Natto, Taurine + Black Pepper, And Other Game-Changers
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Loved the info on nuts; of course I always eat pecans, which didn’t make the list of healthy nuts!❞
Dear subscriber, pardon the paraphrase of your comment—somehow it got deleted and now exists only in this writer’s memory. However, to address it:
Pecans are great too! We can’t include everything in every article (indeed, we got another feedback the same day saying the article was too long), but we love when you come to us with stuff for us to look at and write about (seriously, writer here: the more you ask, the easier it makes my job), so let’s talk pecans for a moment:
Pecans would have been number six on our list if we’d have written more!
Like many nuts, they’ve an abundance of healthy fats, fiber, vitamins, and minerals.
They’re particularly good for zinc, which is vital for immune function, healing (including normal recovery after normal exercise), and DNA synthesis (so: anti-aging).
Pecans are also great for reducing LDL (“bad” cholesterol) and triglycerides (which are also bad for heart health); check it out:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Stress-Proof Brain – by Dr. Melanie Greenberg
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The premise of the book is as stated in the subtitle: using mindfulness and neuroplasticity to manage our stress response.
As such, it’s divided into three parts:
- Understanding your stress (and different types of stressors)
- Calming your amygdalae (thus, dealing with your stress response while the stressor is stressing you)
- Moving forward with your prefrontal cortex (and thus, gradually improving automatic stress responses over time, as we learn new, better responses to do automatically)
The content ranges from the neurophysiological to “therapist’s couch” stuff; Dr. Greenberg having her PhD in psychology has prepared her to write both of those different-but-touching fields with equal competence. In-line citations are given throughout, for those who want to look up studies.
The style is direct and informative, with little to no attention given to making it an entertaining read. As a result, it’s information dense (which is good), and/but not necessarily a “couldn’t put it down” page-turner.
Bottom line: if you’d like to improve your ability to deal with stress, this book is as good as any.
Click here to check out The Stress-Proof Brain, and stress-proof yours!
Share This Post
-
Do We Simply Not Care About Old People?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The covid-19 pandemic would be a wake-up call for America, advocates for the elderly predicted: incontrovertible proof that the nation wasn’t doing enough to care for vulnerable older adults.
The death toll was shocking, as were reports of chaos in nursing homes and seniors suffering from isolation, depression, untreated illness, and neglect. Around 900,000 older adults have died of covid-19 to date, accounting for 3 of every 4 Americans who have perished in the pandemic.
But decisive actions that advocates had hoped for haven’t materialized. Today, most people — and government officials — appear to accept covid as a part of ordinary life. Many seniors at high risk aren’t getting antiviral therapies for covid, and most older adults in nursing homes aren’t getting updated vaccines. Efforts to strengthen care quality in nursing homes and assisted living centers have stalled amid debate over costs and the availability of staff. And only a small percentage of people are masking or taking other precautions in public despite a new wave of covid, flu, and respiratory syncytial virus infections hospitalizing and killing seniors.
In the last week of 2023 and the first two weeks of 2024 alone, 4,810 people 65 and older lost their lives to covid — a group that would fill more than 10 large airliners — according to data provided by the CDC. But the alarm that would attend plane crashes is notably absent. (During the same period, the flu killed an additional 1,201 seniors, and RSV killed 126.)
“It boggles my mind that there isn’t more outrage,” said Alice Bonner, 66, senior adviser for aging at the Institute for Healthcare Improvement. “I’m at the point where I want to say, ‘What the heck? Why aren’t people responding and doing more for older adults?’”
It’s a good question. Do we simply not care?
I put this big-picture question, which rarely gets asked amid debates over budgets and policies, to health care professionals, researchers, and policymakers who are older themselves and have spent many years working in the aging field. Here are some of their responses.
The pandemic made things worse. Prejudice against older adults is nothing new, but “it feels more intense, more hostile” now than previously, said Karl Pillemer, 69, a professor of psychology and gerontology at Cornell University.
“I think the pandemic helped reinforce images of older people as sick, frail, and isolated — as people who aren’t like the rest of us,” he said. “And human nature being what it is, we tend to like people who are similar to us and be less well disposed to ‘the others.’”
“A lot of us felt isolated and threatened during the pandemic. It made us sit there and think, ‘What I really care about is protecting myself, my wife, my brother, my kids, and screw everybody else,’” said W. Andrew Achenbaum, 76, the author of nine books on aging and a professor emeritus at Texas Medical Center in Houston.
In an environment of “us against them,” where everybody wants to blame somebody, Achenbaum continued, “who’s expendable? Older people who aren’t seen as productive, who consume resources believed to be in short supply. It’s really hard to give old people their due when you’re terrified about your own existence.”
Although covid continues to circulate, disproportionately affecting older adults, “people now think the crisis is over, and we have a deep desire to return to normal,” said Edwin Walker, 67, who leads the Administration on Aging at the Department of Health and Human Services. He spoke as an individual, not a government representative.
The upshot is “we didn’t learn the lessons we should have,” and the ageism that surfaced during the pandemic hasn’t abated, he observed.
Ageism is pervasive. “Everyone loves their own parents. But as a society, we don’t value older adults or the people who care for them,” said Robert Kramer, 74, co-founder and strategic adviser at the National Investment Center for Seniors Housing & Care.
Kramer thinks boomers are reaping what they have sown. “We have chased youth and glorified youth. When you spend billions of dollars trying to stay young, look young, act young, you build in an automatic fear and prejudice of the opposite.”
Combine the fear of diminishment, decline, and death that can accompany growing older with the trauma and fear that arose during the pandemic, and “I think covid has pushed us back in whatever progress we were making in addressing the needs of our rapidly aging society. It has further stigmatized aging,” said John Rowe, 79, professor of health policy and aging at Columbia University’s Mailman School of Public Health.
“The message to older adults is: ‘Your time has passed, give up your seat at the table, stop consuming resources, fall in line,’” said Anne Montgomery, 65, a health policy expert at the National Committee to Preserve Social Security and Medicare. She believes, however, that baby boomers can “rewrite and flip that script if we want to and if we work to change systems that embody the values of a deeply ageist society.”
Integration, not separation, is needed. The best way to overcome stigma is “to get to know the people you are stigmatizing,” said G. Allen Power, 70, a geriatrician and the chair in aging and dementia innovation at the Schlegel-University of Waterloo Research Institute for Aging in Canada. “But we separate ourselves from older people so we don’t have to think about our own aging and our own mortality.”
The solution: “We have to find ways to better integrate older adults in the community as opposed to moving them to campuses where they are apart from the rest of us,” Power said. “We need to stop seeing older people only through the lens of what services they might need and think instead of all they have to offer society.”
That point is a core precept of the National Academy of Medicine’s 2022 report Global Roadmap for Healthy Longevity. Older people are a “natural resource” who “make substantial contributions to their families and communities,” the report’s authors write in introducing their findings.
Those contributions include financial support to families, caregiving assistance, volunteering, and ongoing participation in the workforce, among other things.
“When older people thrive, all people thrive,” the report concludes.
Future generations will get their turn. That’s a message Kramer conveys in classes he teaches at the University of Southern California, Cornell, and other institutions. “You have far more at stake in changing the way we approach aging than I do,” he tells his students. “You are far more likely, statistically, to live past 100 than I am. If you don’t change society’s attitudes about aging, you will be condemned to lead the last third of your life in social, economic, and cultural irrelevance.”
As for himself and the baby boom generation, Kramer thinks it’s “too late” to effect the meaningful changes he hopes the future will bring.
“I suspect things for people in my generation could get a lot worse in the years ahead,” Pillemer said. “People are greatly underestimating what the cost of caring for the older population is going to be over the next 10 to 20 years, and I think that’s going to cause increased conflict.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
“Skinny Fat” Explained (& How To Fix It)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Skinny fat” is a term you may have seen floating around social media. It describes people who have a low body weight but a high body fat percentage, often resulting in flabby appearance despite being within a weight range considered healthy. Many try dieting and exercising, only to find that neither work.
This video explains what’s going wrong, and how to fix it:
Diet & exercise won’t work if it’s not right
This problem occurs because common weight-loss approaches, such as restrictive dieting and excessive cardio, fail to improve body composition:
- Restrictive dieting reduces both fat and lean mass, keeping the body fat percentage unchanged
- Cardio burns some calories but the underlying metabolic issue hasn’t meaningfully changed, so any loss will be temporary (and most of any immediate loss will be water weight, anyway)
The key to overcoming skinny fat is resistance training. Lifting weights or doing bodyweight exercises helps build muscle, which not only lowers body fat percentage (by simple mathematics; add more muscle and the percentages of other things must go down even if the total amount is the same) and improves overall definition, which is something most people consider nice. However, the real value here is that it actually addresses the underlying metabolic issue—because muscle costs calories to maintain, one’s basal metabolic rate will now be faster, even when you’re sleeping.
This then becomes… Not quite a self-sustaining system, because you do have to still eat well and continue to do resistance training, but your body will be doing most of the work for you, and you’ll find it’s a lot easier to maintain a healthy body composition than to get one in the first place, for exactly the metabolic reason we described.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Visceral Belly Fat & How To Lose It ← this is a different, but adjacent issue (and very important for avoiding metabolic disease risks)
Take care!
Share This Post
Related Posts
-
Mental illness, psychiatric disorder or psychological problem. What should we call mental distress?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We talk about mental health more than ever, but the language we should use remains a vexed issue.
Should we call people who seek help patients, clients or consumers? Should we use “person-first” expressions such as person with autism or “identity-first” expressions like autistic person? Should we apply or avoid diagnostic labels?
These questions often stir up strong feelings. Some people feel that patient implies being passive and subordinate. Others think consumer is too transactional, as if seeking help is like buying a new refrigerator.
Advocates of person-first language argue people shouldn’t be defined by their conditions. Proponents of identity-first language counter that these conditions can be sources of meaning and belonging.
Avid users of diagnostic terms see them as useful descriptors. Critics worry that diagnostic labels can box people in and misrepresent their problems as pathologies.
Underlying many of these disagreements are concerns about stigma and the medicalisation of suffering. Ideally the language we use should not cast people who experience distress as defective or shameful, or frame everyday problems of living in psychiatric terms.
Our new research, published in the journal PLOS Mental Health, examines how the language of distress has evolved over nearly 80 years. Here’s what we found.
Engin Akyurt/Pexels Generic terms for the class of conditions
Generic terms – such as mental illness, psychiatric disorder or psychological problem – have largely escaped attention in debates about the language of mental ill health. These terms refer to mental health conditions as a class.
Many terms are currently in circulation, each an adjective followed by a noun. Popular adjectives include mental, mental health, psychiatric and psychological, and common nouns include condition, disease, disorder, disturbance, illness, and problem. Readers can encounter every combination.
These terms and their components differ in their connotations. Disease and illness sound the most medical, whereas condition, disturbance and problem need not relate to health. Mental implies a direct contrast with physical, whereas psychiatric implicates a medical specialty.
Mental health problem, a recently emerging term, is arguably the least pathologising. It implies that something is to be solved rather than treated, makes no direct reference to medicine, and carries the positive connotations of health rather than the negative connotation of illness or disease.
Is ‘mental health problem’ actually less pathologising? Monkey Business Images/Shutterstock Arguably, this development points to what cognitive scientist Steven Pinker calls the “euphemism treadmill”, the tendency for language to evolve new terms to escape (at least temporarily) the offensive connotations of those they replace.
English linguist Hazel Price argues that mental health has increasingly come to replace mental illness to avoid the stigma associated with that term.
How has usage changed over time?
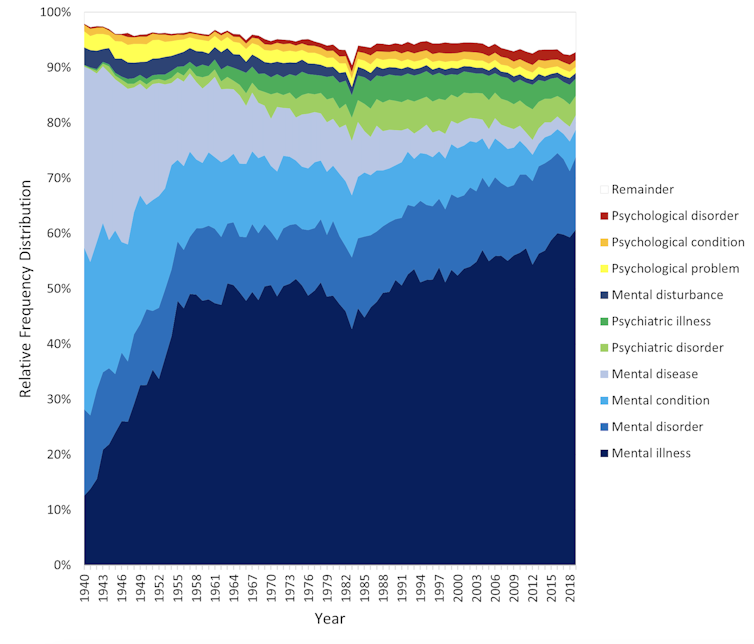
In the PLOS Mental Health paper, we examine historical changes in the popularity of 24 generic terms: every combination of the nouns and adjectives listed above.
We explore the frequency with which each term appears from 1940 to 2019 in two massive text data sets representing books in English and diverse American English sources, respectively. The findings are very similar in both data sets.
The figure presents the relative popularity of the top ten terms in the larger data set (Google Books). The 14 least popular terms are combined into the remainder.
Relative popularity of alternative generic terms in the Google Books corpus. Haslam et al., 2024, PLOS Mental Health. Several trends appear. Mental has consistently been the most popular adjective component of the generic terms. Mental health has become more popular in recent years but is still rarely used.
Among nouns, disease has become less widely used while illness has become dominant. Although disorder is the official term in psychiatric classifications, it has not been broadly adopted in public discourse.
Since 1940, mental illness has clearly become the preferred generic term. Although an assortment of alternatives have emerged, it has steadily risen in popularity.
Does it matter?
Our study documents striking shifts in the popularity of generic terms, but do these changes matter? The answer may be: not much.
One study found people think mental disorder, mental illness and mental health problem refer to essentially identical phenomena.
Other studies indicate that labelling a person as having a mental disease, mental disorder, mental health problem, mental illness or psychological disorder makes no difference to people’s attitudes toward them.
We don’t yet know if there are other implications of using different generic terms, but the evidence to date suggests they are minimal.
The labels we use may not have a big impact on levels of stigma. Pixabay/Pexels Is ‘distress’ any better?
Recently, some writers have promoted distress as an alternative to traditional generic terms. It lacks medical connotations and emphasises the person’s subjective experience rather than whether they fit an official diagnosis.
Distress appears 65 times in the 2022 Victorian Mental Health and Wellbeing Act, usually in the expression “mental illness or psychological distress”. By implication, distress is a broad concept akin to but not synonymous with mental ill health.
But is distress destigmatising, as it was intended to be? Apparently not. According to one study, it was more stigmatising than its alternatives. The term may turn us away from other people’s suffering by amplifying it.
So what should we call it?
Mental illness is easily the most popular generic term and its popularity has been rising. Research indicates different terms have little or no effect on stigma and some terms intended to destigmatise may backfire.
We suggest that mental illness should be embraced and the proliferation of alternative terms such as mental health problem, which breed confusion, should end.
Critics might argue mental illness imposes a medical frame. Philosopher Zsuzsanna Chappell disagrees. Illness, she argues, refers to subjective first-person experience, not to an objective, third-person pathology, like disease.
Properly understood, the concept of illness centres the individual and their connections. “When I identify my suffering as illness-like,” Chappell writes, “I wish to lay claim to a caring interpersonal relationship.”
As generic terms go, mental illness is a healthy option.
Nick Haslam, Professor of Psychology, The University of Melbourne and Naomi Baes, Researcher – Social Psychology/ Natural Language Processing, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Best Kind Of Fiber For Overall Health?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Fiber Of Good Health
We’ve written before about how most people in industrialized nations in general, and N. America in particular, do not get nearly enough fiber:
Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
Fiber’s important for many aspects of health, not least of all the heart:
What Matters Most For Your Heart? Eat More (Of This) For Lower Blood Pressure
As well, of course, as being critical for gut health:
Gut Health 101: Making Friends With Your Gut (You Can Thank Us Later)
But is all fiber “prebiotic fiber”, and/or are some better than others?
Beta-glucan
A recent study (it’s a mouse study, but promising in its applicability for humans) examined the health impacts of 5 different fiber types:
- pectin
- β-glucan
- wheat dextrin
- resistant starch
- cellulose (control)
As for health metrics, they measured:
- body weight
- adiposity
- indirect calorimetry
- glucose tolerance
- gut microbiota
- metabolites thereof
What they found was…
❝Only β-glucan supplementation during HFD-feeding decreased adiposity and body weight gain and improved glucose tolerance compared with HFD-cellulose, whereas all other fibers had no effect. This was associated with increased energy expenditure and locomotor activity in mice compared with HFD-cellulose.
All fibers supplemented into an HFD uniquely shifted the intestinal microbiota and cecal short-chain fatty acids; however, only β-glucan supplementation increased cecal butyrate concentrations. Lastly, all fibers altered the small-intestinal microbiota and portal bile acid composition. ❞
If you’d like to read more, the study itself is here:
If you’d like to read less, the short version is that they are all good but β-glucan scored best in several metrics.
It also acts indirectly as a GLP-1 agonist, by the way:
The right fiber may help you lose weight
You may be wondering: what is β-glucan found in?
It’s found in many (non-animal product) foods, but oats, barley, mushrooms, and yeasts are all good sources.
Is it available as a supplement?
More or less; there are supplements that contain it generously, here’s an example product on Amazon, a cordyceps extract, of which >30% is β-glucan.
As an aside, cordyceps itself has many other healthful properties too:
Cordyceps: Friend Or Foe? ← the answer is, it depends! If you’re human, it’s a friend.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Speedy Easy Ratatouille
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the biggest contributing factors to unhealthy eating? The convenience factor. To eat well, it seems, one must have at least two of the following: money, time, and skill. So today we have a health dish that’s cheap, quick, and easy!
(You won’t need a rat in a hat to help you with this one)
You will need
- 3 ripe tomatoes, roughly chopped
- 2 zucchini, halved and chopped into thick batons
- 2 portobello mushrooms, sliced into ½” slices
- 1 large red pepper, cut into thick chunks
- 3 tbsp extra virgin olive oil
- 2 tbsp finely chopped parsley
- 2 tsp garlic paste
- 2 tsp thyme leaves, destalked
- 1 tsp rosemary leaves, destalked
- 1 tsp red chili flakes
- 1 tsp black pepper
- Optional: 1 tsp MSG, or 1 tsp low sodium salt (the MSG is the healthier option as it contains less sodium than even low sodium salt)
- Optional: other vegetables, chopped. Use what’s in your fridge! This is a great way to use up leftovers. Particularly good options include chopped eggplant, chopped red onion, and/or chopped carrot.
Method
(we suggest you read everything at least once before doing anything)
1) Put the olive oil into a sauté pan and set the heat on medium. When hot but smoking, add the mushrooms and any optional vegetables (but not the others from the list yet), and fry for 5 minutes.
Note: if you aren’t pressed for time, then you can diverge from the “speedy” part of this by cooking each of the vegetables separately before combining, which allows each to keep its flavor more distinct.
2) Add the garlic, followed by the zucchini, red pepper, chili flakes, and thyme; stir periodically (you shouldn’t have to stir constantly) for 10 minutes.
3) Add the tomatoes and a cup of water to the pan, along with any MSG/salt. Cover with the lid and allow to simmer for a further 10 minutes.
4) Serve, adding the garnish.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- The Magic Of Mushrooms: “The Longevity Vitamin” (That’s Not A Vitamin)
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we had 3/5 today!
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
- MSG vs Salt: Sodium Comparison
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: