The Bare-Bones Truth About Osteoporosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
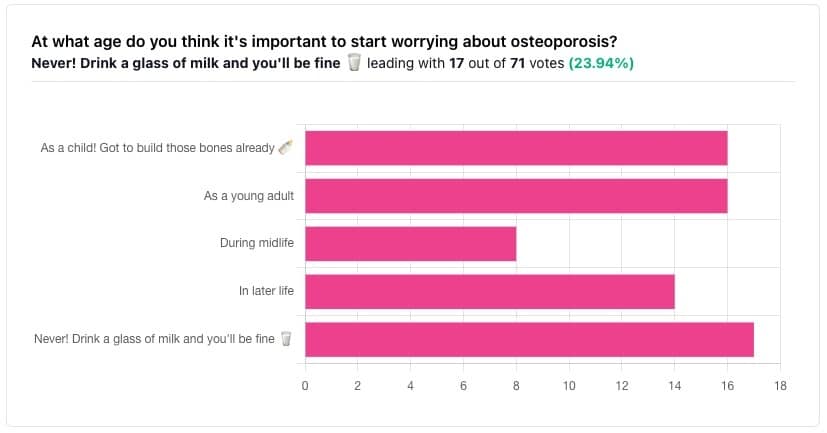
In yesterday’s issue of 10almonds, we asked you “at what age do you think it’s important to start worrying about osteoporosis?”, and here’s the spread of answers you gave us:
The Bare-bones Truth About Osteoporosis
In yesterday’s issue of 10almonds, we asked you “at what age do you think it’s important to start worrying about osteoporosis?”, and here’s the spread of answers you gave us:
At first glance it may seem shocking that a majority of respondents to a poll in a health-focused newsletter think it’ll never be an issue worth worrying about, but in fact this is partly a statistical quirk, because the vote of the strongest “early prevention” crowd was divided between “as a child” and “as a young adult”.
This poll also gave you the option to add a comment with your vote. Many subscribers chose to do so, explaining your choices… But, interestingly, not one single person who voted for “never” had any additional thoughts to add.
We loved reading your replies, by the way, and wish we had room to include them here, because they were very interesting and thought-provoking.
Let’s get to the myths and facts:
Top myth: “you will never need to worry about it; drink a glass of milk and you’ll be fine!”
The body is constantly repairing itself. Its ability to do that declines with age. Until about 35 on average, we can replace bone mineral as quickly as it is lost. After that, we lose it by up to 1% per year, and that rate climbs after 50, and climbs even more steeply for those who go through (untreated) menopause.
Losing 1% per year might not seem like a lot, but if you want to live to 100, there are some unfortunate implications!
About that menopause, by the way… Because declining estrogen levels late in life contribute significantly to osteoporosis, hormone replacement therapy (HRT) may be of value to many for the sake of bone health, never mind the more obvious and commonly-sought benefits.
On the topic of that glass of milk…
- Milk is a great source of calcium, which is useless to the body if you don’t also have good levels of vitamin D and magnesium.
- People’s vitamin D levels tend to directly correlate to the level of sun where they live, if supplementation isn’t undertaken.
- Plant-based milks are usually fortified with vitamin D (and calcium), by the way.
- Most people are deficient in magnesium, because green leafy things don’t form as big a part of most people’s diets as they should.
See also: An update on magnesium and bone health
Next most common myth: “bone health is all about calcium”
We spoke a little above about the importance of vitamin D and magnesium for being able to properly use that. But potassium is also critical:
Read more: The effects of potassium on bone health
While we’re on the topic…
People think of collagen as being for skin health. And it is important for that, but collagen’s benefits (and the negative effects of its absence) go much deeper, to include bone health. We’ve written about this before, so rather than take more space today, we’ll just drop the link:
We Are Such Stuff As Fish Are Made Of
Want to really maximize your bone health?
You might want to check out this well-sourced LiveStrong article:
Bone Health: Best and Worst Foods
(Teaser: leafy greens are in 2nd place, topped by sardines at #1—where do you think milk ranks?)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Toasted Chick’n Mango Tacos
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tacos aren’t generally held up as the world’s healthiest food, but they can be! There’s so much going on in this dish today, healthwise, in a good way, that it’s hard to know where to start. But suffice it to say, these tacos are great for your gut, heart, blood sugars, and more.
You will need
For the chickpeas:
- 1 can chickpeas, drained
- 1 tbsp ras el-hanout*
- 1 tsp red pepper flakes
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
*You can easily make this yourself; following our recipe (linked above in the ingredients list) will be better than buying it ready-made, and if you have strong feelings about any of the ingredients, you can adjust per your preference.
For the tahini sauce:
- ⅓ cup tahini
- 2 tbsp apple cider vinegar
- 2 tbsp finely chopped fresh dill
- ¼ bulb garlic, minced
- 1 tsp red pepper flakes
- ½ tsp black pepper, coarse ground
It may seem like salt is conspicuous by its absence, but there is already enough in the chickpeas component; you do not want to overwhelm the dish. Trust us that enjoying these things together will be well-balanced and delicious as written.
For the mango relish:
- ½ mango, pitted, peeled, and cubed
- 2 tsp apple cider vinegar
- 2 tsp cilantro, finely chopped (substitute with parsley if you have the “cilantro tastes like soap” gene)
- 1 tsp red pepper flakes
For building the taco:
- Soft corn tortillas
- Handful of arugula
- 1 avocado, pitted, peeled, and sliced
- ½ red onion, sliced
Method
(we suggest you read everything at least once before doing anything)
1) Heat a sauté pan with a little olive oil in; add the chickpeas and then the rest of the ingredients from the chickpea section; cook for about 5 minutes, stirring frequently, and set aside.
2) Combine the tahini sauce ingredients in a small bowl, stirring in ¼ cup water, and set aside.
3) Combine the mango relish ingredients in a separate small bowl, and set aside. You can eat the other half of the mango if you like.
4) Lightly toast the tortillas in a dry skillet, or using a grill.
5) Assemble the tacos; we recommend the order: tortillas, arugula, avocado slices, chickpeas, mango relish, red onion slices, tahini sauce.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat More (Of This) For Lower Blood Pressure
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we hit all five today! Yay!
- An Apple (Cider Vinegar) A Day…
- Coconut vs Avocado – Which is Healthier?
- Lettuce vs Arugula – Which is Healthier?
Take care!
Share This Post
-
The Lifestyle Factors That Matter >8 Times More Than Genes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve said before that “genes predispose; they don’t predetermine”. It can be good to know one’s genes, of course, and we’ve written about this here:
Genetic Testing: Health Benefits & Methods
…which can include some quite contemporary risks, such as:
Genetic Risk Factors For Long COVID
And yet…
Nurture Over Nature
A very large (n=492,567) study looked into the impact of 25 lifestyle/environmental factors, of which 23 are considered modifiable, and found that lifestyle/environmental factors accounted for 17% of the variation in mortality risk, while genetic predisposition accounted for less than 2%.
Which is good news, because it means we can improve our lot.
But how?
The strongest negative factors (that increased mortality the most) were:
- Smoking
- Not owning your home (interestingly, “live in accommodation rent-free vs own” performed just as badly as various kinds of “renting home vs own”, while “own house with mortgage, vs own outright” had only a marginal negative effect)
- Sleeping more than 9 hours per day (performed even worse than sleeping under 7 hours per day, which also increased mortality risk, but not by as much as oversleeping)
- Financial difficulties in the past two years
- Homosexuality
- Unemployment
- Being an evening person
- Lonely lifestyle
- Frequent napping
We may hypothesize that homosexuality probably makes the list because of how it makes one more likely to have other items on the list, especially unemployment, and the various poverty-related indicators that come from unemployment.
Being an evening person, whatever its pathology, is a well-established risk factor that we’ve talked about before:
Early Bird Or Night Owl? Genes vs Environment ← this is also, by the way, an excellent example of how “genes predispose; they don’t predetermine”, because there is a genetic factor involved, and/but we absolutely can switch it up, if we go about it correctly, and become a morning person without trying to force it.
The strongest positive factors (that decreased mortality the most) were:
- The inverse of all of the various above things, e.g. never having smoked, owning your own home, etc
- Household income, specifically
- Living with a partner
- Having oil central heating
- Gym use
- Sun protection use
- Physical activity, especially if in leisure time rather than as part of one’s work
- Glucosamine supplements
- Family visit frequency
- Cereal fiber intake (i.e. whole grains)
We may hypothesize that having oil central heating is simply a more expensive option to install than many, and therefore likely one enjoyed by homeowners more often than renters.
We may hypothesize that glucosamine supplementation is an indication of the type of person who takes care of a specific condition (inflammation of the joints) without an existential threat; notably, multivitamin supplements don’t get the same benefit, probably because of their ubiquity.
We may hypothesize that “family visit frequency” is highly correlated to having a support network, being social (and thus not lonely), and likely is associated with household income too.
You can see the full list of factors and their impacts, here:
Environmental architecture of mortality in the UKB ← that’s the UK Biobank
You can read the paper in full, here:
Integrating the environmental and genetic architectures of aging and mortality
Practical takeaways
The priorities seem to be as follows:
Don’t smoke. Ideally you will never have smoked, but short of a time machine, you can’t change that now, so: what you can do is quit now if you haven’t already.
See also: Which Addiction-Quitting Methods Work Best?
Note that other factors often lumped in with such, for example daily alcohol consumption, red meat intake, processed meat intake, and salt intake, all significantly increased mortality risk, but none of them in the same league of badness as smoking.
See also: Is Sugar The New Smoking? ← simply put: no, it is not. Don’t get us wrong; added sugar is woeful for the health, but smoking is pretty much the worst thing you can do for your health, short of intentionally (and successfully) committing suicide.
Be financially secure, ideally owning your own home. For many (indeed, for most people in the world) this may be an “easier said than done” thing, but if you can make decisions that will improve your financial security, the mortality numbers are very clear on this matter.
Be social, as loneliness indeed kills, in numerous ways. Loneliness means a lack of a support network, and it means a lack of social contact (thus increased risk of cognitive decline), and likely decreased ikigai, unless your life’s purpose is something inherently linked to solitude (e.g. the “meditating on top of a mountain” archetype).
See also: What Loneliness Does To Your Brain And Body
And to fix it: How To Beat Loneliness & Isolation
Be active: especially in your leisure time; being active because you have to does convey benefits, but on the same level as physical activity because you want to.
See also: No-Exercise Exercises (That Won’t Feel Like “Having To Do” Exercise)
Use sunscreen: we’re surprised this one made the list; it’s important to avoid skin cancer of course, but we didn’t think it’d be quite such a driver of mortality risk mitigation as the numbers show it is, and we can’t think of a clear alternative explanation, as we could with some of the other “why did this make the list?” items. At worst, it could be a similar case to that of glucosamine use, and thus is a marker of a conscientious person making a regular sustained effort for their health. Either way, it seems like a good idea based on the numbers.
See also: Do We Need Sunscreen In Winter, Really?
Enjoy whole grains: fiber is super-important, and that mustn’t be underestimated!
See also: What Matters Most For Your Heart? ← hint: it isn’t about salt intake or fat
And, for that matter: The Best Kind Of Fiber For Overall Health?
Take care!
Share This Post
-
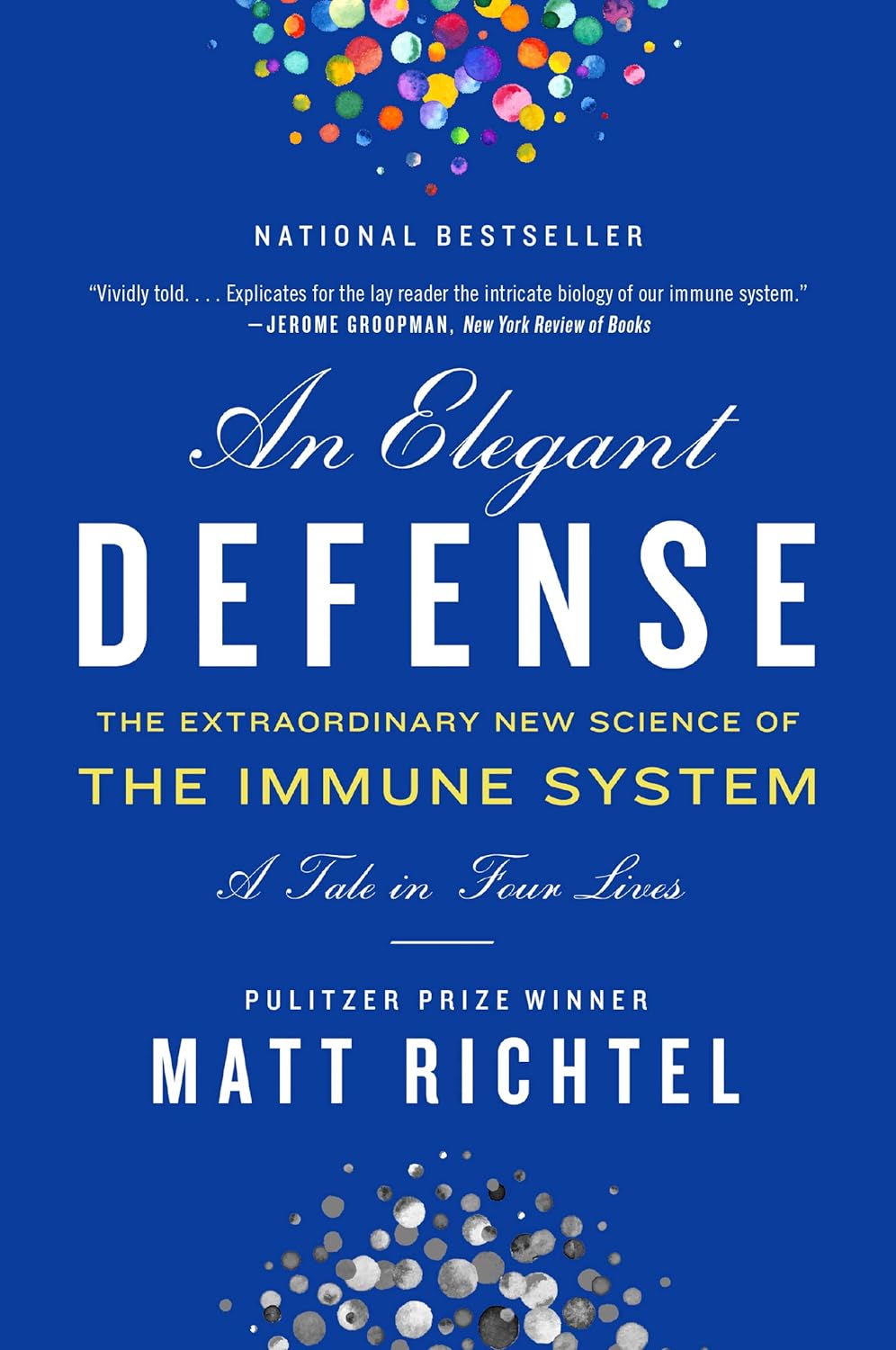
An Elegant Defense – by Matt Richtel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a way, Richtel got the best and worst of the publication date lottery. This book, which he’d obviously been working on for however long, was published in March 2020. Yes, that March 2020. So, it obviously got a huge boost in sales that launced it to bestseller status, and/but it doesn’t actually discuss COVID at all.
What it does discuss, is—as one might expect—the immune system. Or really, the immune systems, plural, several systems working alongside each other. How we got to have such, how our immune functions work, where all the various immune cells come from and what part they play. What pathogens can do to fight and/or confuse (or even co-opt) our immune response, and what modern medicine can do to counteract the pathogens’ anti-countermeasure countermeasures. And how it can still go wrong.
The “Four Lives” promised in the subtitle are stories, and Richtel explains the immune system through specific people’s specific battles. In particular, a friend of his who had quite a remarkable battle against cancer, which was of course terrible for him, but illustrative for us.
The style of the book is very readably journalistic. The author is a Pulitzer-winning NYT journalist, and not normally a science writer. Here at 10almonds, “we like big bibliographies and we cannot lie”, and we didn’t get to enjoy that in this case. The book contained no bibliography (nor appropriate inline citations, nor equivalent footnotes). Maybe a future addition will include this.
Bottom line: there’s a lot of “science for the lay reader” here. While the lack of references is a big oversight, the book does give a very good overview of what both sides (immune response and pathogenic invasion) bring to the battle of your body.
Click here to check out Elegant Defense, and demystify immunology!
Share This Post
Related Posts
-
Surgery won’t fix my chronic back pain, so what will?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This week’s ABC Four Corners episode Pain Factory highlighted that our health system is failing Australians with chronic pain. Patients are receiving costly, ineffective and risky care instead of effective, low-risk treatments for chronic pain.
The challenge is considering how we might reimagine health-care delivery so the effective and safe treatments for chronic pain are available to millions of Australians who suffer from chronic pain.
One in five Australians aged 45 and over have chronic pain (pain lasting three or more months). This costs an estimated A$139 billion a year, including $12 billion in direct health-care costs.
The most common complaint among people with chronic pain is low back pain. So what treatments do – and don’t – work?
Opioids and invasive procedures
Treatments offered to people with chronic pain include strong pain medicines such as opioids and invasive procedures such as spinal cord stimulators or spinal fusion surgery. Unfortunately, these treatments have little if any benefit and are associated with a risk of significant harm.
Spinal fusion surgery and spinal cord stimulators are also extremely costly procedures, costing tens of thousands of dollars each to the health system as well as incurring costs to the individual.
Addressing the contributors to pain
Recommendations from the latest Australian and World Health Organization clinical guidelines for low back pain focus on alternatives to drug and surgical treatments such as:
- education
- advice
- structured exercise programs
- physical, psychological or multidisciplinary interventions that address the physical or psychological contributors to ongoing pain.
Pain education is central. Monkey Business Images/Shutterstock Two recent Australian trials support these recommendations and have found that interventions that address each person’s physical and psychological contributors to pain produce large and sustained improvements in pain and function in people with chronic low back pain.
The interventions have minimal side effects and are cost-effective.
In the RESOLVE trial, the intervention consists of pain education and graded sensory and movement “retraining” aimed to help people understand that it’s safe to move.
In the RESTORE trial, the intervention (cognitive functional therapy) involves assisting the person to understand the range of physical and psychological contributing factors related to their condition. It guides patients to relearn how to move and to build confidence in their back, without over-protecting it.
Why isn’t everyone with chronic pain getting this care?
While these trials provide new hope for people with chronic low back pain, and effective alternatives to spinal surgery and opioids, a barrier for implementation is the out-of-pocket costs. The interventions take up to 12 sessions, lasting up to 26 weeks. One physiotherapy session can cost $90–$150.
In contrast, Medicare provides rebates for just five allied health visits (such as physiotherapists or exercise physiologists) for eligible patients per year, to be used for all chronic conditions.
Private health insurers also limit access to reimbursement for these services by typically only covering a proportion of the cost and providing a cap on annual benefits. So even those with private health insurance would usually have substantial out-of-pocket costs.
Access to trained clinicians is another barrier. This problem is particularly evident in regional and rural Australia, where access to allied health services, pain specialists and multidisciplinary pain clinics is limited.
Higher costs and lack of access are associated with the increased use of available and subsidised treatments, such as pain medicines, even if they are ineffective and harmful. The rate of opioid use, for example, is higher in regional Australia and in areas of socioeconomic disadvantage than metropolitan centres and affluent areas.
So what can we do about it?
We need to reform Australia’s health system, private and public, to improve access to effective treatments for chronic pain, while removing access to ineffective, costly and high-risk treatments.
Better training of the clinical workforce, and using technology such as telehealth and artificial intelligence to train clinicians or deliver treatment may also improve access to effective treatments. A recent Australian trial, for example, found telehealth delivered via video conferencing was as effective as in-person physiotherapy consultations for improving pain and function in people with chronic knee pain.
Advocacy and improving the public’s understanding of effective treatments for chronic pain may also be helpful. Our hope is that coordinated efforts will promote the uptake of effective treatments and improve the care of patients with chronic pain.
Christine Lin, Professor, University of Sydney; Christopher Maher, Professor, Sydney School of Public Health, University of Sydney; Fiona Blyth, Professor, University of Sydney; James Mcauley, Professor of Psychology, UNSW Sydney, and Mark Hancock, Professor of Physiotherapy, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Podiatrists Debunk 11 Feet Myths
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Podiatrists Dr. Sarah Haller and Dr. Brad Schaeffer put us on a better path:
Don’t get wrong-footed
We’ll not keep the 11 myths a mystery; they are…
- “You have warts because your feet are dirty.”
False! Warts are caused by a virus, not dirt. Viruses can be picked up from surfaces like yoga mats, pools, gyms, and showers. - “Bunions are caused by wearing heels.”
False! Bunions are genetic deformities where the bone behind the big toe shifts. Heels might worsen them but don’t cause them. - “Cutting the sides of my toenail will prevent an ingrown toenail.”
False! Toenails should be cut straight across. Cutting the sides can make ingrown toenails worse. - “Pedicures gave me toenail fungus.”
Partially true! You can get fungus from many places, but safe, sterile pedicures are generally fine. - “Only athletes get athlete’s foot.”
False! Athlete’s foot is a fungal infection caused by warm, moist environments. Anyone can get it, not just athletes. - “My feet are fine because I trained them to walk in stilettos.”
False! You can get used to stilettos, but they aren’t healthy long-term. They shorten the Achilles tendon and put pressure on the foot. - “You can’t do anything for a broken toe.”
False! Broken toes can be treated and should be checked by a doctor. They may need to be set for proper healing. - “It’s normal for your feet to hurt from standing all day.”
False! Foot pain isn’t normal and can be prevented with proper footwear, support, and compression socks. - “All inserts are the same.”
False! Everyone’s feet are different. Some may benefit from over-the-counter insoles, but others need custom orthotics. - “Sprained ankles are no big deal.”
False! Sprains can damage ligaments and lead to instability or arthritis if untreated. Proper stabilization is essential. - “If I can walk after an injury, I don’t need to see a doctor.”
False! You can still have serious injuries like fractures even if you can walk. Always get checked after an injury.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Steps For Keeping Your Feet A Healthy Foundation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- “You have warts because your feet are dirty.”
-
How an Idaho vaccine advocacy org plans its annual goals
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The start of a new year means many nonprofits and community health workers are busy setting goals and reflecting on what’s worked and what hasn’t. For those engaged in vaccine outreach, it also means reflecting on the tools and tactics that help them communicate better with their communities about why vaccines matter.
Across the country, childhood vaccination rates have declined since the COVID-19 pandemic, resulting in a resurgence of preventable diseases like pertussis.
Also known as whooping cough, pertussis has surged in states like Idaho, said Karen Jachimowski Sharpnack, executive director of the Idaho Immunization Coalition, in a conversation with PGN about the organization’s 2025 priorities.
Sharpnack shared how spikes in infectious respiratory illnesses can create opportunities to listen better and understand the nuances of the communities they serve.
Here’s more of what Sharpnack said.
[Editor’s note: The contents of this interview have been edited for length and clarity.]
PGN: Whooping cough cases are up in your state. Can you share an example of how your organization is responding?
Karen Jachimowski Sharpnack: If you look at Treasure Valley and Northern Idaho, the majority of those cases have been reported, and it’s like five times as much as we had the previous year.
So, two things that the Coalition is doing in response: First, we put out radio public service announcements throughout those particular areas about what whooping cough is, how contagious it is, and what you should do if you think your child or anyone you know has it.
Second, we are contacting every school superintendent, principal, school nurse, with a letter from us at the Coalition [to warn about] the whooping cough outbreaks in schools right now. Here’s what the symptoms are, here’s what you can do, and then here’s how you can protect yourself and your families.
It doesn’t mean the health district wouldn’t do it, or the Department of Health and Welfare can’t do it. But from our standpoint, at least we are bringing an awareness to the schools that this is happening.
PGN: How does your organization decide when outreach is needed? How do you take a pulse of your communities’ vaccine attitudes?
K.J.S.: We consistently hold listening sessions. We do them in English and Spanish if we need to, and we go around—and I’m talking about the southern part of the state—and bring people together.
We’ve done adults, we’ve done teenagers, we’ve done college students, we’ve done seniors, we’ve done all age groups.
So, we’ll bring eight or 10 people together, and we’ll spend a couple of hours with them. We feed them and we also pay them to be there. We say, ‘We want to hear from you about what you’re hearing about vaccines, what your views are if you’re vaccinated.’ Anytime, by the way, they can get up and leave and still get paid.
We want to hear what they’re hearing on the ground. And these sessions are extremely informational. For one, we learn about the misinformation that goes out there, like immediately. And two, we’re able to then focus [on how to respond]. If we’re hearing this, what kind of media campaign do we need to get together?
PGN: How do these listening sessions inform your work?
K.J.S.: So, a couple times a year we also pay a professional poller to do a poll. And when we get those results we check them against our listening sessions. We want to see: Are we on target? Are we ahead?
We just finished putting a one-pager together for legislators, so we’re ready to go with the new [legislative] session. We do this poll every year in August-September to know how Idahoans are feeling about vaccines. We get the results in October, because we’re getting ready for the next year.
We actually poll 19-to-64-year-olds, really honing in on questions like, ‘Do you believe vaccines are safe and effective?’ ‘Do you believe that school vaccination rules should still be in place?’
And what’s pretty cool is that two-thirds of Idahoans still believe vaccines are safe and effective, want to keep school rules in place, and believe that the infrastructure systems that we have in place for our vaccine registry should remain the same. Those are important to hear, so this is really good information that we can pull out and do something with.
PGN: Like what?
K.J.S.: Here’s the bottom line. It takes money to do this work, so you have to be able to say what you are going to do with the results.
Doing a poll costs anywhere from $15,000 to $35,000. This is an expensive investment, but we know that the polling is so important to us, along with the time that I have my staff go out and do the listening sessions and get feedback.
We take those results to educate, to talk to our legislators, and advocate for vaccines. We actually do these high-level media campaigns around the state. So, we are actually doing something with the polling. We’re not just sharing the results out.
And then we actually ask, what can we do to make a change? What are we hearing that we need to focus on?
That’s why it’s really important, because we are actually pushing this out for 2025. We know where we’re going in 2025 programmatically with marketing, and we know where we’re going with advocacy work.
We’re not guessing. We’re actually listening to people. And then we’re making really concrete decisions on how we’re going to move the organization forward to be able to help our communities.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: