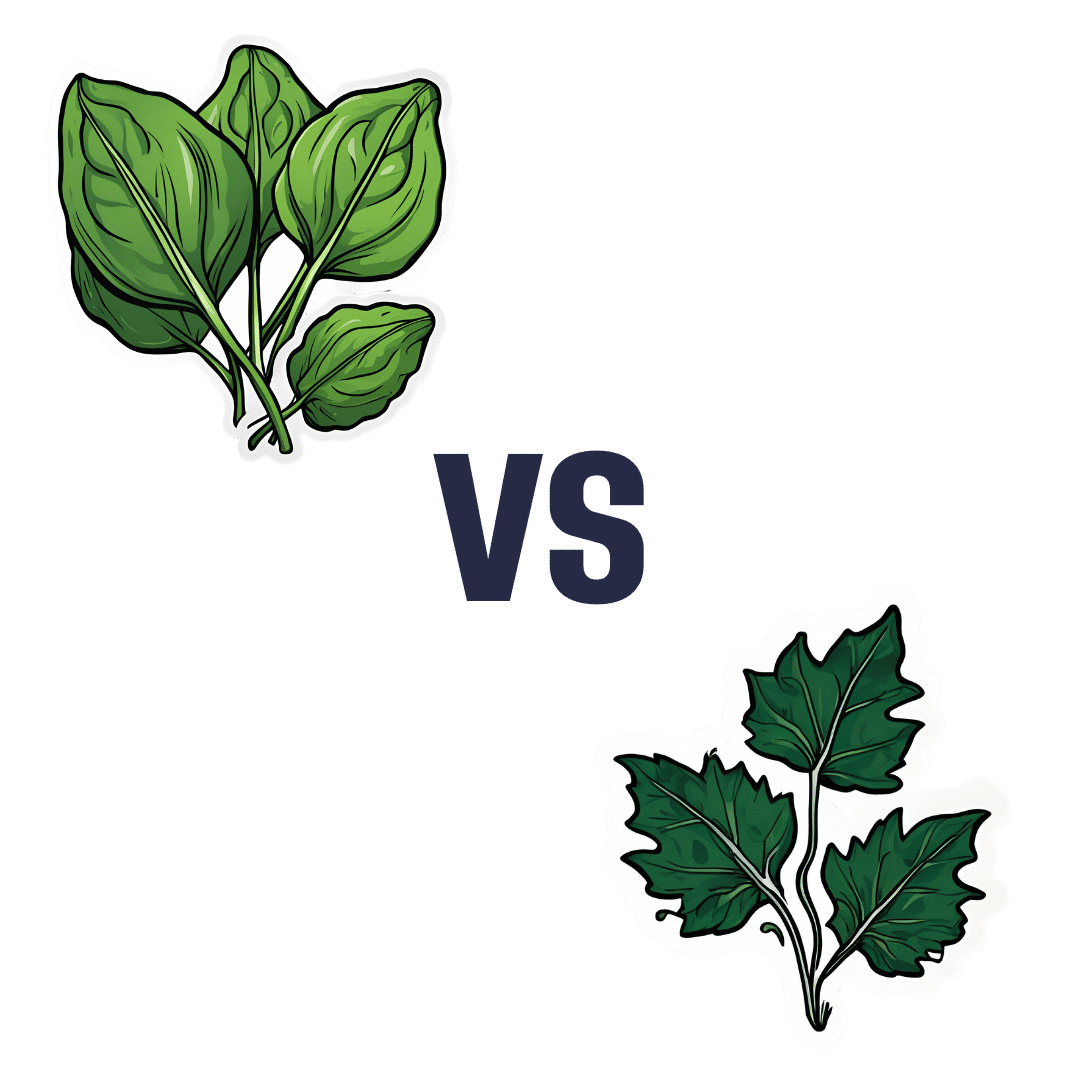
Spinach vs Vine Leaves – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing spinach to vine leaves, we picked the vine leaves.
Why?
Granted, they’re not available in most supermarkets, but if you live not too far from a wine-growing region, then they’ll be available at markets, and certainly stuffed vine leaves are thing found in many restaurants (though those are usually saltier than you’d make them at home—restaurants make most of their money from selling you drinks, after all, not the food). So, it’s worth noting the simple nutritional values if you prepare your own food:
In terms of macros, the most relevant difference is that vine leaves have about 5x the fiber. They’re also higher in carbs, but the overall glycemic index is lower in any case, so that’s not an issue. An easy win for vine leaves here.
Looking at vitamins, spinach has more of vitamins B1, B9, K, and choline, while vine leaves have more of vitamins A, B2, B3, B5, B6, B7, and C. Another win for vine leaves.
When it comes to minerals, spinach has more iron, potassium, and selenium, while vine leaves have more calcium, copper, magnesium, manganese, and phosphorus. One more win for vine leaves.
In terms of phytochemicals, spinach has a much higher oxalate content (that’s not a problem for most people, but bad if you have certain kidney issues).
Adding up the sections, it’s a clear overall win for vine leaves; by all means enjoy either or both though, unless you have kidney problems, of course!
Want to learn more?
You might like:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Crispy Tempeh & Warming Mixed Grains In Harissa Dressing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Comfort food that packs a nutritional punch! Lots of protein, fiber, vitamins, minerals, and healthy fats, and more polyphenols than you can shake a fork at.
You will need
- 1 lb cooked mixed whole grains (your choice what kind; gluten-free options include buckwheat, quinoa, millet)
- 7 oz tempeh, cut into ½” cubes
- 2 red peppers, cut into strips
- 10 baby plum tomatoes, halved
- 1 avocado, pitted, peeled, and diced
- 1 bulb garlic, paperwork done but cloves left whole
- 1 oz black olives, pitted and halved
- 4 tbsp extra virgin olive oil
- 2 tbsp harissa paste
- 2 tbsp soy sauce (ideally tamari)
- 1 tbsp nutritional yeast
- 1 tbsp chia seeds
- 2 tsp black pepper, coarse ground
- 1 tsp red chili flakes
- 1 handful chopped fresh flat-leaf parsley
- ½ tsp MSG or 1 tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400℉ / 200℃.
2) Combine the red pepper strips with the tomatoes, garlic, 2 tbsp of the olive oil, and the MSG/salt, tossing thoroughly to ensure an even coating. Spread them on a lined baking tray, and roast for about 25 minutes. Remove when done, and allow to cool a little.
3) Combine the tempeh with the soy sauce and nutritional yeast flakes, tossing thoroughly to ensure an even coating. Spread them on a lined baking tray, and roast for about 25 minutes, tossing regularly to ensure it is crispy on all sides. If you get started on the tempeh as soon as the vegetables are in the oven, these should be ready only a few minutes after the vegetables.
4) Whisk together the remaining olive oil and harissa paste in a small bowl, to make the dressing,
5) Mix everything in a big serving bowl. By “everything” we mean the roasted vegetables, the crispy tempeh, the mixed grains, the dressing, the chia seeds, the black pepper, the red chili flakes, and the flat leaf parsley.
6) Serve warm.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Grains: Bread Of Life, Or Cereal Killer?
- Tempeh vs Tofu – Which is Healthier?
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Share This Post
-
A Guide to the Good Life – by Dr. William Irvine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Living well” is a surprisingly underrated part of wellness. We spend much of our lives in turmoil. Some of us, windswept and battered by the storms of life; others, up in quietly crumbling towers, seemingly “great” but definitely not feeling it. Diet and exercise etc will only get us so far. What else, then, can we do?
For Dr. Irvine, the key lies in two main things:
- Deciding how we intend to live our life (and doing so)
- Remaining tranquil in the face of external stressors
In Japanese terms, these things can be seen in ikigai and zen, respectively. This book puts them in Western terms, specifically, that of Stoic philosophy. But the goals and methods are very similar.
Far from being an abstract tome of wishy-washy philosophy, this book offers down-to-earth practical exercises and easily applicable advice. There was even an exercise that was new to this reviewer who has been reading such things for decades.
The writing style is also, true to Stoic principles, unpretentious and simple. This is an easy book to read, while being nonethless very engaging from start to finish—and thereafter!
Bottom line: so far as we know, we only get one shot at life, so we might as well make it a good one. Applying the ideas found in this book can help any reader to live better, and take more joy in it along the way.
Click here to check out a Guide to the Good Life, and live your best!
Share This Post
-
How Primary Care Is Being Disrupted: A Video Primer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How patients are seeing their doctor is changing, and that could shape access to and quality of care for decades to come.
More than 100 million Americans don’t have regular access to primary care, a number that has nearly doubled since 2014. Yet demand for primary care is up, spurred partly by record enrollment in Affordable Care Act plans. Under pressure from increased demand, consolidation, and changing patient expectations, the model of care no longer means visiting the same doctor for decades.
KFF Health News senior correspondent Julie Appleby breaks down what is happening — and what it means for patients.
More From This Investigation
Primary Care Disrupted
Known as the “front door” to the health system, primary care is changing. Under pressure from increased demand, consolidation, and changing patient expectations, the model of care no longer means visiting the same doctor for decades. KFF Health News looks at what this means for patients.
Credits
Hannah Norman Video producer and animator Oona Tempest Illustrator and creative director KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
AI: The Doctor That Never Tires?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
AI: The Doctor That Never Tires?
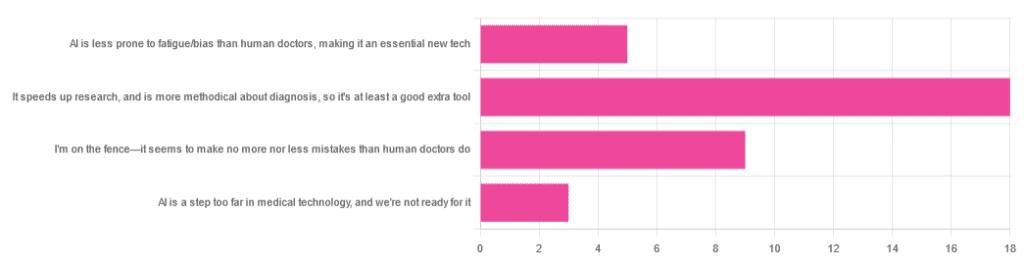
We asked you for your opinion on the use of Artificial Intelligence (AI) in healthcare, and got the above-depicted, below-described set of results:
- A little over half of respondents to the poll voted for “It speeds up research, and is more methodical about diagnosis, so it’s at least a good extra tool”
- A quarter of respondents voted for “I’m on the fence—it seems to make no more nor less mistakes than human doctors do”
- A little under a fifth of respondents voted for “AI is less prone to fatigue/bias than human doctors, making it an essential new tech”
- Three respondents voted for “AI is a step too far in medical technology, and we’re not ready for it”
Writer’s note: I’m a professional writer (you’d never have guessed, right?) and, apparently, I really did write “no more nor less mistakes”, despite the correct grammar being “no more nor fewer mistakes”. Now, I know this, and in fact, people getting less/fewer wrong is a pet hate of mine. Nevertheless, I erred.
Yet, now that I’m writing this out in my usual software, and not directly into the poll-generation software, my (AI!) grammar/style-checker is highlighting the error for me.
Now, an AI could not do my job. ChatGPT would try, and fail miserably. But can technology help me do mine better? Absolutely!
And still, I dismiss a lot of the AI’s suggestions, because I know my field and can make informed choices. I don’t follow it blindly, and I think that’s key.
AI is less prone to fatigue/bias than human doctors, making it an essential new tech: True or False?
True—with one caveat.
First, a quick anecdote from a subscriber who selected this option in the poll:
❝As long as it receives the same data inputs as my doctor (ie my entire medical history), I can see it providing a much more personalised service than my human doctor who is always forgetting what I have told him. I’m also concerned that my doctor may be depressed – not an ailment that ought to affect AI! I recently asked my newly qualified doctor goddaughter whether she would prefer to be treated by a human or AI doctor. No contest, she said – she’d go with AI. Her argument was that human doctors leap to conclusions, rather than properly weighing all the evidence – meaning AI, as long as it receives the same inputs, will be much more reliable❞
Now, an anecdote is not data, so what does the science say?
Well… It says the same:
❝Of 6695 responding physicians in active practice, 6586 provided information on the areas of interest: 3574 (54.3%) reported symptoms of burnout, 2163 (32.8%) reported excessive fatigue, and 427 (6.5%) reported recent suicidal ideation, with 255 of 6563 (3.9%) reporting a poor or failing patient safety grade in their primary work area and 691 of 6586 (10.5%) reporting a major medical error in the prior 3 months. Physicians reporting errors were more likely to have symptoms of burnout (77.6% vs 51.5%; P<.001), fatigue (46.6% vs 31.2%; P<.001), and recent suicidal ideation (12.7% vs 5.8%; P<.001).❞
See the damning report for yourself: Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors
AI, of course, does not suffer from burnout, fatigue, or suicidal ideation.
So, what was the caveat?
The caveat is about bias. Humans are biased, and that goes for medical practitioners just the same. AI’s machine learning is based on source data, and the source data comes from humans, who are biased.
See: Bias and Discrimination in AI: A Cross-Disciplinary Perspective
So, AI can perpetuate human biases and doesn’t have a special extra strength in this regard.
The lack of burnout, fatigue, and suicidal ideation, however, make a big difference.
AI speeds up research, and is more methodical about diagnosis: True or False?
True! AI is getting more and more efficient at this, and as has been pointed out, doesn’t make errors due to fatigue, and often comes to accurate conclusions near-instantaneously. To give just one example:
❝Deep learning algorithms achieved better diagnostic performance than a panel of 11 pathologists participating in a simulation exercise designed to mimic routine pathology workflow; algorithm performance was comparable with an expert pathologist interpreting whole-slide images without time constraints. The area under the curve was 0.994 (best algorithm) vs 0.884 (best pathologist).❞
About that “getting more and more efficient at this”; it’s in the nature of machine learning that every new piece of data improves the neural net being used. So long as it is getting fed new data, which it can process at rate far exceeding humans’ abilities, it will always be constantly improving.
AI makes no more nor
lessfewer mistakes than humans do: True or False?False! AI makes fewer, now. This study is from 2021, and it’s only improved since then:
❝Professionals only came to the same conclusions [as each other] approximately 75 per cent of the time. More importantly, machine learning produced fewer decision-making errors than did all the professionals❞
See: AI can make better clinical decisions than humans: study
All that said, we’re not quite at Star Trek levels of “AI can do a human’s job entirely” just yet:
BMJ | Artificial intelligence versus clinicians: pros and cons
To summarize: medical AI is a powerful tool that:
- Makes healthcare more accessible
- Speeds up diagnosis
- Reduces human error
…and yet, for now at least, still requires human oversights, checks and balances.
Essentially: it’s not really about humans vs machines at all. It’s about humans and machines giving each other information, and catching any mistakes made by the other. That way, humans can make more informed decisions, and still keep a “hand on the wheel”.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Best Menopause Advice You Don’t Want To Hear About
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nutritionist and perimenopause coach Claudia Canu, whom we’ve featured before in our Expert Insights segment, has advice:
Here’s to good health
When it comes to alcohol, the advice is: don’t.
Or at least, cut back, and manage the effects by ensuring good hydration, having an “alcohol curfew” and so forth.
What’s the relation to menopause? Well, alcohol’s not good for anyone at any time of life, but there are some special considerations when it comes to alcohol and estrogenic hormonal health:
- The liver works hard to process the alcohol as a matter of urgency, delaying estrogen processing, which can increase the risk of breast and uterine cancer.
- Alcohol has no positive health effects and is also linked to higher risks of breast and colorectal cancer.
- Alcohol can also trigger some menopausal symptoms, such as night sweats and hot flashes. So, maybe reaching for that “cooling drink” isn’t the remedy it might seem.
- During menopause, the body becomes more insulin-resistant, making it more susceptible to blood sugar spikes caused by alcohol. Also not good.
Common reasons women turn to alcohol include stress, frustration, the need for reward, and social pressure, and all of these can be heightened when undergoing hormonal changes. Yet, alcohol will ultimately only worsen each of those things.
For more on the science of some of the above, plus tips on how to make positive changes with minimum discomfort, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- How To Reduce Or Quit Alcohol
- How To Reduce The Harm Of Drinking (Without Abstaining)
- Where Nutrition Meets Habits! ← our “Expert Insights” spotlight on Canu
- How To Reduce Your Alzheimer’s Risk Early ← particularly important at this life stage
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The GLP-1 Lifestyle – by Dr. Joshua Hackett
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
While GLP-1 receptor agonists (i.e. semaglutide drugs such as Ozempic and Wegovy) have enjoyed the spotlight as a miracle cure (with some drawbacks), this book argues very reasonably that we should see them as a tool that we can use (or not) as part of a holistic approach to manage our metabolism.
Unusually, Dr. Hackett doesn’t argue strongly for one way or another, when it comes to using GLP-1 RAs. Rather, he makes the case that they indeed have pros and cons, and we should not only be aware of those pros and cons before making a decision either way, but also, we must understand the process of what goes on.
In contrast to the “inject it and forget it” marketing, he explains how if we actually understand what’s happening in our metabolism, we can improve things for ourselves and, at the very least, avoid sabotaging ourselves. Again, this knowledge is applicable with or without the drugs.
Much of the book is spent covering the physiological underpinnings and how things work for people of various different sizes and metabolic rates, as well as everything you’d expect about dosing, side effects, and whatnot—as well as things you might not have considered closely related, such gut health, and the question of “is there any way to retain the slimmer figure after stopping?”.
The style is methodical and clear, and not at all sensationalized. It’s very much a “read it cover to cover” book rather than a “dip in” book, so be ready for that, though.
Bottom line: if you and/or a loved one are on GLP1-RAs—or on the fence about them—this is a very even-minded and helpfully explanatory book.
Click here to check out The GLP-1 Lifestyle, and transform your metabolism!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: