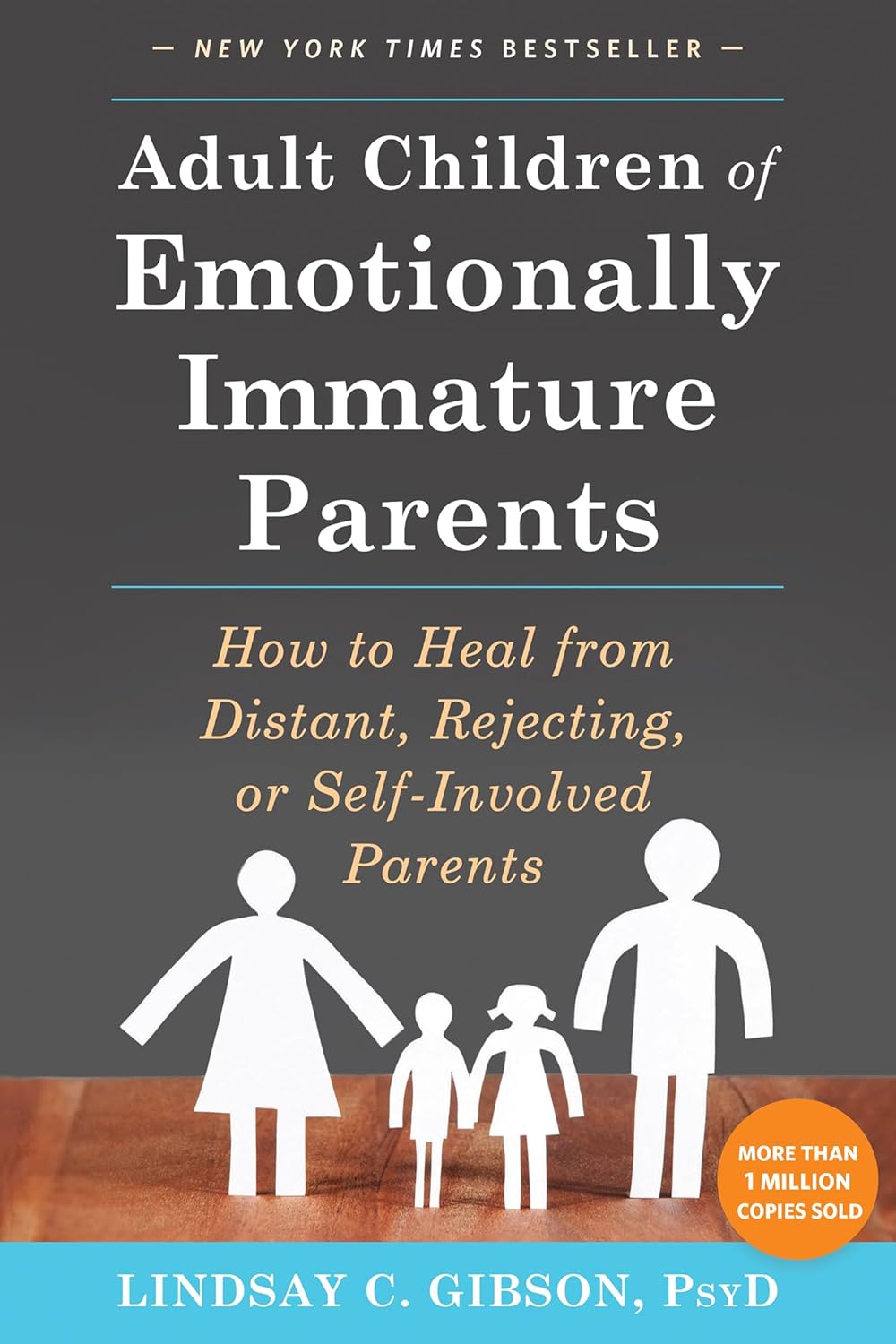
Adult Children of Emotionally Immature Parents – by Dr. Lindsay Gibson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not everyone had the best of parents, and the harm done can last well beyond childhood. This book looks at healing that.
Dr. Gibson talks about four main kinds of “difficult” parents, though of course they can overlap:
- The emotional parent, with their unpredictable outbursts
- The driven parent, with their projected perfectionism
- The passive parent, with their disinterest and unreliability
- The rejecting parent, with their unavailability and insults
For all of them, it’s common that nothing we could do was ever good enough, and that leaves a deep scar. To add to it, the unfavorable dynamic often persists in adult life, assuming everyone involved is still alive and in contact.
So, what to do about it? Dr. Gibson advocates for first getting a good understanding of what wasn’t right/normal/healthy, because it’s easy for a lot of us to normalize the only thing we’ve ever known. Then, beyond merely noting that no child deserved that lack of compassion, moving on to pick up the broken pieces one by one, and address each in turn.
The style of the book is anecdote-heavy (case studies, either anonymized or synthesized per common patterns) in a way that will probably be all-too-relatable to a lot of readers (assuming that if you buy this book, it’s for a reason), science-moderate (references peppered into the text; three pages of bibliography), and practicality-dense—that is to say, there are lots of clear usable examples, there are self-assessment questionnaires, there are worksheets for now making progress forward, and so forth.
Bottom line: if one or more of the parent types above strikes a chord with you, there’s a good chance you could benefit from this book.
Click here to check out Adult Children of Emotionally Immature Parents, and rebuild yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
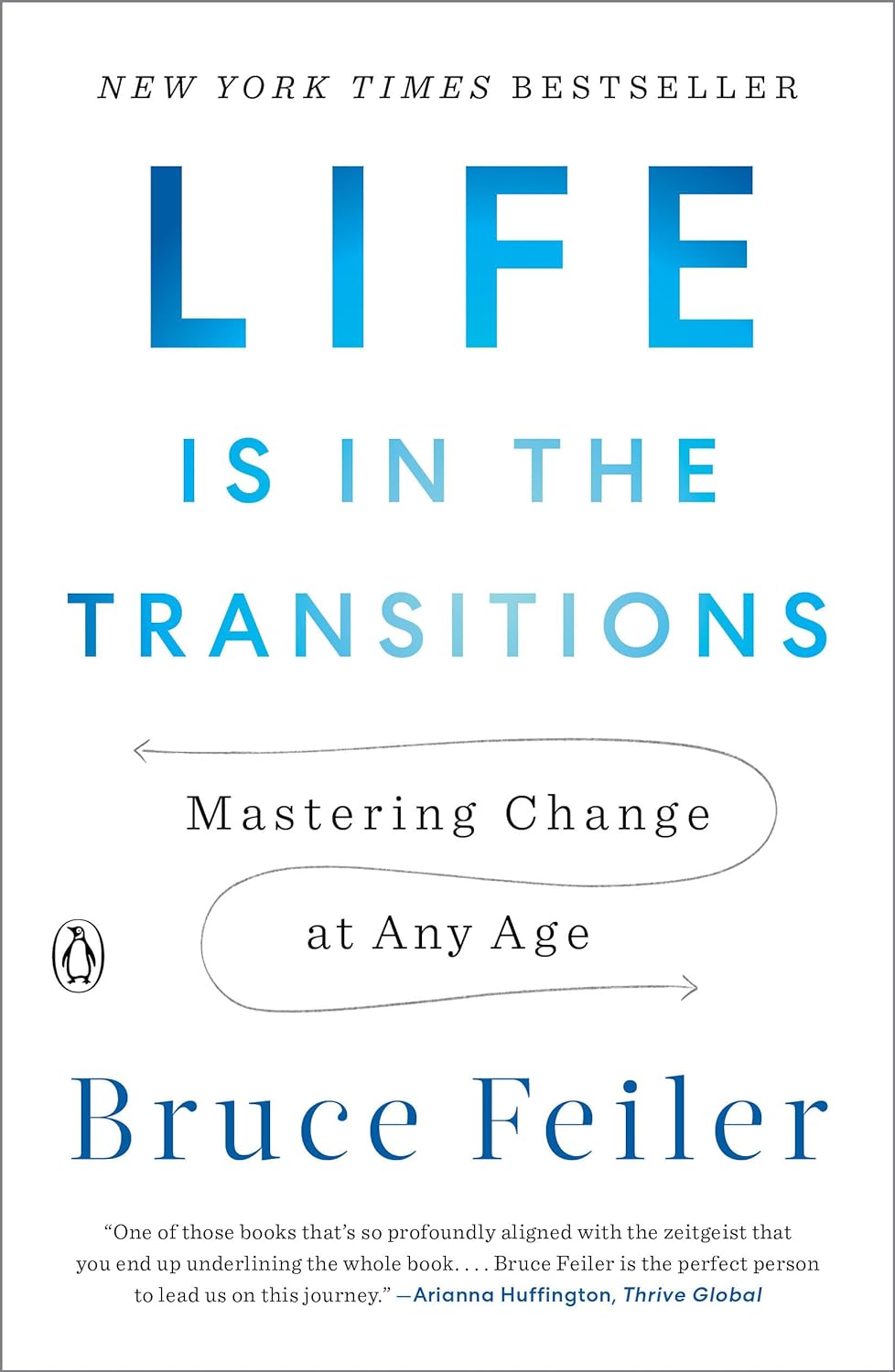
Life Is in the Transitions – by Bruce Feiler
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Change happens. Sometimes, because we choose it. More often, we don’t get a choice.
Our bodies change; with time, with illness, with accident or incident, or even, sometimes, with effort. People in our lives change; they come, they go, they get sick, they die. Our working lives change; we get a job, we lose a job, we change jobs, our jobs change, we retire.
Whether we’re undergoing cancer treatment or a religious conversion, whether our families are growing or down to the last few standing, change is inescapable.
Our author makes the case that on average, we each undergo at least 5 major “lifequakes”; changes that shake our lives to the core. Sometimes one will come along when we’ve barely got back on our feet from the previous—if we have at all.
What, then, to do about this? We can’t stop change from occurring, and some changes aren’t easy to “roll with”. Feiler isn’t prescriptive about this, but rather, descriptive:
By looking at the stories of hundreds of people he interviewed for this book, he looks at how people pivoted on the spot (or picked up the pieces!) and made the best of their situation—or didn’t.
Bottom line: zooming out like this, looking at many people’s lives, can remind us that while we don’t get to choose what winds we get swept by, we at least get to choose how we set the sails. The examples of others, as this book gives, can help us make better decisions.
Click here to check out Life Is In The Transitions, and get conscious about how you handle yours!
Share This Post
-
Gut Health and Anxiety
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I’d like to read articles on gut health and anxiety❞
We hope you caught yesterday’s edition of 10almonds, which touched on both of those! Other past editions you might like include:
We’ll be sure to include more going forward, too!
Share This Post
-
Healthy Habits for Managing & Reversing Prediabetes – by Dr. Marie Feldman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book doesn’t assume prior knowledge, and does explain the science of diabetes, prediabetes, the terms and the symptoms, what’s going on inside, etc—before getting onto the main meat of the book, the tips.
The promised 100 tips are varied in their application; they range from diet and exercise, to matters of sleep, stress, and even love.
There are bonus tips too! For example, an appendix covers “tips for healthier eating out” (i.e. in restaurants etc) and a grocery list to ensure your pantry is good for defending you against prediabetes.
The writing style is very accessible pop-science; this isn’t like reading some dry academic paper—though it does cite its sources for claims, which we always love to see.
Bottom line: if you’d like to proof yourself against prediabetes, and are looking for “small things that add up” habits to get into to achieve that, this book is an excellent first choice.
Share This Post
Related Posts
-
Trout vs Carp – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing trout to carp, we picked the trout.
Why?
Both have their strong points!
In terms of macros, trout has slightly more protein and fat, and/but also has less cholesterol than carp. So, we pick the trout in the macros category.
In the category of vitamins, trout has much more of vitamins A, B1, B2, B3, B5, B6, B7, B12, C, D, E, K, and choline, while carp has slightly more vitamin B9. In other words, an easy win for trout here.
When it comes to minerals, however, trout has more potassium and selenium, while carp has more calcium, copper, iron, magnesium, manganese, phosphorus, and zinc. A fair win for carp this time.
You may be wondering about heavy metals: this will vary depending on location, as well as the age of the fish (younger fish have had less time to accumulate heavy metals than old ones, so if you’re visiting the fishmonger, choose the smaller ones) and the lives they have led (e.g. wild vs farmed), however, as a general rule of thumb, trout will generally have lower heavy metals levels than carp, all other things (e.g. location, age, etc) being equal.
In short, enjoy either or both in moderation, but trout wins on 3/4 categories today.
Want to learn more?
You might like to read:
Farmed Fish vs Wild Caught: Antibiotics, Mercury, & More
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Basil vs Oregano – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing basil to oregano, we picked the basil.
Why?
You may be thinking: these are just herbs; we don’t eat enough of these for the nutritional values to be relevant!
And to this we say: there’s nothing stopping you :p Herbs are full of flavor and goodness and there is really no reason to deny yourself. On this note, check out the sabzi khordan (traditional Levantine herb platter), linked below. You’ll start thinking about herbs in new ways, and you can thank us later!
Now, in terms of macros, nominally basil has more protein and oregano has more carbs and fiber, but the numbers are so close in each case that we’re going to call this category a tie.
When it comes to vitamins, things get more interesting: basil has more of vitamins B2, B3, B6, B9, K, and choline, while oregano has more of vitamins A, B1, B5, C, and E. This means a 6:5 win for basil, but note how the two herbs together give an impressive vitamin coverage. In other words, they complement each other nutritionally, not just culinarily!
In the category of minerals, basil has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium and zinc, while oregano has more selenium. Now, this is obviously a clear win for basil, but we’d like to highlight that both of these herbs are incredibly rich in minerals (i.e. oregano is a very good source of all those minerals we listed for basil, too!); it’s just that basil has even more of most of them.
When looking at any nutrient-dense food (which most herbs are), it’s worth looking at polyphenols. In this case, both are very abundant in polyphenols, and/but their respective numbers are close enough to be within each other’s margin of variation (i.e. exact numbers will depend on the individual plant’s life history), so this category is a tie.
Adding up the sections makes for an overall clear win for basil, but absolutely please do enjoy both unless you have a good reason not to—they complement each other so well, in nutrients as well as in flavor!
Want to learn more?
You might like to read:
- Cilantro vs Parsley – Which is Healthier?
- Holy Basil: What Does (And Doesn’t) It Do?
- Invigorating Sabzi Khordan (A Traditional Levantine Platter Of Herbs & Accompaniments)
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ras El-Hanout
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a spice blend, and its name (رأس الحانوت) means “head of the shop”. It’s popular throughout Morocco, Algeria, and Tunisia, but can often be found elsewhere. The exact blend will vary a little from place to place and even from maker to maker, but the general idea is the same. The one we provide here today is very representative (and for an example of its use, see our Marrakesh Sorghum Salad recipe!).
Note: we’re giving all the quantities in whole tsp today, to make multiplying/dividing easier if you want to make more/less ras el-hanout.
You will need
- 6 tsp ground ginger
- 6 tsp ground coriander seeds
- 4 tsp ground turmeric
- 4 tsp ground sweet cinnamon
- 4 tsp ground cumin
- 2 tsp ground allspice ← not a spice mix! This is the name of a spice!
- 2 tsp ground cardamom
- 2 tsp ground anise
- 2 tsp ground black pepper
- 1 tsp ground cayenne pepper
- 1 tsp ground cloves
Note: you may notice that garlic and salt are conspicuous by their absence. The reason for this is that they are usually added separately per dish, if desired.
Method
1) Mix them thoroughly
That’s it! Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Our Top 5 Spices: How Much Is Enough For Benefits?
- A Tale Of Two Cinnamons ← this is important, to understand why it’s critical to use sweet cinnamon specifically
- Sweet Cinnamon vs Regular Cinnamon – Which is Healthier? ← not even exaggerating; one is health-giving and the other contains a compound that is toxic at 01.mg/kg; guess which one is easier to find in the US and Canada?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: