‘Noisy’ autistic brains seem better at certain tasks. Here’s why neuroaffirmative research matters
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pratik Raul, University of Canberra; Jeroen van Boxtel, University of Canberra, and Jovana Acevska, University of Canberra
Autism is a neurodevelopmental difference associated with specific experiences and characteristics.
For decades, autism research has focused on behavioural, cognitive, social and communication difficulties. These studies highlighted how autistic people face issues with everyday tasks that allistic (meaning non-autistic) people do not. Some difficulties may include recognising emotions or social cues.
But some research, including our own study, has explored specific advantages in autism. Studies have shown that in some cognitive tasks, autistic people perform better than allistic people. Autistic people may have greater success in identifying a simple shape embedded within a more complex design, arranging blocks of different shapes and colours, or spotting an object within a cluttered visual environment (similar to Where’s Wally?). Such enhanced performance has been recorded in babies as young as nine months who show emerging signs of autism.
How and why do autistic individuals do so well on these tasks? The answer may be surprising: more “neural noise”.
What is neural noise?
Generally, when you think of noise, you probably think of auditory noise, the ups and downs in the amplitude of sound frequencies we hear.
A similar thing happens in the brain with random fluctuations in neural activity. This is called neural noise.
This noise is always present, and comes on top of any brain activity caused by things we see, hear, smell and touch. This means that in the brain, an identical stimulus that is presented multiple times won’t cause exactly the same activity. Sometimes the brain is more active, sometimes less. In fact, even the response to a single stimulus or event will fluctuate continuously.
Neural noise in autism
There are many sources of neural noise in the brain. These include how the neurons become excited and calm again, changes in attention and arousal levels, and biochemical processes at the cellular level, among others. An allistic brain has mechanisms to manage and use this noise. For instance, cells in the hippocampus (the brain’s memory system) can make use of neural noise to enhance memory encoding and recall.
Evidence for high neural noise in autism can be seen in electroencephalography (EEG) recordings, where increased levels of neural fluctuations were observed in autistic children. This means their neural activity is less predictable, showing a wider range of activity (higher ups and downs) in response to the same stimulus.
In simple terms, if we imagine the EEG responses like a sound wave, we would expect to see small ups and downs (amplitude) in allistic brains each time they encounter a stimulus. But autistic brains seem to show bigger ups and downs, demonstrating greater amplitude of neural noise.
Many studies have linked this noisy autistic brain with cognitive, social and behavioural difficulties.
But could noise be a bonus?
The diagnosis of autism has a long clinical history. A shift from the medical to a more social model has also seen advocacy for it to be reframed as a difference, rather than a disorder or deficit. This change has also entered autism research. Neuroaffirming research can examine the uniqueness and strengths of neurodivergence.
Psychology and perception researcher David Simmons and colleagues at the University of Glasgow were the first to suggest that while high neural noise is generally a disadvantage in autism, it can sometimes provide benefits due to a phenomenon called stochastic resonance. This is where optimal amounts of noise can enhance performance. In line with this theory, high neural noise in the autistic brain might enhance performance for some cognitive tasks.
Our 2023 research explores this idea. We recruited participants from the general population and investigated their performance on letter-detection tasks. At the same time, we measured their level of autistic traits.
We performed two letter-detection experiments (one in a lab and one online) where participants had to identify a letter when displayed among background visual static of various intensities.
By using the static, we added additional visual noise to the neural noise already present in our participants’ brains. We hypothesised the visual noise would push participants with low internal brain noise (or low autistic traits) to perform better (as suggested by previous research on stochastic resonance). The more interesting prediction was that noise would not help individuals who already had a lot of brain noise (that is, those with high autistic traits), because their own neural noise already ensured optimal performance.
Indeed, one of our experiments showed people with high neural noise (high autistic traits) did not benefit from additional noise. Moreover, they showed superior performance (greater accuracy) relative to people with low neural noise when the added visual static was low. This suggests their own neural noise already caused a natural stochastic resonance effect, resulting in better performance.
It is important to note we did not include clinically diagnosed autistic participants, but overall, we showed the theory of enhanced performance due to stochastic resonance in autism has merits.
Why this is important?
Autistic people face ignorance, prejudice and discrimination that can harm wellbeing. Poor mental and physical health, reduced social connections and increased “camouflaging” of autistic traits are some of the negative impacts that autistic people face.
So, research underlining and investigating the strengths inherent in autism can help reduce stigma, allow autistic people to be themselves and acknowledge autistic people do not require “fixing”.
The autistic brain is different. It comes with limitations, but it also has its strengths.
Pratik Raul, PhD candidiate, University of Canberra; Jeroen van Boxtel, Associate professor, University of Canberra, and Jovana Acevska, Honours Graduate Student, University of Canberra
This article is republished from The Conversation under a Creative Commons license. Read the original article.

Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Much Weight Gain Do Antidepressants Cause?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s a lot of talk in the news lately about antidepressants and weight gain, so let’s look at some numbers.
Here’s a study from July 2024 that compared the weight gain of eight popular antidepressants, and pop-science outlets have reported it with such snippets as:
❝Bupropion users were approximately 15–20% less likely to gain a clinically significant amount of weight than those taking the most common medication, sertraline.
The researchers considered weight gain of 5% or more as clinically significant.❞
Read in full: Study compares weight gain across eight common antidepressants
At this point, you might (especially if you or a loved one is on sertraline) be grabbing a calculator and seeing what 5% of your weight is, and might be concerned at the implications.
However, this is a little like if, in our This or That section, we were to report that food A has 17x more potassium than food B, without mentioning that food A has 0.01mg/100g and food A has 0.17mg/100g, and thus that, while technically “17x more”, the difference is trivial.
As a quick aside: we do, by the way, try to note when things like that might skew the stats and either wipe them out by not mentioning that they contain potassium at all (as they barely do), or if it’s a bit more, describing them as being “approximately equal in potassium” or else draw attention to the “but the amounts are trivial in both cases”.
Back to the antidepressants: in fact, for those two antidepressants compared in that snippet, the truth is (when we go looking in the actual research paper and the data within):
- sertraline was associated with an average weight change of +1.5kg (just over 3lb) over the course of 24 months
- bupropion was associated with an average weight change of +0.5kg (just under 1lb) over the course of 24 months
Sertraline being the most weight-gain-inducing of the 8 drugs compared, and bupropion being the least, this means (with them both having fairly even curves):
- sertraline being associated with an average weight change of 0.06kg (about 2oz) per month
- bupropion being associated with an average weight change of 0.02kg (less than 1oz) per month
For all eight, see the chart here in the paper itself:
Medication-Induced Weight Change Across Common Antidepressant Treatments ← we’ve made the link go straight to the chart, for your convenience, but you can also read the whole paper there
While you’re there, you might also see that for some antidepressants, such as duloxetine, fluoxetine, and venlafaxine, there’s an initial weight gain, but then it clearly hits a plateau and weight ceases to change after a certain point, which is worth considering too, since “you’ll gain a little bit of weight and then stay at that weight” is a very different prognosis from “you’ll gain a bit of weight and keep gaining it forever until you die”.
But then again, consider this:
Most adults will gain half a kilo this year – and every year. Here’s how to stop “weight creep”
That’s more weight gain than one gets on sertraline, the most weight-gain-inducing antidepressant tested!
What about over longer-term use?
Here’s a more recent study (December 2024) that looked at antidepressant use over 6 years, and found an average 2% weight gain over those 6 years, but it didn’t break it down by antidepressant type, sadly:
…which seems like quite a wasted opportunity, since some of the medications considered are very different, working on completely different systems (for example, SSRIs vs NDRIs, working on serotonin or norepinephrine+dopamine, respectively—see our Neurotransmitter Cheatsheet for more about those) and having often quite different side effects. Nevertheless, the study (despite collecting this information) didn’t then tabulate the data, and instead considered them all to be the same factor, “antidepressants”.
What this study did do that was useful was included a control group not on antidepressants so we know that on average:
- never-users of antidepressants gained an average of 1% of their bodyweight over those 6 years
- users-and-desisters of antidepressants gained an average of 1.8% of their bodyweight over those 6 years*
- continuing users of antidepressants gained an average of 2% of their bodyweight over those 6 years
*for this group, weight gain was a commonly cited reason for stopping taking the antidepressants in question
Writer’s anecdote: I’ve been on mirtazapine (a presynaptic alpha2-adrenoreceptor antagonist which increases central noradrenergic and serotonergic neurotransmission) for some years and can only say that I wish I’d been on it decades previously. I requested mirtazapine specifically, because I’m me and I know my stuff and considered it would most likely be by far the best fit for me out of the options available. Starting at a low dose, the only meaningful side effect was mild sedation (expected, and associated only with low-dose use); increasing after a couple of weeks to a moderate dose, that side effect disappeared and now the only remaining side effect is a slight dryness of the mouth, which is fine, as it ensures I remember to stay hydrated 🙂 anyway, my weight hasn’t changed (beyond very small temporary fluctuations) in the time I’ve been on mirtazapine. Disclaimer: the plural of anecdote is not data, and I can only speak for my own experience, and am not making any particular recommendation here. Your personal physiology will be different from mine, and may respond well or badly to any given treatment according to your own physiology.
Further considerations
This is touched on in the “Discussion” section of the latter paper (so do check that out if you want all the details, more than we can reasonably put here), but there are other factors to consider, for example:
- whether people were underweight/healthy weight/overweight at baseline (sometimes, a weight gain can be a good thing, recovering from an illness, and in the case of the illness that is depression, weight can swing either way)
- antidepressants changing eating and exercise habits (generally speaking: more likely to eat more and exercise more)
- body composition! How did they not cover this (neither paper did)?! Muscle weighs more than fat, and improvements in exercise can result in an increase in muscle and thus an increase in overall weight.
As researchers like to say, “this highlights the need for more high-quality studies to look into…” (and then the various things that went unexamined).
Want to know more?
Check out our previous main feature:
Antidepressants: Personalization Is Key!
Take care!
Share This Post
-
Staying Healthy and Active After 60
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Questions and Answers at 10almonds
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Q: How to be your best self after 60: Self motivation / Avoiding or limiting salt, sugar & alcohol: Alternatives / Ways to sneak in more movements/exercise
…and, from a different subscriber…
Q: Inflammation & over 60 weight loss. Thanks!
Here are some of our greatest hits on those topics:
- Where Nutrition Meets Habits ← focusing on food that’s all three of: healthy + easy + cheap
- How To Keep On Keeping On ← exercise tips for when the motivation wanes
- Keep Inflammation At Bay ← science-based tips and advice
Also, while we’ve recommended a couple of books on stopping (or reducing) drinking, we’ve not done a main feature on that, so we definitely will one of these days!
Share This Post
-
The End of Old Age – by Dr. Marc Agronin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this book is not: a book about ending aging. For that, you would want to check out “Ending Aging”, by Dr. Aubrey de Grey.
What this book actually is: a book about the purpose of aging. As in: “aging: to what end?”, and then the book answers that question.
Rather than viewing aging as solely a source of decline, this book (while not shying away from that) resolutely examines the benefits of old age—from clinically defining wisdom, to exploring the many neurological trade-offs (e.g., “we lose this thing but we get this other thing in the process”), and the assorted ways in which changes in our brain change our role in society, without relegating us to uselessness—far from it!
The style of the book is deep and meaningful prose throughout. Notwithstanding the author’s academic credentials and professional background in geriatric psychiatry, there’s no hard science here, just comprehensible explanations of psychiatry built into discussions that are often quite philosophical in nature (indeed, the author additionally has a degree in psychology and philosophy, and it shows).
Bottom line: if you’d like your own aging to be something you understand better and can actively work with rather than just having it happen to you, then this is an excellent book for you.
Share This Post
Related Posts
-
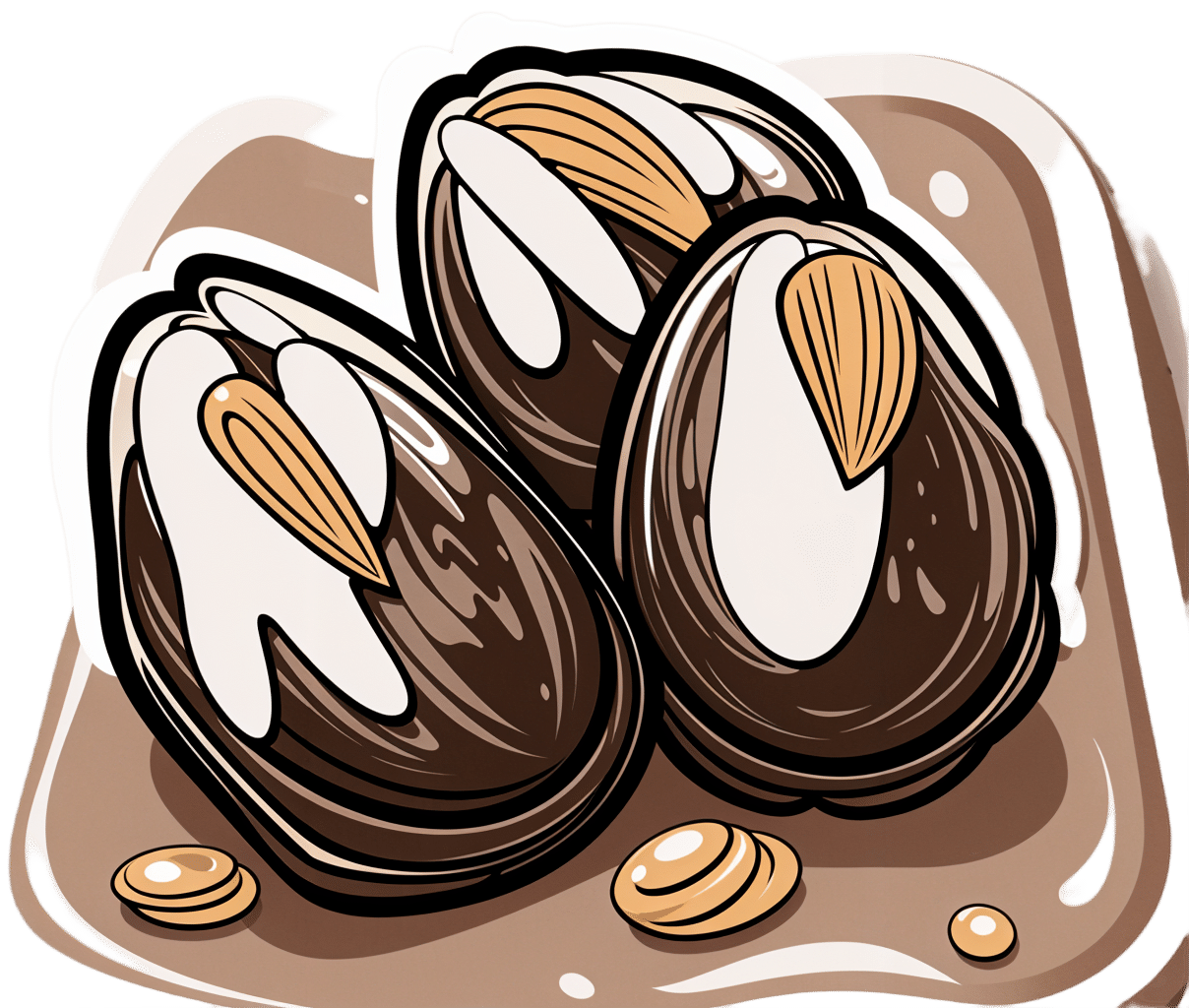
Tiramisu Crunch Bites
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s coffee, it’s creamy, it’s nutty, it’s chocolatey, what’s not to love? It has all the well-loved flavors of tiramisu, but this recipe is a simple one, and it’s essentially stuffed dates in a way you’ve never had them before. They’re delectable, decadent, and decidedly good for your health. These things are little nutrient-bombs that’ll keep you reaching for more.
You will need
- Coffee (we will discuss this)
- 150g (5.5oz) mascarpone (if vegan or lactose-intolerant, can be substituted with vegan varieties, or at a pinch, pressed silken tofu)
- 500g (1lb) dates (Medjool are ideal)
- Twice as many almonds as you have dates
- 50g (2oz) dark chocolate (the darkest, bitterest, you can find)
- Edible flower petals if you can source them (some shops sell dried rose petals for this purpose)
Method
(we suggest you read everything at least once before doing anything)
1) Take the mascarpone and whisk (or blend) it with the coffee. What kind of coffee, you ask? Many will use instant coffee (1tbsp granules mixed with enough boiling water to dissolve it), and that is actually healthiest (counterintuitive but true) but if you care for flavor over health, and have the means to make espresso, make it ristretto (so, stop it halfway through filling up an espresso cup), let it cool, and use that. Absolute bonus for flavor (not for health): if you have the means to make Turkish coffee, use an equivalent amount of that (again, cooled).
You will now have coffee-flavoured mascarpone. It’s great for your gut and full of antioxidant polyphenols. Set it aside for the moment.
2) Take the dark chocolate and melt it. Please don’t microwave it or try to do it in a pan directly over the hob; instead, you will need to use a Bain-Marie. If you don’t have one made-for-purpose, you can place a metal or heatproof glass bowl in a saucepan, with something to stop it from touching the floor of the pan. Then boil water in the pan (without letting the water get into the bowl), and melt the chocolate in the bowl—this will allow you to melt it evenly without burning the chocolate.
You will now have melted dark chocolate. It has its own set of polyphenols, and is great for everything from the brain to the gut microbiome.
3) Cut the dates lengthways on one side and remove the stone. Stuff them carefully with the coffee-flavored mascarpone (you can use a teaspoon, or use a piping kit if you have one). Add a couple of almonds to each one. Place them all on a big plate, and drizzle the melted chocolate over them. Add the petals if you have them.
The dates and almonds deliver extra vitamins and minerals in abundance (not to mention, lots of fiber), and also are an amazing combination even just by themselves. With the mascarpone and chocolate added, this winning on new levels. We’re not done yet, though…
4) Chill them in the fridge for about 30 minutes.
Serve!
Learn more
For those interested in some of the science of what we have going on today:
- Make The Heart-Healthiest Coffee ← this is about cafestol content and why instant is heart-healthiest (alas)
- The Bitter Truth About Coffee (Or Is It) ← this is about the health benefits (and some risks, but mostly benefits) of coffee
- Why You Should Diversify Your Nuts ← almonds are a top-tier choice, but other nuts are good too! This recipe could work well with hazelnuts, for example (we wouldn’t call it “tiramisu crunch bites” in that case, though, since the flavor profile would change)
- Which Sugars Are Healthier, And Which Are Just The Same? ← for any worrying “aren’t dates sugary, though?”
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Matcha is having a moment. What are the health benefits of this green tea drink?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Matcha has experienced a surge in popularity in recent months, leading to reports of global shortages and price increases.
If you haven’t been caught up in the craze, matcha is a powdered version of green tea. On a cafe menu you might see a hot or iced matcha latte, or even a matcha-flavoured cake or pastry. A quick google brings up countless recipes incorporating matcha, both sweet and savoury.
Retailers and cafe owners have suggested the main reasons for matcha’s popularity include its “instagrammable” looks and its purported health benefits.
But what are the health benefits of matcha? Here’s what the evidence says.
Rawpixel.com/Shutterstock First, what is matcha?
Matcha is a finely ground powder of green tea leaves, which come from the plant Camellia sinensis. This is the same plant used to make green and black tea. However, the production process differentiates matcha from green and black tea.
For matcha, the tea plant is grown in shade. Once the leaves are harvested, they’re steamed and dried and the stems are removed. Then the leaves are carefully ground at controlled temperatures to form the powder.
The production process for green tea is simpler. The leaves are picked from the unshaded plants, heated and then dried. We then steep the dried leaves in hot water to get tea (whereas with matcha the whole leaf is consumed).
With black tea, after the leaves are picked they’re exposed to air, which leads to oxidation. This makes the leaves black and gives the tea a different flavour.
In countries such as Japan, matcha is traditionally whisked with water and served in a stone bowl. Charlotte May/Pexels A source of phytonutrients
Phytonutrients are chemical compounds found in plants which have a range of benefits for human health. Matcha contains several.
Chlorophyll gives plants such as Camellia sinensis their green colour. There’s some evidence chlorophyll may have health benefits – including anti-inflammatory, anti-cancer and anti-obesity effects – due to its antioxidant properties. Antioxidants neutralise free radicals, which are unstable molecules that harm our cells.
Theanine has been shown to improve sleep and reduce stress and anxiety. The only other known dietary source of theanine is mushrooms.
Caffeine is a phytonutrient we know well. Aside from increasing alertness, caffeine has also demonstrated antioxidant effects and some protection against a range of chronic and neurodegenerative diseases. However, too much caffeine can have negative side effects.
Interestingly, shading the plants while growing appears to change the nutritional composition of the leaf and may lead to higher levels of these phytonutrients in matcha compared to green tea.
Another compound worth mentioning is called catechins, of which there are several different types. Matcha powder similarly has more catechins than green tea. They are strong antioxidants, which have been shown to have protective effects against bacteria, viruses, allergies, inflammation and cancer. Catechins are also found in apples, blueberries and strawberries.
What are the actual health benefits?
So we know matcha contains a variety of phytonutrients, but does this translate to noticeable health benefits?
A review published in 2023 identified only five experimental studies that have given matcha to people. These studies gave participants about 2–4g of matcha per day (equivalent to 1–2 teaspoons of matcha powder), compared to a placebo, as either a capsule, in tea or in foods. Matcha decreased stress and anxiety, and improved memory and cognitive function. There was no effect on mood.
A more recent study showed 2g of matcha in older people aged 60 to 85 improved sleep quality. However, in younger people aged 27 to 64 in another study, matcha had little effect on sleep.
A study in people with obesity found no difference in the weight loss observed between the matcha group and the control group. This study did not randomise participants, and people knew which group they had been placed in.
It could be hypothesised that given you consume all of the leaf, and given levels of some phytonutrients may be higher due to the growing conditions, matcha may have more nutritional benefits than green tea. But to my knowledge there has been no direct comparison of health outcomes from green tea compared to matcha.
Matcha has grown in popularity – but evidence for its health benefits is still limited. Usanee/Shutterstock There’s lots of evidence for green tea
While to date a limited number of studies have looked at matcha, and none compared matcha and green tea, there’s quite a bit of research on the health benefits of drinking green tea.
A systematic review of 21 studies on green tea has shown similar benefits to matcha for improvements in memory, plus evidence for mood improvement.
There’s also evidence green tea provides other health benefits. Systematic reviews have shown green tea leads to weight loss in people with obesity, lower levels of certain types of cholesterol, and reduced blood pressure. Green tea may also lower the risk of certain types of cancer.
So, if you can’t get your hands on matcha at the moment, drinking green tea may be a good way to get your caffeine hit.
Although the evidence on green tea provides us with some hints about the health benefits of matcha, we can’t be certain they would be the same. Nonetheless, if your local coffee shop has a good supply of matcha, there’s nothing to suggest you shouldn’t keep enjoying matcha drinks.
However, it may be best to leave the matcha croissant or cronut for special occasions. When matcha is added to foods with high levels of added sugar, salt and saturated fat, any health benefits that could be attributed to the matcha may be negated.
Evangeline Mantzioris, Program Director of Nutrition and Food Sciences, Accredited Practising Dietitian, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Elderly loss of energy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Please please give some information on elderly loss of energy and how it can be corrected. Please!❞
A lot of that is the metabolic slump described above! While we certainly wouldn’t describe 60 as elderly, and the health impacts from those changes at 45–55 get a gentler curve from 60 onwards… that curve is only going in one direction if we don’t take exceptionally good care of ourselves.
And of course, there’s also a degree of genetic lottery, and external factors we can’t entirely control (e.g. injuries etc).
One factor that gets overlooked a lot, though, is really easy to fix: B-vitamins.
In particular, vitamins B1, B5, B6, and B12. Of those, especially vitamins B1 and B12.
(Vitamins B5 and B6 are critical to health too, but relatively few people are deficient in those, while many are deficient in B1 and/or B12, especially as we get older)
Without going so detailed as to make this a main feature: these vitamins are essential for energy conversion from food, and they will make a big big difference.
You might especially want to consider taking sulbutiamine, which is a synthetic version of thiamin (vitamin B1), and instead of being water-soluble, it’s fat-soluble, and it easily crosses the blood-brain barrier, which is a big deal.
As ever, always check with your doctor because your needs/risks may be different. Also, there can be a lot of reasons for fatigue and you wouldn’t want to overlook something important.
You might also want to check out yesterday’s sponsor, as they offer personalized at-home health testing to check exactly this sort of thing.
❝What are natural ways to lose weight after 60? Taking into account bad knees or ankles, walking may be out as an exercise, running certainly is.❞
Losing weight is generally something that comes more from the kitchen than the gym, as most forms of exercise (except HIIT; see below) cause the metabolism to slow afterwards to compensate.
However, exercise is still very important, and swimming is a fine option if that’s available to you.
A word to the wise: people will often say “gentle activities, like tai chi or yoga”, and… These things are not the same.
Tai chi and yoga both focus on stability and suppleness, which are great, but:
- Yoga is based around mostly static self-support, often on the floor
- Tai chi will have you very often putting most of your weight on one slowly-increasingly bent knee at a time, and if you have bad knees, we’ll bet you winced while reading that.
So, maybe skip tai chi, or at least keep it to standing meditations and the like, not dynamic routines. Qigong, the same breathing exercises used in tai chi, is also an excellent way to improve your metabolism, by the way.
Ok, back onto HIIT:
You might like our previous article: How To Do HIIT* (Without Wrecking Your Body)
*High-Intensity Interval Training (the article also explains what this is and why you want to do it)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: