Beet “Kvass” With Ginger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Kvass is a popular drink throughout Eastern Europe, with several countries claiming it, but the truth is, kvass is older than nations (as in: nations, in general, any of them; nation states are a newer concept than is often realized), and its first recorded appearance was in the city state of Kyiv.
This one is definitely not a traditional recipe, as kvass is usually made from rye, but keeping true to its Eastern European roots with (regionally popular) beetroot, it’s nevertheless a great fermented drink, full of probiotic benefits, and this time, with antioxidants too.
It’s a little saltier than most things we give recipes for here, so enjoy it on hot sunny days as a great way to replenish electrolytes!
You will need (for 1 quart / 1 liter)
- 2¾ cups filtered or spring water
- 2 beets, roughly chopped
- 1 tbsp chopped fresh ginger
- 2 tsp salt (do not omit or substitute)
Method
(we suggest you read everything at least once before doing anything)
1) Sterilize a 1-quart jar with boiling water (carefully please)
2) Put all the ingredients in the jar and stir until the salt dissolves
3) Close the lid tightly and store in a cool dark place to ferment for 2 weeks
4) Strain the beets and ginger (they are now pickled and can be enjoyed in a salad or as a kimchi-like snack), pouring the liquid into a clean jar/bottle. This can be kept in the fridge for up to a month. Next time you make it, if you use ¼ cup of this as a “starter” to replace an equal volume of water in the original recipe, the fermentation will take days instead of weeks.
5) Serve! Best served chilled, but without ice, on a hot sunny day.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- What To Eat, Take, And Do Before A Workout
- Ginger Does A Lot More Than You Think
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Elderly loss of energy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Please please give some information on elderly loss of energy and how it can be corrected. Please!❞
A lot of that is the metabolic slump described above! While we certainly wouldn’t describe 60 as elderly, and the health impacts from those changes at 45–55 get a gentler curve from 60 onwards… that curve is only going in one direction if we don’t take exceptionally good care of ourselves.
And of course, there’s also a degree of genetic lottery, and external factors we can’t entirely control (e.g. injuries etc).
One factor that gets overlooked a lot, though, is really easy to fix: B-vitamins.
In particular, vitamins B1, B5, B6, and B12. Of those, especially vitamins B1 and B12.
(Vitamins B5 and B6 are critical to health too, but relatively few people are deficient in those, while many are deficient in B1 and/or B12, especially as we get older)
Without going so detailed as to make this a main feature: these vitamins are essential for energy conversion from food, and they will make a big big difference.
You might especially want to consider taking sulbutiamine, which is a synthetic version of thiamin (vitamin B1), and instead of being water-soluble, it’s fat-soluble, and it easily crosses the blood-brain barrier, which is a big deal.
As ever, always check with your doctor because your needs/risks may be different. Also, there can be a lot of reasons for fatigue and you wouldn’t want to overlook something important.
You might also want to check out yesterday’s sponsor, as they offer personalized at-home health testing to check exactly this sort of thing.
❝What are natural ways to lose weight after 60? Taking into account bad knees or ankles, walking may be out as an exercise, running certainly is.❞
Losing weight is generally something that comes more from the kitchen than the gym, as most forms of exercise (except HIIT; see below) cause the metabolism to slow afterwards to compensate.
However, exercise is still very important, and swimming is a fine option if that’s available to you.
A word to the wise: people will often say “gentle activities, like tai chi or yoga”, and… These things are not the same.
Tai chi and yoga both focus on stability and suppleness, which are great, but:
- Yoga is based around mostly static self-support, often on the floor
- Tai chi will have you very often putting most of your weight on one slowly-increasingly bent knee at a time, and if you have bad knees, we’ll bet you winced while reading that.
So, maybe skip tai chi, or at least keep it to standing meditations and the like, not dynamic routines. Qigong, the same breathing exercises used in tai chi, is also an excellent way to improve your metabolism, by the way.
Ok, back onto HIIT:
You might like our previous article: How To Do HIIT* (Without Wrecking Your Body)
*High-Intensity Interval Training (the article also explains what this is and why you want to do it)
Share This Post
-
The Plant Power Doctor
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Prescription For GLOVES
This is Dr. Gemma Newman. She’s a GP (General Practitioner, British equivalent to what is called a family doctor in America), and she realized that she was treating a lot of patients while nobody was actually getting better.
So, she set out to help people actually get better… But how?
The biggest thing
The single biggest thing she recommends is a whole foods plant-based diet, as that’s a starting point for a lot of other things.
Click here for an assortment of short videos by her and other health professionals on this topic!
Specifically, she advocates to “love foods that love you back”, and make critical choices when deciding between ingredients.
Click here to see her recipes and tips (this writer is going to try out some of these!)
What’s this about GLOVES?
We recently reviewed her book “Get Well, Stay Well: The Six Healing Health Habits You Need To Know”, and now we’re going to talk about those six things in more words than we had room for previously.
They are six things that she says we should all try to get every day. It’s a lot simpler than a lot of checklists, and very worthwhile:
Gratitude
May seem like a wishy-washy one to start with, but there’s a lot of evidence for this making a big difference to health, largely on account of how it lowers stress and anxiety. See also:
How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
Love
This is about social connections, mostly. We are evolved to be a social species, and while some of us want/need more or less social interaction than others, generally speaking we thrive best in a community, with all the social support that comes with that. See also:
How To Beat Loneliness & Isolation
Outside
This is about fresh air and it’s about moving and it’s about seeing some green plants (and if available, blue sky), marvelling at the wonder of nature and benefiting in many ways. See also:
Vegetables
We spoke earlier about the whole foods plant-based diet for which she advocates, so this is that. While reducing/skipping meat etc is absolutely a thing, the focus here is on diversity of vegetables; it is best to make a game of seeing how many different ones you can include in a week (not just the same three!). See also:
Three Critical Kitchen Prescriptions
Exercise
At least 150 minutes moderate exercise per week, and some kind of resistance work. It can be calisthenics or something; it doesn’t have to be lifting weights if that’s not your thing! See also:
Resistance Is Useful! (Especially As We Get Older)
Sleep
Quality and quantity. Yes, 7–9 hours, yes, regardless of age. Unless you’re a child or a bodybuilder, in which case make it nearer 12. But for most of us, 7–9. See also:
Why You Probably Need More Sleep
Want to know more?
As well as the book we mentioned earlier, you might also like:
The Plant Power Doctor – by Dr. Gemma Newman
While the other book we mentioned is available for pre-order for Americans (it’s already released for the rest of the world), this one is available to all right now, so that’s a bonus too.
If books aren’t your thing (or even if they are), you might like her award-winning podcast:
Take care!
Share This Post
-
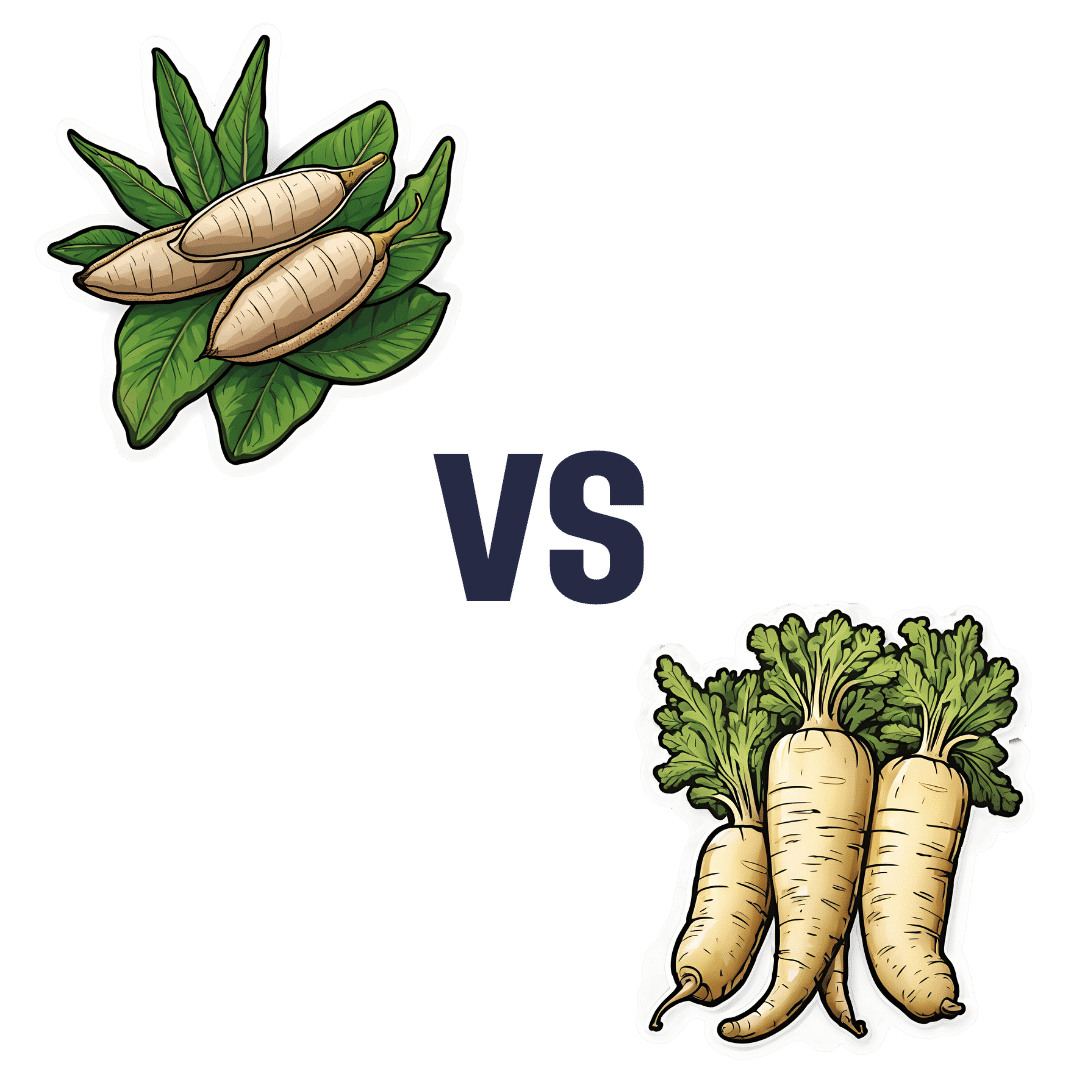
Cassava vs Parsnip – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cassava to parsnips, we picked the parsnips.
Why?
This one wasn’t close!
In terms of macros, cassava has more than 2x the carbs while parsnips have nearly 3x the fiber, making for a very clear win for parsnips.
In the category of vitamins, cassava has more of vitamins B3 and C, while parsnips have more of vitamins B1, B2, B5, B6, B9, E, and K, with very large margins of difference in the latter two cases. Another overwhelming win for parsnips.
Looking at minerals, cassava is not higher in any minerals, while parsnips have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc; a very one-sided win for parsnips!
So, by all means enjoy either or both (diversity is good), but there’s a clear winner here today, and it’s parsnips.
Want to learn more?
You might like:
What Do The Different Kinds Of Fiber Do? 30 Foods That Rank Highest
Enjoy!
Share This Post
Related Posts
-
Rutin For Your Circulation & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
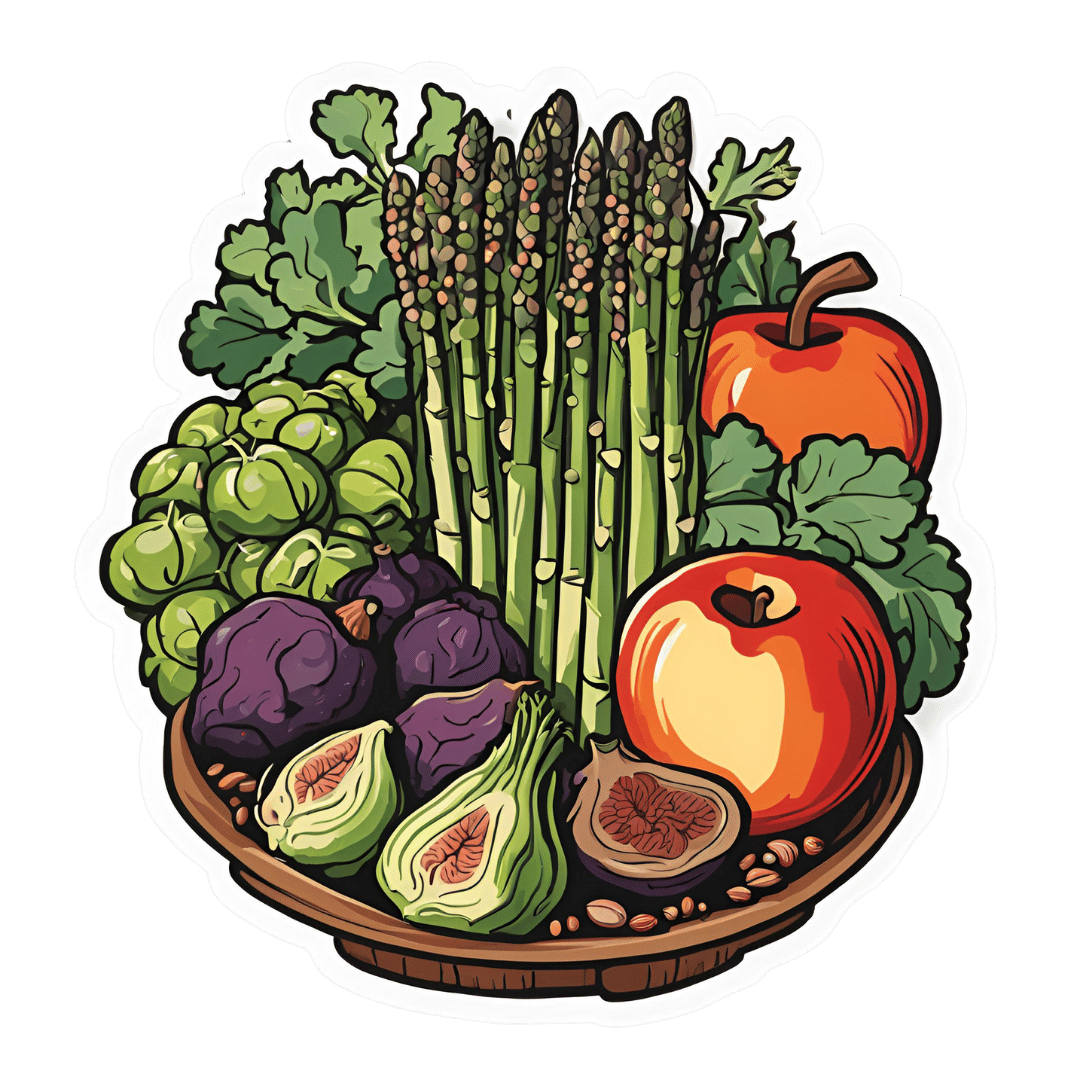
Rutin is a bioflavonoid so potent it’s also been called “vitamin P”, and it’s found most abundantly in buckwheat, as well appearing in citrus and some stone fruits (apricots, plums, etc) as well as figs and apples—it’s also found in asparagus, and green and black tea.
So, what does it do?
Quite a lot: The Pharmacological Potential of Rutin
There’s much more there than we have room to cover here, but we’ll pick out a few salient properties to focus on.
First, a word of warning
A lot of the extant science for rutin is in non-human animals. Sometimes, what works for non-human animals doesn’t work for humans; we saw a clear example of this here:
Conjugated Linoleic Acid For Weight Loss?
…in which CLA worked for weight loss in mice, hamsters, chickens, and pigs, but stubbornly not humans.
The state of affairs with the science for rutin isn’t nearly that bad and there are human studies showing efficacy, and indeed, rutin is given to (human) patients with capillary fragility, varicose veins, bruising, or hemorrhoids, for example:
So, we’ll try to give you humans-only sources so far as we can today!
Improving blood flow
Rutin does improve various blood metrics, including various kinds of blood pressure (diastolic, systolic, mean arterial, pulse) and heart rate. At least, it did in humans with type 2 diabetes, and we may reasonably assume these results may be extrapolated to humans without type 2 (or any other) diabetes:
As you may gather from the title, it did also significantly improve serum antioxidant levels, and quality of life (which latter was categorized as: emotional limitations, energy and freshness, mental health, social performance, and general health).
We couldn’t find studies for cardioprotective effects in humans (and of course those couldn’t be RCTs, they’d have to be observational studies, because no ethics board allows inducing heart attacks in humans for the sake of science), but here’s a study using rats (with and without diabetes), showing proof of principle at least:
Anti-Alzheimer’s potential
As ever, a good general rule of thumb is “what’s good for the blood is good for the brain”, and that’s true in this case too.
The title says it all, here:
In case that is not clear: everything in that title after the word “inhibits” is bad for the brain and is implicated in Alzheimer’s disease pathogenesis and progression; in other words, rutin is good against all those bad, Alzheimer’s-favoring things.
Other neuroprotective activity
You may remember from the above-linked research that it helps protect against damage caused by Advanced Glycation End-products (AGEs) (the golden-brown stuff that appears as a result of dry-cooking proteins and fats); it also helps against damage caused by acrylamide (the golden-brown stuff that appears as a result of dry-cooking starches).
Note: in both cases “dry-cooking” includes cooking with oil; it simply means “without water”.
Again, this was a rat study, because no ethics board would have let the researchers fry human brains for science.
Want to try some?
As well as simply enjoying the fruits and vegetables that contain it, it is possible to take a rutin supplement.
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healing Cracked Fingers
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Question. Suffer from cracked (split) finger tips in the cold weather. Very painful, is there something I can take to ward off this off. Appreciate your daily email.❞
Ouch, painful indeed! Aside from good hydration (which is something we easily forget in cold weather), there’s no known internal guard against this*, but from the outside, oil-based moisturizers are the way to go.
Olive oil, coconut oil, jojoba oil, and shea butter are all fine options.
If the skin is broken such that infection is possible, then starting with an antiseptic ointment/cream is sensible. A good example product is Savlon, unless you are allergic to its active ingredient chlorhexidine.
*However, if perchance you are also suffering from peripheral neuropathy (a common comorbidity of cracked skin in the extremities), then lion’s main mushroom can help with that.
Writer’s anecdote: I myself started suffering from peripheral neuropathy in my hands earlier this year, doubtlessly due to some old injuries of mine.
However, upon researching for the above articles, I was inspired to try lion’s mane mushroom for myself. I take it daily, and have now been free of symptoms of peripheral neuropathy for several months.
Here’s an example product on Amazon, by the way
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
3 Appetite Suppressants Better Than Ozempic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Annette Bosworth gives her recommendations, and explains why:
What and how
We’ll get straight to it; the recommendations are:
- Coffee, black, unsweetened: not only suppresses the appetite but also boosts the metabolism, increasing fat burn.
- Salt: especially for when fasting (as under such circumstances we may lose salts without replenishing them), a small taste of this can help satisfy taste buds while replenishing sodium and—depending on the salt—other minerals. For example, if you buy “low-sodium salt” in the supermarket, this is generally sodium chloride cut with potassium chloride and/or occasionally magnesium sulfate.
- Ketones (MCT oil): ketones can suppress hunger, particularly when fasting causes blood sugar levels to drop. Supplementing with MCT oil promotes ketone production in the liver, training the body to produce more ketones naturally, thus curbing appetite.
For more on these including the science of them, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Ozempic vs Five Natural Supplements
- Some Surprising Truths About Hunger And Satiety
- The Fruit That Can Specifically Reduce Belly Fat
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: