3 drugs that went from legal, to illegal, then back again
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cannabis, cocaine and heroin have interesting life stories and long rap sheets. We might know them today as illicit drugs, but each was once legal.
Then things changed. Racism and politics played a part in how we viewed them. We also learned more about their impact on health. Over time, they were declared illegal.
But decades later, these drugs and their derivatives are being used legally, for medical purposes.
Here’s how we ended up outlawing cannabis, cocaine and heroin, and what happened next.
Cannabis, religion and racism
Cannabis plants originated in central Asia, spread to North Africa, and then to the Americas. People grew cannabis for its hemp fibre, used to make ropes and sacks. But it also had other properties. Like many other ancient medical discoveries, it all started with religion.
Cannabis is mentioned in the Hindu texts known as the Vedas (1700-1100 BCE) as a sacred, feel-good plant. Cannabis or bhang is still used ritually in India today during festivals such as Shivratri and Holi.
From the late 1700s, the British in India started taxing cannabis products. They also noticed a high rate of “Indian hemp insanity” – including what we’d now recognise as psychosis – in the colony. By the late 1800s, a British government investigation found only heavy cannabis use seemed to affect people’s mental health.
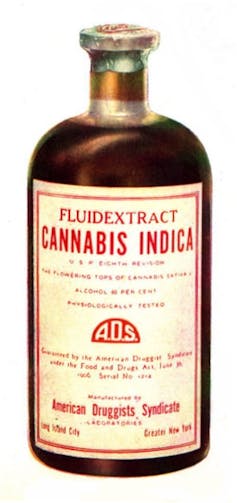
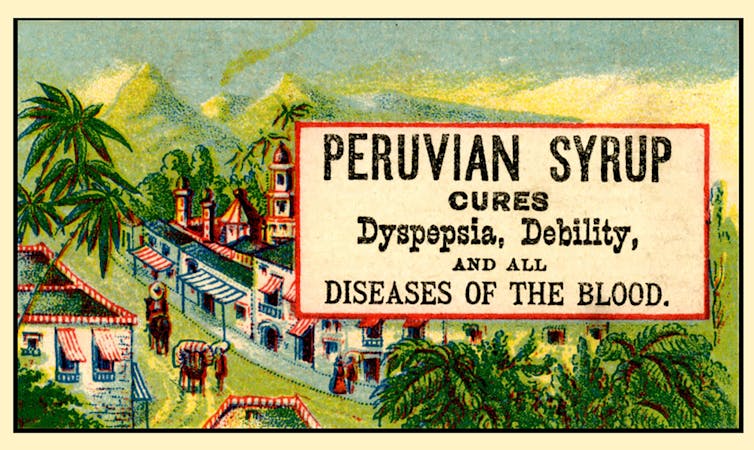
In the 1880s, cannabis was used therapeutically in the United States to treat tetanus, migraine and “insane delirium”. But not everyone agreed on (or even knew) the best dose. Local producers simply mixed up what they had into a tincture – soaking cannabis leaves and buds in alcohol to extract essential oils – and hoped for the best.
So how did cannabis go from a slightly useless legal drug to a social menace?
Some of it was from genuine health concerns about what was added to people’s food, drink and medicine.
In 1908 in Australia, New South Wales listed cannabis as an ingredient that could “adulterate” food and drink (along with opium, cocaine and chloroform). To sell the product legally, you had to tell the customers it contained cannabis.
Some of it was international politics. Moves to control cannabis use began in 1912 with the world’s first treaty against drug trafficking. The US and Italy both wanted cannabis included, but this didn’t happen until until 1925.
Some of it was racism. The word marihuana is Spanish for cannabis (later Anglicised to marijuana) and the drug became associated with poor migrants. In 1915, El Paso, Texas, on the Mexican border, was the first US municipality to ban the non-medical cannabis trade.
By the late 1930s, cannabis was firmly entrenched as a public menace and drug laws had been introduced across much of the US, Europe and (less quickly) Australia to prohibit its use. Cannabis was now a “poison” regulated alongside cocaine and opiates.
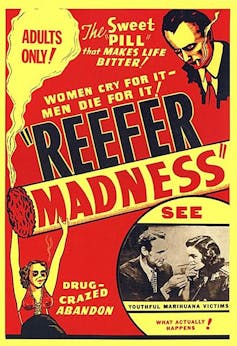
The 1936 movie Reefer Madness was a high point of cannabis paranoia. Cannabis smoking was also part of other “suspect” new subcultures such as Black jazz, the 1950s Beatnik movement and US service personnel returning from Vietnam.
Today recreational cannabis use is associated with physical and mental harm. In the short term, it impairs your functioning, including your ability to learn, drive and pay attention. In the long term, harms include increasing the risk of psychosis.
But what about cannabis as a medicine? Since the 1980s there has been a change in mood towards experimenting with cannabis as a therapeutic drug. Medicinal cannabis products are those that contain cannabidiol (CBD) or tetrahydrocannabinol (THC). Today in Australia and some other countries, these can be prescribed by certain doctors to treat conditions when other medicines do not work.
Medicinal cannabis has been touted as a treatment for some chronic conditions such as cancer pain and multiple sclerosis. But it’s not clear yet whether it’s effective for the range of chronic diseases it’s prescribed for. However, it does seem to improve the quality of life for people with some serious or terminal illnesses who are using other prescription drugs.
Cocaine, tonics and addiction
Several different species of the coca plant grow across Bolivia, Peru and Colombia. For centuries, local people chewed coca leaves or made them into a mildly stimulant tea. Coca and ayahuasca (a plant-based psychedelic) were also possibly used to sedate people before Inca human sacrifice.
In 1860, German scientist Albert Niemann (1834-1861) isolated the alkaloid we now call “cocaine” from coca leaves. Niemann noticed that applying it to the tongue made it feel numb.
But because effective anaesthetics such as ether and nitrous oxide had already been discovered, cocaine was mostly used instead in tonics and patent medicines.
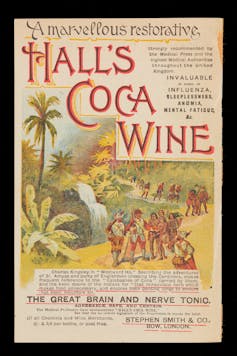
Perhaps the most famous example was Coca-Cola, which contained cocaine when it was launched in 1886. But cocaine was used earlier, in 1860s Italy, in a drink called Vin Mariani – Pope Leo XIII was a fan.
With cocaine-based products easily available, it quickly became a drug of addiction.
Cocaine remained popular in the entertainment industry. Fictional detective Sherlock Holmes injected it, American actor Tallulah Bankhead swore by it, and novelist Agatha Christie used cocaine to kill off some of her characters.
In 1914, cocaine possession was made illegal in the US. After the hippy era of the 1960s and 1970s, cocaine became the “it” drug of the yuppie 1980s. “Crack” cocaine also destroyed mostly Black American urban communities.
Cocaine use is now associated with physical and mental harms. In the short and long term, it can cause problems with your heart and blood pressure and cause organ damage. At its worst, it can kill you. Right now, illegal cocaine production and use is also surging across the globe.
But cocaine was always legal for medical and surgical use, most commonly in the form of cocaine hydrochloride. As well as acting as a painkiller, it’s a vasoconstrictor – it tightens blood vessels and reduces bleeding. So it’s still used in some types of surgery.
Heroin, coughing and overdoses
Opium has been used for pain relief ever since people worked out how to harvest the sap of the opium poppy. By the 19th century, addictive and potentially lethal opium-based products such as laudanum were widely available across the United Kingdom, Europe and the US. Opium addiction was also a real problem.
Because of this, scientists were looking for safe and effective alternatives for pain relief and to help people cure their addictions.
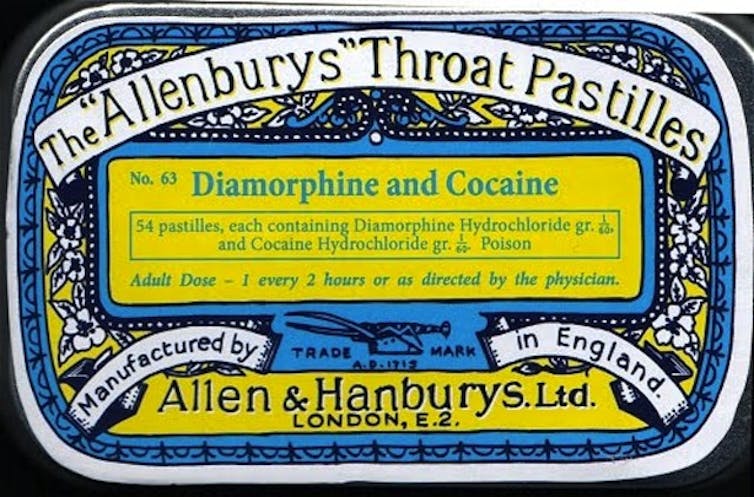
In 1874, English chemist Charles Romley Alder Wright (1844-1894) created diacetylmorphine (also known as diamorphine). Drug firm Bayer thought it might be useful in cough medicines, gave it the brand name Heroin and put it on the market in 1898. It made chest infections worse.
Although diamorphine was created with good intentions, this opiate was highly addictive. Shortly after it came on the market, it became clear that it was every bit as addictive as other opiates. This coincided with international moves to shut down the trade in non-medical opiates due to their devastating effect on China and other Asian countries.
Like cannabis, heroin quickly developed radical chic. The mafia trafficked into the US and it became popular in the Harlem jazz scene, beatniks embraced it and US servicemen came back from Vietnam addicted to it. Heroin also helped kill US singers Janis Joplin and Jim Morrison.
Today, we know heroin use and addiction contributes to a range of physical and mental health problems, as well as death from overdose.
However, heroin-related harm is now being outpaced by powerful synthetic opioids such as oxycodone, fentanyl, and the nitazene group of drugs. In Australia, there were more deaths and hospital admissions from prescription opiate overdoses than from heroin overdoses.
In a nutshell
Not all medicines have a squeaky-clean history. And not all illicit drugs have always been illegal.
Drugs’ legal status and how they’re used are shaped by factors such as politics, racism and social norms of the day, as well as their impact on health.
Philippa Martyr, Lecturer, Pharmacology, Women’s Health, School of Biomedical Sciences, The University of Western Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Reduce Your Alzheimer’s Risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Reduce Your Alzheimer’s Risk
Alzheimer’s is just one cause of dementia, but it’s a very notable one, not least of all because it’s
- a) the most common cause of dementia, and
- b) a measurably terminal disease.
For that reason we’re focusing on Alzheimer’s today, although most of the advice will go for avoiding dementia in general.
First, some things not everyone knows about Alzheimer’s:
- Alzheimer’s is a terminal disease.
- People who get a diagnosis at age 60 are typically given 4–8 years to live.
- Some soldier on for as many as 20, but those are rare outliers.
- Alzheimer’s begins 20 years or more before other symptoms start to develop.
- This makes this information very relevant for younger people approaching 40, for example.
- Alzheimer’s accounts for 60–80% of dementia, and affects around 6% of people over 60.
- By the age of 65, that figure is 10%. By the age of 70, however, the percentage is still about the same—this is because of the mortality rate preventing the accumulation of Alzheimer’s patients over time.
Want to know more? Read: 2023 Alzheimer’s Disease Facts And Figures Special Report ← this is a very comprehensive downloadablereference, by the way, including a lot of information about diagnosis, treatmentpathways, and earlyinterventions.
Speaking of diagnosis…
Know what the symptoms are… and aren’t!
Forgetting your car keys can be frustrating. Forgetting them frequently can be worrying.
But: there’s a difference between forgetting your car keys, and forgetting what car keys are used for. The latter is the kind of memory loss that’s more of a red flag for Alzheimer’s.
Similarly: forgetting someone’s name can be embarrassing. Forgetting someone’s name, asking them, forgetting asking them, asking them again, forgetting again (lather rinse repeat) is more of a red flag for Alzheimer’s.
There are other symptoms too, some of them less commonly known:
❝Difficulty remembering recent conversations, names or events; apathy; and depression are often early symptoms. Communication problems, confusion, poor judgment and behavioral changes may occur next. Difficulty walking, speaking, and swallowing are common in the late stages of the disease❞
If you or a loved one are experiencing worrying symptoms: when it comes to diagnosis and intervention, sooner is a lot better than later, so do talk to your doctor.
As for reducing your risk? First, the obvious stuff:
The usual 5 things that go for almost everything:
- Have a good diet—the Mediterranean Diet is once again recommended (we expect this will not be a surprise to regular readers!)
- Get regular exercise—in the case of avoiding Alzheimer’s and other dementias, typically the most important thing here is heart health, so getting regular cardiovascular exercise, such walking, running, or dancing is great. Cycling too. Swimming, not so much. Not that swimming’s bad or anything, it’s just that when your body is horizontal, the heart has less work to do, especially in the upper part of the body, because it’s not defying gravity. Similarly, yoga is great for the health but won’t particularly help with this, nor will weight training.
- Get good sleep—as we get older, we tend to need less sleep, and tend more towards the lower end of the standard “7–9 hours” prescription, but getting at least those 7 hours makes a huge difference.
- Cut down (or eliminate) alcohol consumption—and especially avoid binge-drinking. While “binge-drinking” is typically associated with young people, that Christmas party where that one uncle gets very drunk is also binge-drinking, for example. Plus, heavy drinking in early life has also been correlated with higher risk of Alzheimer’s later.
- Don’t smoke. It’s bad for everything, and Alzheimer’s risk is no exception.
How much do lifestyle changes alone make a difference?
They make a big difference. This 2022 population-based cohort study (so: huge sample size) looked at people who had 4–5 of the healthy lifestyle factors being studied, vs people who had 0–1 of them. They found:
❝A healthy lifestyle was associated with a longer life expectancy among men and women, and they lived a larger proportion of their remaining years without Alzheimer’s dementia.❞
The numbers of years involved by the way ranged between 3 and 20 years, in terms of life expectancy and years without or with Alzheimer’s, with the average increase of healthy life years being approximately the same as the average increase in years. This is important, because:
A lot of people think “well if I’m going to go senile, I might as well [unhealthy choice that shortens lifespan]”, but they misunderstand a critical factor:
The unhealthy choices will reduce their healthy life years, and simply bring the unhealthy ones (and subsequent death) sooner. If you’re going to spend your last few years in ill-health, it’s better to do so at 90 than 50.
The other thing you may already know… And a thing about it that not everyone considers:
Keeping cognitively active is important. This much is broadly known by the general public, and to clinicians, this was the fourth “healthy factor” in the list of five (instead of the sleep that we put there, because we were listing the 5 things that go for most preventable health issues).
Everyone leaps to mention sudoku at this point, so if that’s your thing, great, enjoy it! (This writer personally enjoys chess, which isn’t everyone’s cup of tea; if it yours though, you can come join her on Chess.com and we’ll keep sharp together)
But the more parts of your mental faculties you keep active, the better. Remember, brainpower (as with many things in health and life) is a matter of “use it or lose it” and this is on a “per skill” basis!
What this means: doing sudoku (a number-based puzzle game) or chess (great as it may be) won’t help as much for keeping your language skills intact, for example. Given that language skills are one of the most impactful and key faculties to get lost to Alzheimer’s disease, neglecting such would be quite an oversight!
Some good ways to keep your language skills tip-top:
- Read—but read something challenging, if possible. It doesn’t have to be Thomas Scanlon’s What We Owe To Each Other, but it should be more challenging than a tabloid, for example. In fact, on the topic of examples:
- This newsletter is written to be easy to read, while not shying away from complex ideas or hard science. Our mission is literally to “make [well-sourced, science-based] health and productivity crazy simple”.
- But the academic papers that we link? Those aren’t written to be easy to read. Go read them, or at least the abstracts (in academia, an abstract is essentially an up-front summary, and is usually the first thing you’ll see when you click a link to a study or such). Challenge yourself!
- Write—compared to reading/listening, producing language is a (related, but) somewhat separate skill. Just ask any foreign language learner which is more challenging: reading or writing!
- Journaling is great, but writing for others is better (as then you’ll be forced to think more about it)
- Learn a foreign language—in this case, what matters it that you’re practicing and learning, so in the scale of easy to hard, or doesn’t matter if it’s Esperanto or Arabic. Duolingo is a great free resource that we recommend for this, and they have a wide range of extensive courses these days.
Now for the least obvious things…
Social contact is important.
Especially in older age, it’s easy to find oneself with fewer remaining friends and family, and getting out and about can be harder for everyone. Whatever our personal inclinations (some people being more introverted or less social than others), we are fundamentally a social species, and hundreds of thousands of years of evolution have built us around the idea that we will live our lives alongside others of our kind. And when we don’t, we don’t do as well.
See for example: Associations of Social Isolation and Loneliness With Later Dementia
If you can’t get out and about easily:
- Online socialising is still socializing.
- Online community is still community.
- Online conversations between friends are still conversations between friends.
If you don’t have much (or anyone) in the category of friends and family, join Facebook groups related to your interests, for example.
Berries are surprisingly good
^This may read like a headline from 200,000 BCE, but it’s relevant here!
Particularly recommended are:
- blueberries
- blackberries
- raspberries
- strawberries
- cranberries
We know that many of these berries seem to have a shelf-life of something like 30 minutes from time of purchase, but… Frozen and dried are perfectly good nutritionally, and in many cases, even better nutritionally than fresh.
Read: Effect of berry-based supplements and foods on cognitive function: a systematic review
Turmeric’s health benefits appear to include protecting against Alzheimer’s
Again, this is about risk reduction, and turmeric (also called curcumin, which is not the same as cumin) significantly reduces the build-up of amyloid plaques in the brain. Amyloid plaques are part of the progression of Alzheimer’s.
See for yourself: Protective Effects of Indian Spice Curcumin Against Amyloid Beta in Alzheimer’s Disease
If you don’t like it as a spice (and even if you do, you probably don’t want to put it in your food every day), you can easily get it as a supplement in capsule form.
Lower your homocysteine levels
Lower our what now? Homocysteine is an amino acid used for making certain proteins, and it’s a risk factor for Alzheimer’s.
Foods high in folate (and possible other B-vitamins) seem to lower homocysteine levels. Top choices include:
- Leafy greens
- Cruciferous vegetables
- Tomatoes
Get plenty of lutein
We did a main feature about specifically this a little while ago, so we’ll not repeat our work here, but lutein is found in, well, the same things we just listed above, and lower levels of lutein are associated with Alzheimer’s disease. It’s not a proven causative factor—we don’t know entirely what causes Alzheimer’s, just a lot of factors that have a high enough correlation that it’d be remiss to ignore them.
Catch up on our previous article: Brain Food? The Eyes Have It
Share This Post
-
Dancing vs Parkinson’s Depression
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a fun study, and the results are/were very predictable, and/but not necessarily something that people might think of in advance. First, let’s look at how some things work:
Parkinson’s disease & depression
Parkinson’s disease is a degenerative neurological disease that, amongst other things, is characterized by low dopamine levels.
For the general signs and symptoms, see: Recognize The Early Symptoms Of Parkinson’s Disease
Dopamine is the neurotransmitter responsible for feelings of reward, is involved in our language faculties and the capacity to form plans (even simple plans such as “make a cup of coffee”) as well as being critical for motor functions.
See also: Neurotransmitter Cheatsheet ← for demystifying some of “what does what” for commonly-conflated chemicals
You can see, therefore, why Parkinson’s disease will often have depression as a comorbidity—there may be influencing social factors as well (many Parkinson’s disease sufferers are quite socially isolated, which certainly does not help), but a clear neurochemical factor that we can point to is “a person with low dopamine levels will feel joyless, bored, and unmotivated”.
Let movement be thy medicine
Parkinson’s disease medications, therefore, tend to involve increasing dopamine levels and/or the brain’s ability to use dopamine.
Antidepressant medications, however, are more commonly focused on serotonin, as serotonin is another neurotransmitter associated with happiness—it’s the one we get when we look at open green spaces with occasional trees and a blue sky ← we get it in other ways too, but for evolutionary reasons, it seems our brains still yearn the most for landscapes that look like the Serengeti, even if we have never even been there personally.
There are other kinds of antidepressants too, and (because depression can have different causes) what works for one person won’t necessarily work for another. See: Antidepressants: Personalization Is Key!
In the case of Parkinson’s disease, because the associated depression is mostly dopamine-related, those green spaces and blue skies and SSRIs won’t help much. But you know what does?
Dance!
A recent (published last month, at time of writing) study by Dr. Karolina Bearss et al. did an interventional study that found that dance classes significantly improved both subjective experience of depression, and objective brain markers of depression, across people with (68%) and without (32%) Parkinson’s disease.
The paper is quite short and it has diagrams, and discusses the longer-term effect as well as the per-session effect:
Dance is thought to have a double-effect, improving both cognitive factors and motor control factors, for obvious reasons, and all related to dopamine response (dancing is an activity we are hardwired to find rewarding*, plus it is exercise which also triggers various chemicals to be made, plus it is social, which also improves many mental health factors).
*You may have heard the expression that “dancing is a vertical expression of a horizontal desire”, and while that may not be true for everyone on an individual level, on a species level it is a very reasonable hypothesis for why we do it and why it is the way it is.
Want to learn more?
We wrote previously about battling depression (of any kind) here:
The Mental Health First-Aid That You’ll Hopefully Never Need
Take care!
Share This Post
-
Thinking about cosmetic surgery? New standards will force providers to tell you the risks and consider if you’re actually suitable
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
People considering cosmetic surgery – such as a breast augmentation, liposuction or face lift – should have extra protection following the release this week of new safety and quality standards for providers, from small day-clinics through to larger medical organisations.
The new standards cover issues including how these surgeries are advertised, psychological assessments before surgery, the need for people to be informed of risks associated with the procedure, and the type of care people can expect during and afterwards. The idea is for uniform standards across Australia.
The move is part of sweeping reforms of the cosmetic surgery industry and the regulation of medical practitioners, including who is allowed to call themselves a surgeon.
It is heartening to see these reforms, but some may say they should have come much sooner for what’s considered a highly unregulated area of medicine.
Why do people want cosmetic surgery?
Australians spent an estimated A$473 million on cosmetic surgery procedures in 2023.
The major reason people want cosmetic surgery relates to concerns about their body image. Comments from their partners, friends or family about their appearance is another reason.
The way cosmetic surgery is portrayed on social media is also a factor. It’s often portrayed as an “easy” and “accessible” fix for concerns about someone’s appearance. So such aesthetic procedures have become far more normalised.
The use of “before” and “after” images online is also a powerful influence. Some people may think their appearance is worse than the “before” photo and so they think cosmetic intervention is even more necessary.
People don’t always get the results they expect
Most people are satisfied with their surgical outcomes and feel better about the body part that was previously concerning them.
However, people have often paid a sizeable sum of money for these surgeries and sometimes experienced considerable pain as they recover. So a positive evaluation may be needed to justify these experiences.
People who are likely to be unhappy with their results are those with unrealistic expectations for the outcomes, including the recovery period. This can occur if people are not provided with sufficient information throughout the surgical process, but particularly before making their final decision to proceed.
What’s changing?
According to the new standards, services need to ensure their own advertising is not misleading, does not create unreasonable expectations of benefits, does not use patient testimonials, and doesn’t offer any gifts or inducements.
For some clinics, this will mean very little change as they were not using these approaches anyway, but for others this may mean quite a shift in their advertising strategy.
It will likely be a major challenge for clinics to monitor all of their patient communication to ensure they adhere to the standards.
It is also not quite clear how the advertising standards will be monitored, given the expanse of the internet.
What about the mental health assessment?
The new standards say clinics must have processes to ensure the assessment of a patient’s general health, including psychological health, and that information from a patient’s referring doctor be used “where available”.
According to the guidelines from the Medical Board of Australia, which the standards are said to complement, all patients must have a referral, “preferably from their usual general practitioner or if that is not possible, from another general practitioner or other specialist medical practitioner”.
While this is a step in the right direction, we may be relying on medical professionals who may not specialise in assessing body image concerns and related mental health conditions. They may also have had very little prior contact with the patient to make their clinical impressions.
So these doctors need further training to ensure they can perform assessments efficiently and effectively. People considering surgery may also not be forthcoming with these practitioners, and may view them as “gatekeepers” to surgery they really want to have.
Ideally, mental health assessments should be performed by health professionals who are extensively trained in the area. They also know what other areas should be explored with the patient, such as the potential impact of trauma on body image concerns.
Of course, there are not enough mental health professionals, particularly psychologists, to conduct these assessments so there is no easy solution.
Ultimately, this area of health would likely benefit from a standard multidisciplinary approach where all health professionals involved (such as the cosmetic surgeon, general practitioner, dermatologist, psychologist) work together with the patient to come up with a plan to best address their bodily concerns.
In this way, patients would likely not view any of the health professionals as “gatekeepers” but rather members of their treating team.
If you’re considering cosmetic surgery
The Australian Commission on Safety and Quality in Health Care, which developed the new standards, recommended taking these four steps if you’re considering cosmetic surgery:
-
have an independent physical and mental health assessment before you commit to cosmetic surgery
-
make an informed decision knowing the risks
-
choose your practitioner, knowing their training and qualifications
-
discuss your care after your operation and where you can go for support.
My ultimate hope is people safely receive the care to help them best overcome their bodily concerns whether it be medical, psychological or a combination.
Gemma Sharp, Associate Professor, NHMRC Emerging Leadership Fellow & Senior Clinical Psychologist, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Related Posts
-
Superfood Broccoli Pesto
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cruciferous vegetables have many health benefits of their own (especially: a lot of anticancer benefits). But, it can be hard to include them in every day’s menu, so this is just one more way that’ll broaden your options! It’s delicious mixed into pasta, or served as a dip, or even on toast.
You will need
- 4 cups small broccoli florets
- 1 cup fresh basil leaves
- ½ cup pine nuts
- ¼ bulb garlic
- 3 tbsp extra virgin olive oil
- 2 tbsp nutritional yeast
- 1 tbsp lemon juice
- 2 tsp black pepper, coarse ground
- 1 tsp red pepper flakes
- ½ tsp MSG or 1 tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Steam the broccoli for 3–5 minutes. Allow to cool.
2) Blend the pine nuts, garlic, lemon juice, and nutritional yeast.
3) Add the broccoli, basil, olive oil, black pepper, red pepper, and MSG or salt, and blend in the food processor again until well-combined.
4) Serve:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Broccoli vs Cauliflower – Which is Healthier?
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Herbs for (Evidence-Based) Health & Healing ← Basil features here! It’s easy to think that medicinal herbs have to be some kind of arcane obscurity, but it’s often not so.
- Our Top 5 Spices: How Much Is Enough For Benefits? ← Black pepper, red pepper, and garlic all feature here
- All About Olive Oil: Is “Extra Virgin” Worth It?
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Blood-Sugar Balancing Beetroot Cutlets
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
These beetroot cutlets are meaty and proteinous and fibrous and even have a healthy collection of fats, making these much better for your heart and blood than an animal-based equivalent.
You will need
- 1 can kidney beans, drained and rinsed (or 1 cup same, cooked, drained, and rinsed)
- ½ cup chopped roasted or steamed beetroot, blotted dry
- ½ cup chopped walnuts (if allergic, substitute with ¼ cup pumpkin seeds)
- ½ cup cooked (ideally: mixed) grains of your choice (if you need gluten-free, there are plenty of gluten-free grains and pseudocereals)
- ¼ cup finely chopped onion
- ¼ bulb garlic, minced or crushed
- 2 tbsp nutritional yeast
- 2 tbsp ground flaxseeds
- 2 tbsp ground chia seeds
- 2 tsp tomato purée
- 1 tsp black pepper
- ½ tsp white miso paste
- ½ tsp smoked paprika
- ½ tsp cayenne pepper
- ¼ tsp MSG or ½ tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Combine the beetroot, beans, walnuts, grains, and onion in a food processor, and process until a coarse even mixture.
2) Add the remaining ingredients and process to mix thoroughly.
3) Transfer the mixture to a clean work surface and divide into six balls. If the structural integrity is not good (i.e. too soft), add a little more of any or all of these ingredients: chopped walnuts, ground flax, ground chia, nutritional yeast.
4) Press the balls firmly into cutlets, and refrigerate for at least 1 hour, but longer is even better if you have the time. Alternatively, if you’d like to freeze them for later use, then this is the point at which to do that.
5) Preheat the oven to 375℉ / 190℃.
6) Roast the cutlets on a baking tray lined with baking paper, for about 30 minutes, turning over carefully with a spatula halfway through. They should be firm when done; if they’re not, give them a little longer.
7) Serve hot, for example on a bed of greens and with a drizzle of aged balsamic vinegar.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Beetroot’s Many Benefits
- Our Top 5 Spices: How Much Is Enough For Benefits?
- What Omega-3 Fatty Acids Really Do For Us
- Three Daily Servings of Beans?
- If You’re Not Taking Chia, You’re Missing Out
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
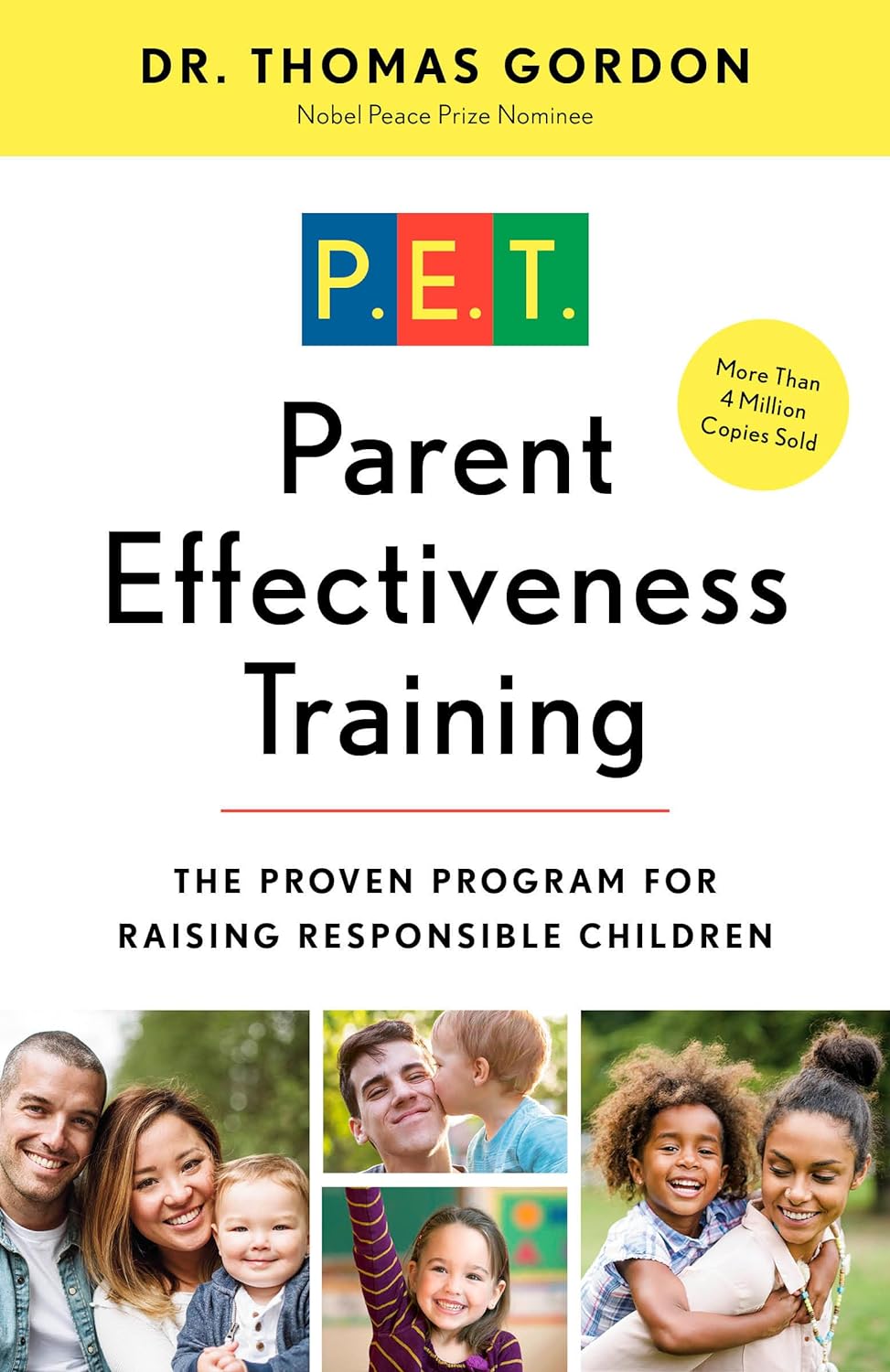
Parent Effectiveness Training – by Dr. Thomas Gordon
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Do you want your home (or workplace, for that matter) to be a place of peace? This book literally got the author nominated for a Nobel Peace Prize. Can’t really get much higher praise than that.
The title is “Parent Effectiveness Training”, but in reality, the advice in the book is applicable to all manner of relationships, including:
- romantic relationships
- friends
- colleagues
- …and really any human interaction.
It covers some of the same topics we did today (and more) in much more detail than we ever could in a newsletter. It lays out formulae to use, gives plenty of examples, and/but is free from undue padding.
- Pros: this isn’t one of those “should have been an article” books. It has so much valuable content.
- Cons: It is from the 1970s* so examples may feel “dated” now.
In addition to going into much more detail on some of the topics covered in today’s issue of 10almonds, Dr. Gordon also talks in-depth about the concept of “problem-ownership”.
In a nutshell, that means: whose problem is a given thing? Who “has” what problem? Everyone needs to be on the same page about everyone else’s problems in the situation… as well as their own, which is not always a given!
Dr. Gordon presents, in short, tools not just to resolve conflict, but also to pre-empt it entirely. With these techniques, we can identify and deal with problems (together!) well before they arise.
Everybody wins.
Get your copy of “Parent Effectiveness Training” from Amazon today!
*Note: There is an updated edition on the market, and that’s what you’ll find upon following the above link. This reviewer (hi!) has a battered old paperback from the 1970s and cannot speak for what was changed in the new edition. However: if the 70s one is worth more than its weight in gold (and it is), the new edition is surely just as good, if not better!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: