Life Is in the Transitions – by Bruce Feiler
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Change happens. Sometimes, because we choose it. More often, we don’t get a choice.
Our bodies change; with time, with illness, with accident or incident, or even, sometimes, with effort. People in our lives change; they come, they go, they get sick, they die. Our working lives change; we get a job, we lose a job, we change jobs, our jobs change, we retire.
Whether we’re undergoing cancer treatment or a religious conversion, whether our families are growing or down to the last few standing, change is inescapable.
Our author makes the case that on average, we each undergo at least 5 major “lifequakes”; changes that shake our lives to the core. Sometimes one will come along when we’ve barely got back on our feet from the previous—if we have at all.
What, then, to do about this? We can’t stop change from occurring, and some changes aren’t easy to “roll with”. Feiler isn’t prescriptive about this, but rather, descriptive:
By looking at the stories of hundreds of people he interviewed for this book, he looks at how people pivoted on the spot (or picked up the pieces!) and made the best of their situation—or didn’t.
Bottom line: zooming out like this, looking at many people’s lives, can remind us that while we don’t get to choose what winds we get swept by, we at least get to choose how we set the sails. The examples of others, as this book gives, can help us make better decisions.
Click here to check out Life Is In The Transitions, and get conscious about how you handle yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Sometimes, Perfect Isn’t Practical!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝10 AM breakfast is not realistic for most. What’s wrong with 8 AM and Evening me at 6. Don’t quite understand the differentiation.❞
(for reference, this is about our “Breakfasting For Health?” main feature)
It’s not terrible to do it the way you suggest It’s just not optimal, either, that’s all!
Breakfasting at 08:00 and then dining at 18:00 is ten hours apart, so no fasting benefits between those. Let’s say you take half an hour to eat dinner, then eat nothing again until breakfast, that’s 18:30 to 08:00, so that’s 13½ hours fasting. You’ll recall that fasting benefits start at 12 hours into the fast, so that means you’d only get 1½ hours of fasting benefits.
As for breakfasting at 08:00 regardless of intermittent fasting considerations, the reason for the conclusion of around 10:00 being optimal, is based on when our body is geared up to eat breakfast and get the most out of that, which the body can’t do immediately upon waking. So if you wake and get sunlight at 08:30, get a little moderate exercise, then by 10:00 your digestive system will be perfectly primed to get the most out of breakfast.
However! This is entirely based on you waking and getting sunlight at 08:30.
So, iff you wake and get sunlight at 06:30, then in that case, breakfasting at 08:00 would give the same benefits as described above. What’s important is the 1½ hour priming-time.
Writer’s note: our hope here is always to be informational, not prescriptive. Take what works for you; ignore what doesn’t fit your lifestyle.
I personally practice intermittent fasting for about 21hrs/day. I breakfast (often on nuts and perhaps a little salad) around 16:00, and dine at around 18:00ish, giving myself a little wiggleroom. I’m not religious about it and will slide it if necessary.
As you can see: that makes what is nominally my breakfast practically a pre-dinner snack, and I clearly ignore the “best to eat in the morning” rule because that’s not consistent with my desire to have a family dinner together in the evening while still practicing the level of fasting that I prefer.
Science is science, and that’s what we report here. How we apply it, however, is up to us all as individuals!
Enjoy!
Share This Post

How Science News Outlets Can Lie To You (Yes, Even If They Cite Studies!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Each Monday, we’re going to be bringing you cutting-edge research reviews to not only make your health and productivity crazy simple, but also, constantly up-to-date.
But today, in this special edition, we want to lay out plain and simple how to see through a lot of the tricks used not just by popular news outlets, but even sometimes the research publications themselves.
That way, when we give you health-related science news, you won’t have to take our word for it, because you’ll be able to see whether the studies we cite really support the claims we make.
Of course, we’ll always give you the best, most honest information we have… But the point is that you shouldn’t have to trust us! So, buckle in for today’s special edition, and never have to blindly believe sci-hub (or Snopes!) again.

The above now-famous Tumblr post that became a meme is a popular and obvious example of how statistics can be misleading, either by error or by deliberate spin.
But what sort of mistakes and misrepresentations are we most likely to find in real research?
Spin Bias
Perhaps most common in popular media reporting of science, the Spin Bias hinges on the fact that most people perceive numbers in a very “fuzzy logic” sort of way. Do you?
Try this:
- A million seconds is 11.5 days
- A billion seconds is not weeks, but 13.2 months!
…just kidding, it’s actually nearly thirty-two years.
Did the months figure seem reasonable to you, though? If so, this is the same kind of “human brains don’t do large numbers” problem that occurs when looking at statistics.
Let’s have a look at reporting on statistically unlikely side effects for vaccines, as an example:
- “966 people in the US died after receiving this vaccine!” (So many! So risky!)
- “Fewer than 3 people per million died after receiving this vaccine!” (Hmm, I wonder if it is worth it?)
- “Half of unvaccinated people with this disease die of it” (Oh)
How to check for this: ask yourself “is what’s being described as very common really very common?”. To keep with the spiders theme, there are many (usually outright made-up) stats thrown around on social media about how near the nearest spider is at any given time. Apply this kind of thinking to medical conditions.. If something affects only 1% of the population (So few! What a tiny number!), how far would you have to go to find someone with that condition? The end of your street, perhaps?
Selection/Sampling Bias
Diabetes disproportionately affects black people, but diabetes research disproportionately focuses on white people with diabetes. There are many possible reasons for this, the most obvious being systemic/institutional racism. For example, advertisements for clinical trial volunteer opportunities might appear more frequently amongst a convenient, nearby, mostly-white student body. The selection bias, therefore, made the study much less reliable.
Alternatively: a researcher is conducting a study on depression, and advertises for research subjects. He struggles to get a large enough sample size, because depressed people are less likely to respond, but eventually gets enough. Little does he know, even the most depressed of his subjects are relatively happy and healthy compared with the silent majority of depressed people who didn’t respond.

See This And Many More Educational Cartoons At Sketchplanations.com!
How to check for this: Does the “method” section of the scientific article describe how they took pains to make sure their sample was representative of the relevant population, and how did they decide what the relevant population was?
Publication Bias
Scientific publications will tend to prioritise statistical significance. Which seems great, right? We want statistically significant studies… don’t we?
We do, but: usually, in science, we consider something “statistically significant” when it hits the magical marker of p=0.05 (in other words, the probability of getting that result is 1/20, and the results are reliably coming back on the right side of that marker).
However, this can result in the clinic stopping testing once p=0.05 is reached, because they want to have their paper published. (“Yay, we’ve reached out magical marker and now our paper will be published”)
So, you can think of publication bias as the tendency for researchers to publish ‘positive’ results.
If it weren’t for publication bias, we would have a lot more studies that say “we tested this, and here are our results, which didn’t help answer our question at all”—which would be bad for the publication, but good for science, because data is data.
To put it in non-numerical terms: this is the same misrepresentation as the technically true phrase “when I misplace something, it’s always in the last place I look for it”—obviously it is, because that’s when you stop looking.
There’s not a good way to check for this, but be sure to check out sample sizes and see that they’re reassuringly large.
Reporting/Detection/Survivorship Bias
There’s a famous example of the rise in “popularity” of left-handedness. Whilst Americans born in ~1910 had a bit under a 3.5% chance of being left handed, those born in ~1950 had a bit under a 12% change.
Why did left-handedness become so much more prevalent all of a sudden, and then plateau at 12%?
Simple, that’s when schools stopped forcing left-handed children to use their right hands instead.
In a similar fashion, countries have generally found that homosexuality became a lot more common once decriminalized. Of course the real incidence almost certainly did not change—it just became more visible to research.
So, these biases are caused when the method of data collection and/or measurement leads to a systematic error in results.
How to check for this: you’ll need to think this through logically, on a case by case basis. Is there a reason that we might not be seeing or hearing from a certain demographic?
And perhaps most common of all…
Confounding Bias
This is the bias that relates to the well-known idea “correlation ≠ causation”.
Everyone has heard the funny examples, such as “ice cream sales cause shark attacks” (in reality, both are more likely to happen in similar places and times; when many people are at the beach, for instance).
How can any research paper possibly screw this one up?
Often they don’t and it’s a case of Spin Bias (see above), but examples that are not so obviously wrong “by common sense” often fly under the radar:
“Horse-riding found to be the sport that most extends longevity”
Should we all take up horse-riding to increase our lifespans? Probably not; the reality is that people who can afford horses can probably afford better than average healthcare, and lead easier, less stressful lives overall. The fact that people with horses typically have wealthier lifestyles than those without, is the confounding variable here.

See This And Many More Educational Cartoons on XKCD.com!
In short, when you look at the scientific research papers cited in the articles you read (you do look at the studies, yes?), watch out for these biases that found their way into the research, and you’ll be able to draw your own conclusions, with well-informed confidence, about what the study actually tells us.
Science shouldn’t be gatekept, and definitely shouldn’t be abused, so the more people who know about these things, the better!
So…would one of your friends benefit from this knowledge? Forward it to them!
Share This Post

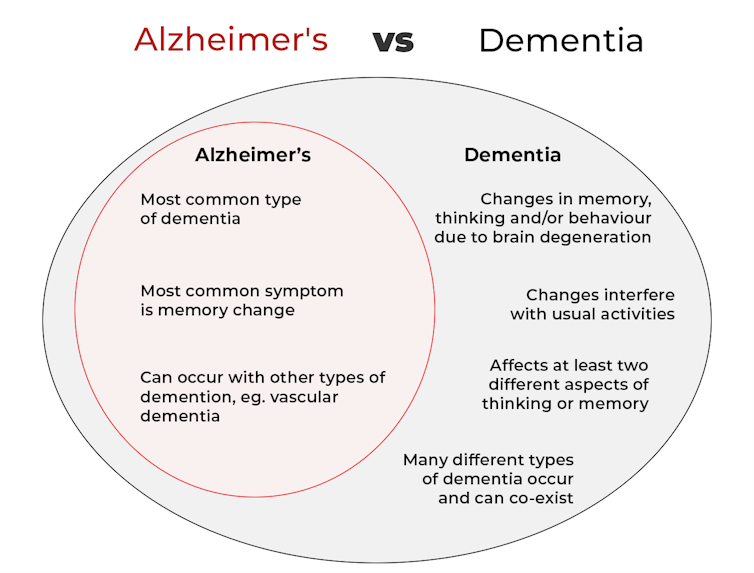
What’s the difference between Alzheimer’s and dementia?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
Changes in thinking and memory as we age can occur for a variety of reasons. These changes are not always cause for concern. But when they begin to disrupt daily life, it could indicate the first signs of dementia.
Another term that can crop up when we’re talking about dementia is Alzheimer’s disease, or Alzheimer’s for short.
So what’s the difference?

Lightspring/Shutterstock What is dementia?
Dementia is an umbrella term used to describe a range of syndromes that result in changes in memory, thinking and/or behaviour due to degeneration in the brain.
To meet the criteria for dementia these changes must be sufficiently pronounced to interfere with usual activities and are present in at least two different aspects of thinking or memory.
For example, someone might have trouble remembering to pay bills and become lost in previously familiar areas.
It’s less-well known that dementia can also occur in children. This is due to progressive brain damage associated with more than 100 rare genetic disorders. This can result in similar cognitive changes as we see in adults.
So what’s Alzheimer’s then?
Alzheimer’s is the most common type of dementia, accounting for about 60-80% of cases.
So it’s not surprising many people use the terms dementia and Alzheimer’s interchangeably.
Changes in memory are the most common sign of Alzheimer’s and it’s what the public most often associates with it. For instance, someone with Alzheimer’s may have trouble recalling recent events or keeping track of what day or month it is.

People with dementia may have trouble keeping track of dates. Daisy Daisy/Shutterstock We still don’t know exactly what causes Alzheimer’s. However, we do know it is associated with a build-up in the brain of two types of protein called amyloid-β and tau.
While we all have some amyloid-β, when too much builds up in the brain it clumps together, forming plaques in the spaces between cells. These plaques cause damage (inflammation) to surrounding brain cells and leads to disruption in tau. Tau forms part of the structure of brain cells but in Alzheimer’s tau proteins become “tangled”. This is toxic to the cells, causing them to die. A feedback loop is then thought to occur, triggering production of more amyloid-β and more abnormal tau, perpetuating damage to brain cells.
Alzheimer’s can also occur with other forms of dementia, such as vascular dementia. This combination is the most common example of a mixed dementia.

Vascular dementia
The second most common type of dementia is vascular dementia. This results from disrupted blood flow to the brain.
Because the changes in blood flow can occur throughout the brain, signs of vascular dementia can be more varied than the memory changes typically seen in Alzheimer’s.
For example, vascular dementia may present as general confusion, slowed thinking, or difficulty organising thoughts and actions.
Your risk of vascular dementia is greater if you have heart disease or high blood pressure.
Frontotemporal dementia
Some people may not realise that dementia can also affect behaviour and/or language. We see this in different forms of frontotemporal dementia.
The behavioural variant of frontotemporal dementia is the second most common form (after Alzheimer’s disease) of younger onset dementia (dementia in people under 65).
People living with this may have difficulties in interpreting and appropriately responding to social situations. For example, they may make uncharacteristically rude or offensive comments or invade people’s personal space.
Semantic dementia is also a type of frontotemporal dementia and results in difficulty with understanding the meaning of words and naming everyday objects.
Dementia with Lewy bodies
Dementia with Lewy bodies results from dysregulation of a different type of protein known as α-synuclein. We often see this in people with Parkinson’s disease.
So people with this type of dementia may have altered movement, such as a stooped posture, shuffling walk, and changes in handwriting. Other symptoms include changes in alertness, visual hallucinations and significant disruption to sleep.
Do I have dementia and if so, which type?
If you or someone close to you is concerned, the first thing to do is to speak to your GP. They will likely ask you some questions about your medical history and what changes you have noticed.
Sometimes it might not be clear if you have dementia when you first speak to your doctor. They may suggest you watch for changes or they may refer you to a specialist for further tests.
There is no single test to clearly show if you have dementia, or the type of dementia. A diagnosis comes after multiple tests, including brain scans, tests of memory and thinking, and consideration of how these changes impact your daily life.
Not knowing what is happening can be a challenging time so it is important to speak to someone about how you are feeling or to reach out to support services.
Dementia is diverse
As well as the different forms of dementia, everyone experiences dementia in different ways. For example, the speed dementia progresses varies a lot from person to person. Some people will continue to live well with dementia for some time while others may decline more quickly.
There is still significant stigma surrounding dementia. So by learning more about the various types of dementia and understanding differences in how dementia progresses we can all do our part to create a more dementia-friendly community.
The National Dementia Helpline (1800 100 500) provides information and support for people living with dementia and their carers. To learn more about dementia, you can take this free online course.
Nikki-Anne Wilson, Postdoctoral Research Fellow, Neuroscience Research Australia (NeuRA), UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts

16/8 Intermittent Fasting For Beginners
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Health Insider explains in super-simple fashion why and how to do Intermittent Fasting (IF), which is something that can sound complicated at first, but becomes very simple and easy once understood.
What do we need to know?
Intermittent fasting (IF) is a good, well-evidenced way to ease your body’s metabolic load, and
give your organs a chance to recover from the strain of digestion and its effects. That’s not just your gastrointestinal organs! It’s your pancreas and liver too, amongst others—this is about glucose metabolism as much as it is about digestion.This, in turn, allows your body some downtime to do its favorite thing, which is: maintenance!
This maintenance takes the form of enhanced cellular apoptosis and autophagy, helping to keep cells young and cancer-free.
In other words, with well-practised intermittent fasting, we can reduce our risk of metabolic disease (including heart disease and diabetes) as well as cancer and neurodegeneration.
You may be wondering: this sounds miraculous; what’s the catch? There are a couple:
- While fasting from food, the body’s enhanced metabolism requires more water, so you’ll need to take extra care keep on top of your hydration (this is one reason why Ramadan fasting, while healthy for most people, is not as healthy as IF—because Ramadan fasting means abstaining from water, too).
- If you are diabetic, and especially if you have Type 1 Diabetes, fasting may not be a safe option for you, since if you get a hypo in the middle of your fasting period, it’s obviously not a good idea to wait another many hours before fixing it.
Extra note on that last one: it’s easy to think “can’t I just lower my bolus insulin instead of eating?” and while superficially yes that will raise your blood sugar levels, it’s because the sugar will be sticking around in your blood, and not actually getting released into the organs that need it. So while your blood glucose monitor may say you’re fine, you will be starving your organs and if you keep it up they may suffer serious damage.
Disclaimer: our standard legal/medical disclaimer applies, and this is intended for educational purposes only; please do speak with your endocrinologist before changing anything you usually do with regard to your blood sugar maintenance.
Ok, back onto the cheerier topic at hand:
Aside from the above: for most people, IF is a remarkably healthful practice in very many ways.
For more on the science, practicalities, and things to do/avoid, enjoy this short (4:53) video:
Click Here If The Embedded Video Doesn’t Load Automatically
Want to know more?
Check out our previous main feature on this topic:
Intermittent Fasting: Mythbusting Edition
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

What Happened to You? – by Dr. Bruce Perry and Oprah Winfrey
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The very title “What Happened To You?” starts with an assumption that the reader has suffered trauma. This is not just a sample bias of “a person who picks up a book about healing from trauma has probably suffered trauma”, but is also a statistically safe assumption. Around 60% of adults report having suffered some kind of serious trauma.
The authors examine, as the subtitle suggests, these matters in three parts:
- Trauma
- Resilience
- Healing
Trauma can take many forms; sometimes it is a very obvious dramatic traumatic event; sometimes less so. Sometimes it can be a mountain of small things that eroded our strength leaving us broken. But what then, of resilience?
Resilience (in psychology, anyway) is not imperviousness; it is the ability to suffer and recover from things.
Healing is the tail-end part of that. When we have undergone trauma, displayed whatever amount of resilience we could at the time, and now have outgrown our coping strategies and looking to genuinely heal.
The authors present many personal stories and case studies to illustrate different kinds of trauma and resilience, and then go on to outline what we can do to grow from there.
Bottom line: if you or a loved one has suffered trauma, this book may help a lot in understanding and processing that, and finding a way forwards from it.
Click here to check out “What Happened To You?” and give yourself what you deserve.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Spark – by Dr. John Ratey
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We all know that exercise is good for mental health as well as physical. So, what’s so revolutionary about this “revolutionary new science of exercise and the brain”?
A lot of it has to do with the specific neuroscience of how exercise has not only a mood-boosting effect (endorphins) and neuroprotective effect (helping to guard against cognitive decline), but also promotes neuroplasticity… e.g., the creation and strengthening of neural pathways, as well as boosting the structure of the brain in some parts such as the cerebellum.
The book also covers not just “exercise has these benefits”, but also the “how this works” of all kinds of brain benefits, including:
- against Alzheimer’s
- mitigating ADHD
- managing menopause
- dealing with addiction
…and more. And once we understand how something works, we’re far more likely to be motivated to actually do the kinds of exercises that give the specific benefits we want/need. Which is very much the important part!
In short: this book will tell you what you need to know to get you doing the exercises you need to enjoy those benefits—very much worth it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: