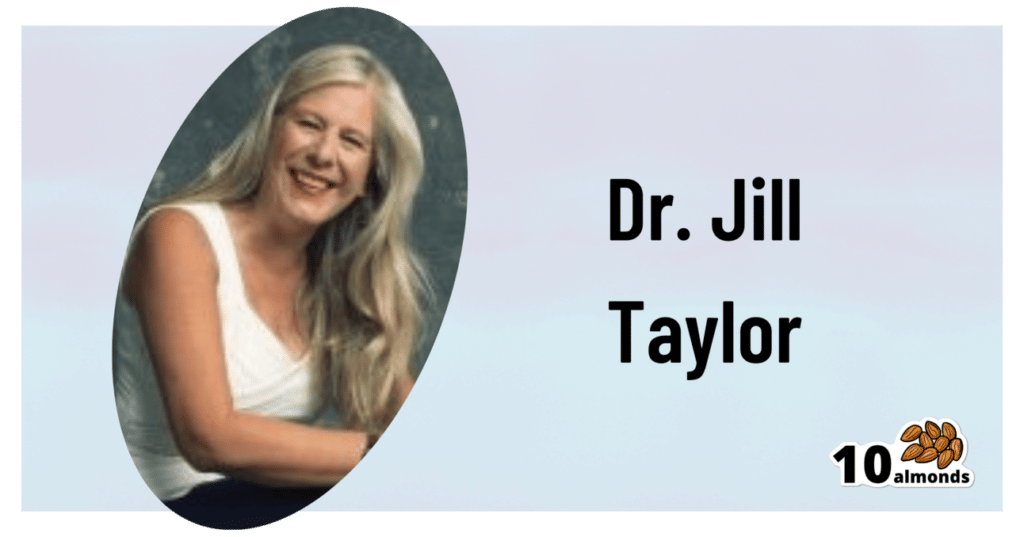
The Stroke Of Insight That Nobody Wants
This is Dr. Jill Bolte Taylor. She’s a neuroanatomist, who, at the age of 37 (when she was a post-doctoral fellow at Harvard Medical School), had what she refers to as her “stroke of insight”.
That is to say, she had a massive stroke, and after a major brain surgery to remove a clot the size of a golf ball, she spent the next 8 years re-learning to do everything.
Whereas previously she’d been busy mapping the brain to determine how cells communicate with each other, now she was busy mapping whether socks or shoes should go on first. Needless to say, she got an insight into neuroplasticity that few people would hope for.
What does she want us to know?
Dr. Taylor (now once again a successful scientist, lecturer, and author) advocates for “whole brain living”, which involves not taking parts of our brain for granted.
About those parts…
Dr. Taylor wants us to pay attention to all the parts regardless of size, ranging from the two hemispheres, all the way down to the billions of brain cells, and yet even further, to the “trillions of molecular geniuses”—because each brain cell is itself reliant on countless molecules of the many neurochemicals that make up our brain.
For a quick refresher on some of the key players in that latter category, see our Neurotransmitter Cheatsheet 😎
When it comes to the hemispheres, there has historically been a popular belief that these re divided into:
- The right brain: emotional, imaginative, creative, fluid feeling
- The left brain: intellectual, analytical, calculating, crystal thinking
…which is not true, anatomically speaking, because there are cells on both sides doing their part of both of these broad categories of brain processes.
However, Dr. Taylor found, while one hemisphere of her brain was much more damaged than the other, that nevertheless she could recover some functions more quickly than others, which, once she was able to resume her career, inspired her model of four distinct ways of cogitating that can be switched-between and played with or against each other:
Meet The Four Characters Inside Your Brain
Why this matters
As she was re-learning everything, the way forward was not quick or easy, and she also didn’t know where she was going, because for obvious reasons, she couldn’t remember, much less plan.
Looking backwards after her eventual full recovery, she noted a lot of things that she needed during that recovery, some of which she got and some of which she didn’t.
Most notably for her, she needed the right kind of support that would allow all four of the above “characters” as she puts it, to thrive and grow. And, when we say “grow” here we mean that literally, because of growing new brain cells to replace the lost ones (as well as the simple ongoing process of slowly replacing brain cells).
For more on growing new brain cells, by the way, see:
How To Grow New Brain Cells (At Any Age)
In order to achieve this in all of the required brain areas (i.e., and all of the required brain functions), she also wants us to know… drumroll please…
When to STFU
Specifically, the ability to silence parts of our brain that while useful in general, aren’t necessarily being useful right now. Since it’s very difficult to actively achieve a negative when it comes to brain-stuff (don’t think of an elephant), this means scheduling time for other parts of our brain to be louder. And that includes:
- scheduling time to feel (emotionally)
- scheduling time to feel (gut feelings)
- scheduling time to feel (kinesthetically)
…amongst others.
Note: those three are presented in that order, from least basic to most basic. And why? Because, clever beings that we are, we typically start from a position that’s not remotely basic, such as “overthinking”, for example. So, there’s a wind-down through thinking just the right amount, thinking through simpler concepts, feeling, noticing one’s feelings, noticing noticing one’s feelings, all the way down to what, kinesthetically, are we actually physically feeling.
❝It is interesting to note that although our limbic system fucntions throughout our lifetime, it does not mature. As a result, when our emotional “buttons” are pushed, we retain the ability to react to incoming stimulation as though we were a two-year-old, even when we are adults.❞
~ Dr. Jill Taylor
Of course, sometimes the above is not useful, which is why the ability to switch between brain modes is a very important and useful skill to develop.
And how do we do that? By practising. Which is something that it’s necessary to take up consciously, and pursue consistently. When children are at school, there are (hopefully, ideally) curricula set out to ensure they engage and train all parts of their brain. As adults, this does not tend to get the same amount of focus.
“Children’s brains are still developing”—indeed, and so are adult brains:
The Brain As A Work-In-Progress
Dr. Taylor had the uncommon experience of having to, in many ways, neurologically speaking, redo childhood. And having had a second run at it, she developed an appreciation of the process that most of us didn’t necessarily get when doing childhood just the once.
In other words: take the time to feel stuff; take the time to quiet down your chatty mind, take the time engage your senses, and take it seriously! Really notice, as though for the first time, what the texture of your carpet is like. Really notice, as though for the first time, what it feels like to swallow some water. Really notice, as though for the first time, what it feels like to experience joy—or sadness, or comfort, or anger, or peace. Exercise your imagination. Make some art (it doesn’t have to win awards; it just has to light up your brain!). Make music (again, it’s about wiring your brain in your body, not about outdoing Mozart in composition and/or performance). Make changes! Make your brain work in the ways it’s not in the habit of doing.
If you need a little help switching off parts of your brain that are being too active, so that you can better exercise other parts of your brain that might otherwise have been neglected, you might want to try:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: