Future-Proof Your Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
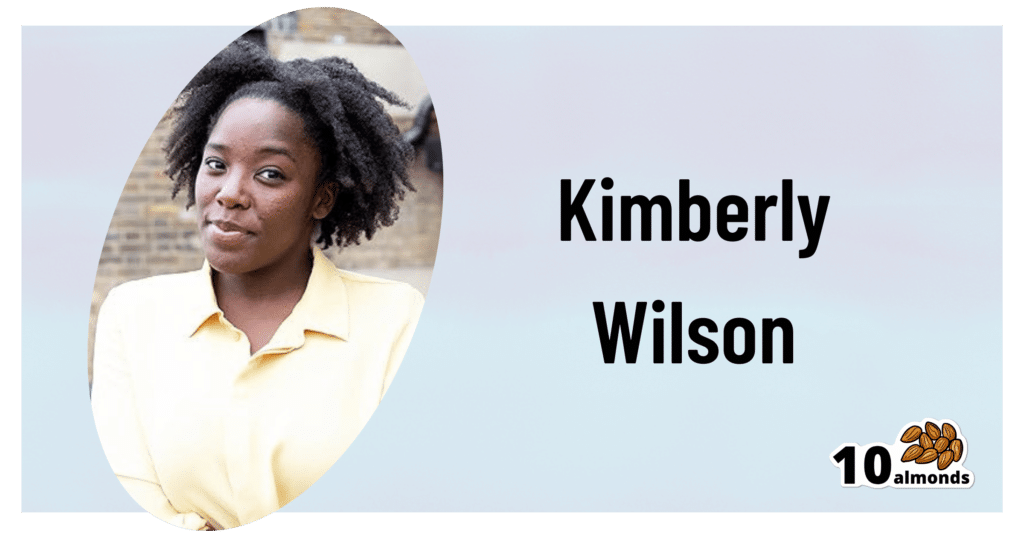
This is Kimberly Wilson. She’s a psychologist, not a doctor, and/but her speciality is neurophysiology and brain health.
Here’s what she wants us to know…
Avoid this very common killer
As you’re probably aware, the #1 killer in the US is heart disease, followed by COVID, which effectively pushed everything down a place. Thereafter, we see cancer, followed by accidental injuries, stroke, and dementia (including Alzheimer’s).
Over in the UK, where Wilson is from, dementia (including Alzheimer’s disease) is the #1 killer, followed by heart disease and then respiratory diseases (including COVID), and then stroke, then cancer.
As ever, what’s good for the heart is good for the brain, so many of the same interventions will help avoid both. With regard to some of the other differences in order, the reasons are mostly due to differences in the two countries’ healthcare systems and firearms laws.
It’s worth noting, though, that the leading cause of death in young people (aged 15–19) is suicide in the UK; in the US it’s nominally accidental injuries first (e.g. accidental shootings) with intentional suicide in the second spot.
In other words… Young or old, mental health is a serious health category that kills literally the most people in the UK, and also makes the top spots in the US.
Avoid the early killer
Given the demographics of most of our readership, chances are you’ve already lived past your teens and twenties. That’s not to say that suicide is no longer a risk, though, and it’s also worth noting that while mental health issues are invisible, they’re still physical illnesses (the brain is also an organ, after all!), so this isn’t something where you can simply “decide not to” and that’s you set, safe for life. So, please do continue to take good care in that regard.
We wrote about this previously, here:
How To Stay Alive (When You Really Don’t Want To)
Avoid the later killer
Wilson talks about how a recent survey found that…
- while nearly half of adults say dementia is the disease they fear most,
- only a third of those thought you could do anything to avoid it, and
- just 1% could name the 7 known risk factors.
Quick test: can you name the 7 known risk factors?
Please take a moment to actually try (this kind of mental stimulation is good in any case), and count them out on your fingers (or write them down), and then…
When you’re ready: click here to see the answer!
How many did you get? If you got them all, well done. If not, then well, now you know, so that’s good.
So, with those 7 things in mind, the first obvious advice is to take care of those things.
Taking an evidence-based medicine approach, Wilson recommends some specific interventions that will each improve one or more of those things, directly or indirectly:
Eating right
Wilson is a big fan of “nutritional psychiatry” and feeding one’s brain properly. We wrote about this, here:
The 6 Pillars Of Nutritional Psychiatry
As well as agreeing with the obvious “eat plenty of fiber, different-colored plants, and plenty of greens and beans”, Wilson specifically also champions getting enough of vitamins B9, B12, and D, as well as getting a healthy dose of omega-3 fatty acids.
She also recommends intermittent fasting, if that’s a reasonable option for you—but advocates for not worrying about it, if it’s not easy for you. For example, if you are diabetic, or have (or have a history with) some kind of eating disorder(s), then it’s probably not usefully practicable. But for most people, it can reduce systemic inflammation, which means also reducing neuroinflammation.
Managing stress right
Here she advocates for three main things:
- Mindful meditation (see: Evidence-Based, No-Frills Mindfulness)
- Psychological resilience (see: Building Psychological Resilience)
- Mindful social media use (see: Making Social Media Work For Your Mental Health)
Managing money right
Not often we talk about this in a health science publication as opposed to a financial planning publication, but the fact is that a lot of mental distress, which goes on to have a huge impact on the brain, is rooted in financial stresses.
And, of course, it’s good to be able to draw on financial resources to directly fund one’s good health, but that is the secondary consideration here—the financial stress is the biggest issue, and you can’t CBT your way out of debt, for example.
Therapists often face this, and what has been referred to informally by professionals in the field as “Shit Life Syndrome”—and there’s only so much that therapy can do about that.
We’re not a financial publication, but one recommendation we’ll drop is that if you don’t currently have budgeting software that you use, this writer personally uses and swears by YNAB (You Need A Budget), so maybe check that out if you don’t already have everything covered in that regard. It’s not free, but there is a 34-day free trial.
Therapy can be very worthwhile nonetheless
Wilson notes that therapy is like non-invasive brain surgery (because of neuroplasticity, it’s literally changing physical things in your brain).
It’s not a magic bullet and it’s not the right choice for everyone, but it’s worth considering, and even self-therapy can yield benefits for many:
The Gym For Your Mental Health: Getting The Most Out Of Therapy
Sleeping right
Sleep is not only critical for health in general and brain health in particular, it’s also most of when our glymphatic system does clean-up in the brain (essential for avoiding Alzheimer’s & Parkinson’s, amongst other diseases):
How To Clean Your Brain (Glymphatic Health Primer)
Want to know more from Kimberley Wilson?
We reviewed a book of hers recently, here:
Unprocessed: What your Diet Is Doing To Your Brain – by Kimberley Wilson
However, much of what we shared today was sourced from another book of hers that we haven’t reviewed yet but probably will do one of these days:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Alzheimer’s may have once spread from person to person, but the risk of that happening today is incredibly low
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
An article published this week in the prestigious journal Nature Medicine documents what is believed to be the first evidence that Alzheimer’s disease can be transmitted from person to person.
The finding arose from long-term follow up of patients who received human growth hormone (hGH) that was taken from brain tissue of deceased donors.
Preparations of donated hGH were used in medicine to treat a variety of conditions from 1959 onwards – including in Australia from the mid 60s.
The practice stopped in 1985 when it was discovered around 200 patients worldwide who had received these donations went on to develop Creuztfeldt-Jakob disease (CJD), which causes a rapidly progressive dementia. This is an otherwise extremely rare condition, affecting roughly one person in a million.
What’s CJD got to do with Alzehimer’s?
CJD is caused by prions: infective particles that are neither bacterial or viral, but consist of abnormally folded proteins that can be transmitted from cell to cell.
Other prion diseases include kuru, a dementia seen in New Guinea tribespeople caused by eating human tissue, scrapie (a disease of sheep) and variant CJD or bovine spongiform encephalopathy, otherwise known as mad cow disease. This raised public health concerns over the eating of beef products in the United Kingdom in the 1980s.
Human growth hormone used to come from donated organs
Human growth hormone (hGH) is produced in the brain by the pituitary gland. Treatments were originally prepared from purified human pituitary tissue.
But because the amount of hGH contained in a single gland is extremely small, any single dose given to any one patient could contain material from around 16,000 donated glands.
An average course of hGH treatment lasts around four years, so the chances of receiving contaminated material – even for a very rare condition such as CJD – became quite high for such people.
hGH is now manufactured synthetically in a laboratory, rather than from human tissue. So this particular mode of CJD transmission is no longer a risk.
Human growth hormone is now produced in a lab.
National Cancer Institute/UnsplashWhat are the latest findings about Alzheimer’s disease?
The Nature Medicine paper provides the first evidence that transmission of Alzheimer’s disease can occur via human-to-human transmission.
The authors examined the outcomes of people who received donated hGH until 1985. They found five such recipients had developed early-onset Alzheimer’s disease.
They considered other explanations for the findings but concluded donated hGH was the likely cause.
Given Alzheimer’s disease is a much more common illness than CJD, the authors presume those who received donated hGH before 1985 may be at higher risk of developing Alzheimer’s disease.
Alzheimer’s disease is caused by presence of two abnormally folded proteins: amyloid and tau. There is increasing evidence these proteins spread in the brain in a similar way to prion diseases. So the mode of transmission the authors propose is certainly plausible.
However, given the amyloid protein deposits in the brain at least 20 years before clinical Alzheimer’s disease develops, there is likely to be a considerable time lag before cases that might arise from the receipt of donated hGH become evident.
When was this process used in Australia?
In Australia, donated pituitary material was used from 1967 to 1985 to treat people with short stature and infertility.
More than 2,000 people received such treatment. Four developed CJD, the last case identified in 1991. All four cases were likely linked to a single contaminated batch.
The risks of any other cases of CJD developing now in pituitary material recipients, so long after the occurrence of the last identified case in Australia, are considered to be incredibly small.
Early-onset Alzheimer’s disease (defined as occurring before the age of 65) is uncommon, accounting for around 5% of all cases. Below the age of 50 it’s rare and likely to have a genetic contribution.
Early onset Alzheimer’s means it occurs before age 65.
perfectlab/ShutterstockThe risk is very low – and you can’t ‘catch’ it like a virus
The Nature Medicine paper identified five cases which were diagnosed in people aged 38 to 55. This is more than could be expected by chance, but still very low in comparison to the total number of patients treated worldwide.
Although the long “incubation period” of Alzheimer’s disease may mean more similar cases may be identified in the future, the absolute risk remains very low. The main scientific interest of the article lies in the fact it’s first to demonstrate that Alzheimer’s disease can be transmitted from person to person in a similar way to prion diseases, rather than in any public health risk.
The authors were keen to emphasise, as I will, that Alzheimer’s cannot be contracted via contact with or providing care to people with Alzheimer’s disease.
Steve Macfarlane, Head of Clinical Services, Dementia Support Australia, & Associate Professor of Psychiatry, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
The Mediterranean Diet Cookbook for Beginners – by Jessica Aledo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are a lot of Mediterranean Diet books on the market, and not all of them actually stick to the Mediterranean Diet. There’s a common mistake of thinking “Well, this dish is from the Mediterranean region, so…”, but that doesn’t make, for example, bacon-laden carbonara part of the Mediterranean Diet!
Jessica Aledo does better, and sticks unwaveringly to the Mediterranean Diet principles.
First, she gives a broad introduction, covering:
- The Mediterranean Diet pyramid
- Foods to eat on the Mediterranean Diet
- Foods to avoid on the Mediterranean Diet
- Benefits of the Mediterranean Diet
Then, it’s straight into the recipes, of which there are 201 (as with many recipe books, the title is a little misleading about this).
They’re divided into sections, thus:
- Breakfasts
- Lunches
- Snacks
- Dinners
- Desserts
The recipes are clear and simple, one per double-page, with high quality color illustrations. They give ingredients/directions/nutrients. There’s no padding!
Helpfully, she does include a shopping list as an appendix, which is really useful!
Bottom line: if you’re looking to build your Mediterranean Diet repertoire, this book is an excellent choice.
Get your copy of The Mediterranean Diet Cookbook for Beginners from Amazon today!
Share This Post
-
5 Steps To Beat Overwhelm
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dealing With Overwhelm
Whether we live a hectic life in general, or we usually casually take each day as it comes but sometimes several days gang up on us at once, everyone gets overwhelmed sometimes.
Today we’re going to look at how to deal with it healthily.
Step 1: Start anywhere
It’s easy to get stuck in “analysis paralysis” and not know how to tackle an unexpected large problem. An (unhealthy) alternative is to try to tackle everything at once, and end up doing nothing very well.
Even the most expert juggler will not successfully juggle 10 random things thrown unexpectedly at them.
So instead, just pick any part of the the mountain of to-dos, and start.
If you do want a little more finesse though, check out:
Procrastination, And How To Pay Off The To-Do List Debt
Step 2: Accept what you’re capable of
This one works both ways. It means being aware of your limitations yes, but also, of your actual abilities:
- Is the task ahead of you really beyond what you are capable of?
- Could you do it right now without hesitation if a loved one’s life depended on it?
- Could you do it, but there’s a price to pay (e.g. you can do it but it’ll wipe you out in some other life area)?
Work out what’s possible and acceptable to you, and make a decision. And remember, it could be that someone else could do it, but everyone has taken the “if you want something doing, give it to someone busy” approach. It’s flattering that people have such confidence in our competence, but it is also necessary to say “no” sometimes, or at least enlisting help.
Step 3: Listen to your body
…like a leader listening to an advisory council. Your perception of tiredness, pain, weakness, and all your emotions are simply messengers. Listen to the message! And then say “thank you for the information”, and proceed accordingly.
Sometimes that will be in the way the messengers seem to be hoping for!
Sometimes, however, maybe we (blessed with a weighty brain and not entirely a slave to our limbic system) know better, and know when it’s right to push through instead.
Similarly, that voice in your head? You get to decide where it goes and doesn’t. On which note…
Step 4: Be responsive, not reactive
We wrote previously on the difference between these:
A Bone To Pick… Up And Then Put Back Where We Found It
Measured responses will always be better than knee-jerk reactions, unless it is literally a case of a split-second making a difference. 99% of our problems in life are not so; usually the problem will still be there unchanged after a moment’s mindful consideration, so invest in that moment.
You’ve probably heard the saying “give me six hours to chop down a tree, and I’ll spend the first four sharpening the axe”. In this case, that can be your mind. Here’s a good starting point:
No-Frills, Evidence-Based Mindfulness
And if your mental state is already worse than that, mind racing with threats (real or perceived) and doom-laden scenarios, here’s how to get out of that negative spiral first, so that you can apply the rest of this:
Do remember to turn it on again afterwards, though
Step 5: Transcend discomfort
This is partly a callback to step 3, but it’s now coming from a place of a clear ready mind, so the territory should be looking quite different now. Nevertheless, it’s entirely possible that your clear view shows discomfort ahead.
You’re going to make a conscious decision whether or not to proceed through the discomfort (and if you’re not, then now’s the time to start calmly and measuredly looking at alternative plans; delegating, ditching, etc).
If you are going to proceed through discomfort, then it can help to frame the discomfort as simply a neutral part of the path to getting where you want. Maybe you’re going to be going way out of your comfort zone in order to deal with something, and if that’s the case, make your peace with it now, in advance.
“Certainly it hurts” / “Well, what’s the trick then?” / “The trick, William Potter, is not minding that it hurts”
(lines from a famous scene from the 1962 movie Lawrence of Arabia)
It’s ok to say to yourself (if it’s what you decide is the right thing to do) “Yep, this experience is going to suck terribly, but I’m going to do it anyway”.
See also (this being about Radical Acceptance):
What’s The Worst That Could Happen?
Take care!
Share This Post
Related Posts
-
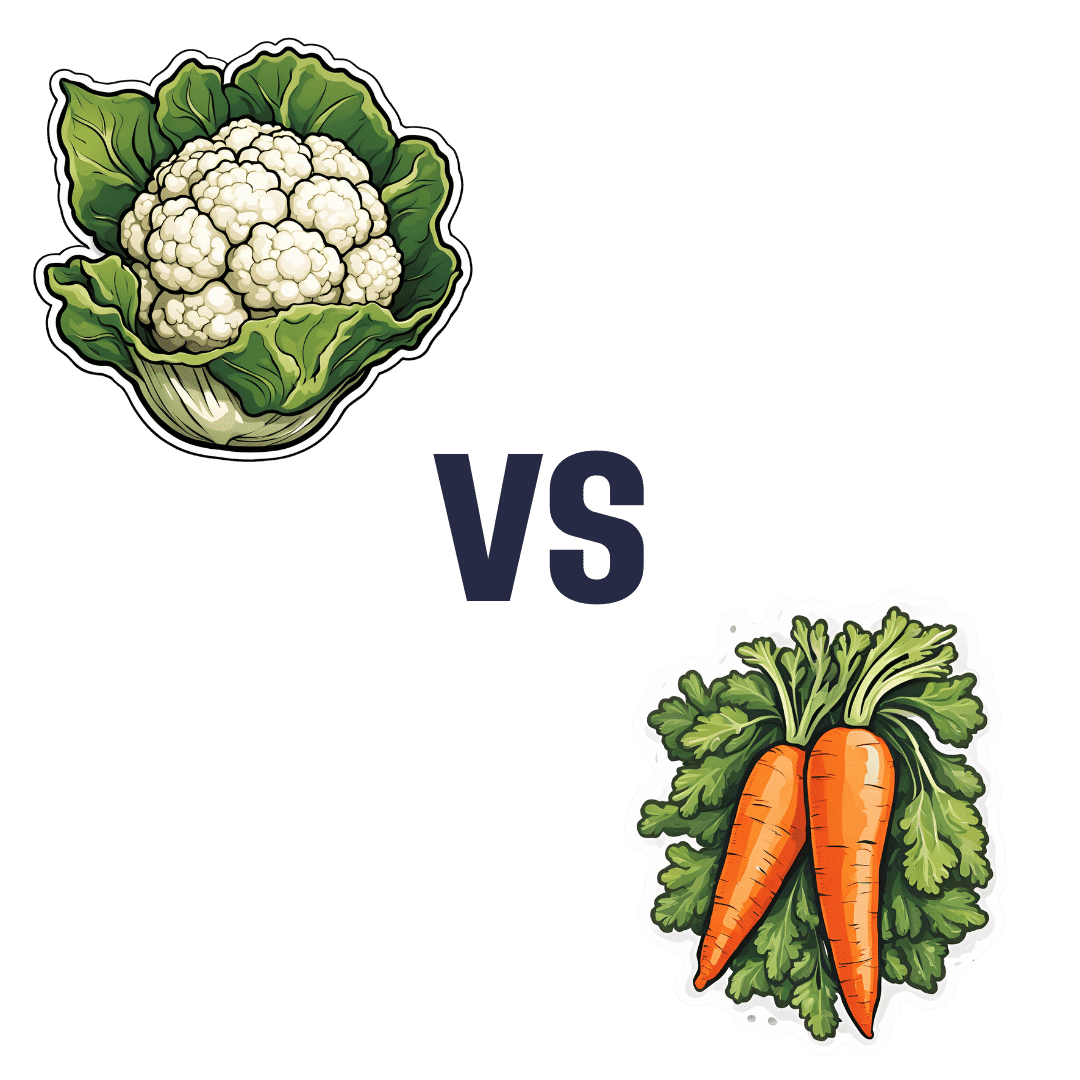
Cauliflower vs Carrot – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cauliflower to carrot, we picked the cauliflower.
Why?
In terms of macros, cauliflower has nearly 2x the protein while carrot has nearly 2x the carbs and slightly more fiber; we’re calling it a tie in this category.
When it comes to vitamins, cauliflower has more of vitamins B2, B5, B6, B9, C, K, and choline, while carrot has more of vitamins A, B1, B3, and E. Thus, a 7:4 win for cauliflower here.
In the category of minerals, cauliflower has more iron, magnesium, manganese, phosphorus, selenium, and zinc, while carrot has more calcium, copper, and potassium. So, a 6:3 win for cauliflower here.
In short, for overall nutritional density, adding up the sections makes for a clear win for cauliflower, but of course, enjoy either or (preferably) both; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Lifestyle vs Multiple Sclerosis & More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Saray Stancic. She’s another from the ranks of “doctors who got a serious illness and it completely changed how they view the treatment of serious illness”.
In her case, Stancic was diagnosed with multiple sclerosis, and wasn’t impressed with the results from the treatments offered, so (after 8 years of pain, suffering, and many medications, only for her condition to worsen) she set about doing better with an evidence-based lifestyle medicine approach.
After 7 years of her new approach, she would go on to successfully run a marathon and live symptom-free.
All this to say: her approach isn’t a magic quick fix, but it is a serious method for serious results, and after all, while it’d be nice to be magically in perfect health tomorrow, what’s important is being in good health for life, right?
If you’re interested in her impressive story, check out:
Doctor With Multiple Sclerosis On The Collapse Of US Healthcare
If you want to know what she did, then read on…
Six key lifestyle changes
Dr. Stancic credits her recovery to focus on the following evidence-based approaches:
The plant-centered plate
This is critical, and is the one she places most emphasis on. Most chronic diseases are exacerbated, if not outright caused, by chronic inflammation, and one cannot fix that without an anti-inflammatory diet.
An anti-inflammatory diet doesn’t have to be 100% plant-based, but broadly speaking, plants are almost always anti-inflammatory to a greater or lesser degree, while animal products are often pro-inflammatory—especially red meat and unfermented dairy.
For more details, see:
Anti-Inflammatory Diet 101 (What to Eat to Fight Inflammation)
Movement every day
While “exercise is good for you” is in principle not a shocker, remember that her starting point was being in terrible condition with badly flared-up MS.
Important to understand here is that excessive exercise can weaken the immune system and sometimes cause flare-ups of various chronic diseases.
Moving thoroughly and moving often, however, is best. So walking yes, absolutely, but also don’t neglect the rest of your body, do some gentle bodyweight squats (if you can; if you can’t, work up to them), stretch your arms as well as your legs, take all your joints through a full range of motion.
See also:
The Doctor Who Wants Us To Exercise Less, & Move More
Mindful stress management
Stress in life is unavoidable, but how we manage it is up to us. Bad things will continue to happen, great and small, but we can take a deep breath, remember that those things aren’t the boss of us, and deal with it calmly and conscientiously.
Mindfulness-Based Stress Reduction is of course the evidence-based “gold standard” for this, but whatever (not substance-based) method works for you, works for you!
About MBSR:
No-Frills, Evidence-Based Mindfulness
Good sleeping habits
Getting good sleep can be hard for anyone, let alone if you have chronic pain. However, Dr. Stancic advocates for doing whatever we can to get good sleep—which means not just duration (the famous “7–9 hours”), but also quality.
Learn more:
The 6 Dimensions Of Sleep (And Why They Matter)
Substance intake awareness
This one’s not so much of a “don’t do drugs, kids” as the heading makes it look. Dr. Stancic assumes we already know, for example, that smoking is bad for us in a long list of ways, and alcohol isn’t much better.
However, she also advises us that in our eagerness to do that plant-based diet, we would do better to go for whole foods plant-based, rather than the latest processed meat substitutes, for example.
And supplements? She bids us exercise caution, and to make sure to get good quality, as poor quality supplements can be worse than taking nothing (looking at you, cheap turmeric supplements that contain heavy metals).
And of course, that nutrients gained from diet will almost always be better than nutrients gained from supplements, as our body can usually use them better.
And see also, some commonly-made supplements mistakes:
Do You Know Which Supplements You Shouldn’t Take Together? (10 Pairs!)
Human connection
Lastly, we humans are a social species by evolution; as individuals, we may enjoy relatively more or less social contact, but having access to such is important not just for our mental health, but our physical health too—we will tend to deteriorate much more quickly when we have to deal with everything alone, all other things being equal.
It doesn’t mean you need a busy social life if that’s not in your nature, but it does mean it’s incredibly beneficial to have at least a small number of people that you trust and whose company you enjoy, at least relatively accessible to you (i.e., their life need not revolve around you, but they are the kind of people who will generally happily spend time with you and provide support when needed if they can).
As for how:
How To Beat Loneliness & Isolation
Want to know more from Dr. Stancic?
We recently reviewed this very good book of hers, which goes over each of these six things in much more detail than we have room for here:
What’s Missing from Medicine – by Dr. Saray Stancic
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Traveling To Die: The Latest Form of Medical Tourism
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the 18 months after Francine Milano was diagnosed with a recurrence of the ovarian cancer she thought she’d beaten 20 years ago, she traveled twice from her home in Pennsylvania to Vermont. She went not to ski, hike, or leaf-peep, but to arrange to die.
“I really wanted to take control over how I left this world,” said the 61-year-old who lives in Lancaster. “I decided that this was an option for me.”
Dying with medical assistance wasn’t an option when Milano learned in early 2023 that her disease was incurable. At that point, she would have had to travel to Switzerland — or live in the District of Columbia or one of the 10 states where medical aid in dying was legal.
But Vermont lifted its residency requirement in May 2023, followed by Oregon two months later. (Montana effectively allows aid in dying through a 2009 court decision, but that ruling doesn’t spell out rules around residency. And though New York and California recently considered legislation that would allow out-of-staters to secure aid in dying, neither provision passed.)
Despite the limited options and the challenges — such as finding doctors in a new state, figuring out where to die, and traveling when too sick to walk to the next room, let alone climb into a car — dozens have made the trek to the two states that have opened their doors to terminally ill nonresidents seeking aid in dying.
At least 26 people have traveled to Vermont to die, representing nearly 25% of the reported assisted deaths in the state from May 2023 through this June, according to the Vermont Department of Health. In Oregon, 23 out-of-state residents died using medical assistance in 2023, just over 6% of the state total, according to the Oregon Health Authority.
Oncologist Charles Blanke, whose clinic in Portland is devoted to end-of-life care, said he thinks that Oregon’s total is likely an undercount and he expects the numbers to grow. Over the past year, he said, he’s seen two to four out-of-state patients a week — about one-quarter of his practice — and fielded calls from across the U.S., including New York, the Carolinas, Florida, and “tons from Texas.” But just because patients are willing to travel doesn’t mean it’s easy or that they get their desired outcome.
“The law is pretty strict about what has to be done,” Blanke said.
As in other states that allow what some call physician-assisted death or assisted suicide, Oregon and Vermont require patients to be assessed by two doctors. Patients must have less than six months to live, be mentally and cognitively sound, and be physically able to ingest the drugs to end their lives. Charts and records must be reviewed in the state; neglecting to do so constitutes practicing medicine out of state, which violates medical licensing requirements. For the same reason, the patients must be in the state for the initial exam, when they request the drugs, and when they ingest them.
State legislatures impose those restrictions as safeguards — to balance the rights of patients seeking aid in dying with a legislative imperative not to pass laws that are harmful to anyone, said Peg Sandeen, CEO of the group Death With Dignity. Like many aid-in-dying advocates, however, she said such rules create undue burdens for people who are already suffering.
Diana Barnard, a Vermont palliative care physician, said some patients cannot even come for their appointments. “They end up being sick or not feeling like traveling, so there’s rescheduling involved,” she said. “It’s asking people to use a significant part of their energy to come here when they really deserve to have the option closer to home.”
Those opposed to aid in dying include religious groups that say taking a life is immoral, and medical practitioners who argue their job is to make people more comfortable at the end of life, not to end the life itself.
Anthropologist Anita Hannig, who interviewed dozens of terminally ill patients while researching her 2022 book, “The Day I Die: The Untold Story of Assisted Dying in America,” said she doesn’t expect federal legislation to settle the issue anytime soon. As the Supreme Court did with abortion in 2022, it ruled assisted dying to be a states’ rights issue in 1997.
During the 2023-24 legislative sessions, 19 states (including Milano’s home state of Pennsylvania) considered aid-in-dying legislation, according to the advocacy group Compassion & Choices. Delaware was the sole state to pass it, but the governor has yet to act on it.
Sandeen said that many states initially pass restrictive laws — requiring 21-day wait times and psychiatric evaluations, for instance — only to eventually repeal provisions that prove unduly onerous. That makes her optimistic that more states will eventually follow Vermont and Oregon, she said.
Milano would have preferred to travel to neighboring New Jersey, where aid in dying has been legal since 2019, but its residency requirement made that a nonstarter. And though Oregon has more providers than the largely rural state of Vermont, Milano opted for the nine-hour car ride to Burlington because it was less physically and financially draining than a cross-country trip.
The logistics were key because Milano knew she’d have to return. When she traveled to Vermont in May 2023 with her husband and her brother, she wasn’t near death. She figured that the next time she was in Vermont, it would be to request the medication. Then she’d have to wait 15 days to receive it.
The waiting period is standard to ensure that a person has what Barnard calls “thoughtful time to contemplate the decision,” although she said most have done that long before. Some states have shortened the period or, like Oregon, have a waiver option.
That waiting period can be hard on patients, on top of being away from their health care team, home, and family. Blanke said he has seen as many as 25 relatives attend the death of an Oregon resident, but out-of-staters usually bring only one person. And while finding a place to die can be a problem for Oregonians who are in care homes or hospitals that prohibit aid in dying, it’s especially challenging for nonresidents.
When Oregon lifted its residency requirement, Blanke advertised on Craigslist and used the results to compile a list of short-term accommodations, including Airbnbs, willing to allow patients to die there. Nonprofits in states with aid-in-dying laws also maintain such lists, Sandeen said.
Milano hasn’t gotten to the point where she needs to find a place to take the meds and end her life. In fact, because she had a relatively healthy year after her first trip to Vermont, she let her six-month approval period lapse.
In June, though, she headed back to open another six-month window. This time, she went with a girlfriend who has a camper van. They drove six hours to cross the state border, stopping at a playground and gift shop before sitting in a parking lot where Milano had a Zoom appointment with her doctors rather than driving three more hours to Burlington to meet in person.
“I don’t know if they do GPS tracking or IP address kind of stuff, but I would have been afraid not to be honest,” she said.
That’s not all that scares her. She worries she’ll be too sick to return to Vermont when she is ready to die. And, even if she can get there, she wonders whether she’ll have the courage to take the medication. About one-third of people approved for assisted death don’t follow through, Blanke said. For them, it’s often enough to know they have the meds — the control — to end their lives when they want.
Milano said she is grateful she has that power now while she’s still healthy enough to travel and enjoy life. “I just wish more people had the option,” she said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: