Overdosing on Chemo: A Common Gene Test Could Save Hundreds of Lives Each Year
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One January morning in 2021, Carol Rosen took a standard treatment for metastatic breast cancer. Three gruesome weeks later, she died in excruciating pain from the very drug meant to prolong her life.
Rosen, a 70-year-old retired schoolteacher, passed her final days in anguish, enduring severe diarrhea and nausea and terrible sores in her mouth that kept her from eating, drinking, and, eventually, speaking. Skin peeled off her body. Her kidneys and liver failed. “Your body burns from the inside out,” said Rosen’s daughter, Lindsay Murray, of Andover, Massachusetts.
Rosen was one of more than 275,000 cancer patients in the United States who are infused each year with fluorouracil, known as 5-FU, or, as in Rosen’s case, take a nearly identical drug in pill form called capecitabine. These common types of chemotherapy are no picnic for anyone, but for patients who are deficient in an enzyme that metabolizes the drugs, they can be torturous or deadly.
Those patients essentially overdose because the drugs stay in the body for hours rather than being quickly metabolized and excreted. The drugs kill an estimated 1 in 1,000 patients who take them — hundreds each year — and severely sicken or hospitalize 1 in 50. Doctors can test for the deficiency and get results within a week — and then either switch drugs or lower the dosage if patients have a genetic variant that carries risk.
Yet a recent survey found that only 3% of U.S. oncologists routinely order the tests before dosing patients with 5-FU or capecitabine. That’s because the most widely followed U.S. cancer treatment guidelines — issued by the National Comprehensive Cancer Network — don’t recommend preemptive testing.
The FDA added new warnings about the lethal risks of 5-FU to the drug’s label on March 21 following queries from KFF Health News about its policy. However, it did not require doctors to administer the test before prescribing the chemotherapy.
The agency, whose plan to expand its oversight of laboratory testing was the subject of a House hearing, also March 21, has said it could not endorse the 5-FU toxicity tests because it’s never reviewed them.
But the FDA at present does not review most diagnostic tests, said Daniel Hertz, an associate professor at the University of Michigan College of Pharmacy. For years, with other doctors and pharmacists, he has petitioned the FDA to put a black box warning on the drug’s label urging prescribers to test for the deficiency.
“FDA has responsibility to assure that drugs are used safely and effectively,” he said. The failure to warn, he said, “is an abdication of their responsibility.”
The update is “a small step in the right direction, but not the sea change we need,” he said.
Europe Ahead on Safety
British and European Union drug authorities have recommended the testing since 2020. A small but growing number of U.S. hospital systems, professional groups, and health advocates, including the American Cancer Society, also endorse routine testing. Most U.S. insurers, private and public, will cover the tests, which Medicare reimburses for $175, although tests may cost more depending on how many variants they screen for.
In its latest guidelines on colon cancer, the Cancer Network panel noted that not everyone with a risky gene variant gets sick from the drug, and that lower dosing for patients carrying such a variant could rob them of a cure or remission. Many doctors on the panel, including the University of Colorado oncologist Wells Messersmith, have said they have never witnessed a 5-FU death.
In European hospitals, the practice is to start patients with a half- or quarter-dose of 5-FU if tests show a patient is a poor metabolizer, then raise the dose if the patient responds well to the drug. Advocates for the approach say American oncology leaders are dragging their feet unnecessarily, and harming people in the process.
“I think it’s the intransigence of people sitting on these panels, the mindset of ‘We are oncologists, drugs are our tools, we don’t want to go looking for reasons not to use our tools,’” said Gabriel Brooks, an oncologist and researcher at the Dartmouth Cancer Center.
Oncologists are accustomed to chemotherapy’s toxicity and tend to have a “no pain, no gain” attitude, he said. 5-FU has been in use since the 1950s.
Yet “anybody who’s had a patient die like this will want to test everyone,” said Robert Diasio of the Mayo Clinic, who helped carry out major studies of the genetic deficiency in 1988.
Oncologists often deploy genetic tests to match tumors in cancer patients with the expensive drugs used to shrink them. But the same can’t always be said for gene tests aimed at improving safety, said Mark Fleury, policy director at the American Cancer Society’s Cancer Action Network.
When a test can show whether a new drug is appropriate, “there are a lot more forces aligned to ensure that testing is done,” he said. “The same stakeholders and forces are not involved” with a generic like 5-FU, first approved in 1962, and costing roughly $17 for a month’s treatment.
Oncology is not the only area in medicine in which scientific advances, many of them taxpayer-funded, lag in implementation. For instance, few cardiologists test patients before they go on Plavix, a brand name for the anti-blood-clotting agent clopidogrel, although it doesn’t prevent blood clots as it’s supposed to in a quarter of the 4 million Americans prescribed it each year. In 2021, the state of Hawaii won an $834 million judgment from drugmakers it accused of falsely advertising the drug as safe and effective for Native Hawaiians, more than half of whom lack the main enzyme to process clopidogrel.
The fluoropyrimidine enzyme deficiency numbers are smaller — and people with the deficiency aren’t at severe risk if they use topical cream forms of the drug for skin cancers. Yet even a single miserable, medically caused death was meaningful to the Dana-Farber Cancer Institute, where Carol Rosen was among more than 1,000 patients treated with fluoropyrimidine in 2021.
Her daughter was grief-stricken and furious after Rosen’s death. “I wanted to sue the hospital. I wanted to sue the oncologist,” Murray said. “But I realized that wasn’t what my mom would want.”
Instead, she wrote Dana-Farber’s chief quality officer, Joe Jacobson, urging routine testing. He responded the same day, and the hospital quickly adopted a testing system that now covers more than 90% of prospective fluoropyrimidine patients. About 50 patients with risky variants were detected in the first 10 months, Jacobson said.
Dana-Farber uses a Mayo Clinic test that searches for eight potentially dangerous variants of the relevant gene. Veterans Affairs hospitals use a 11-variant test, while most others check for only four variants.
Different Tests May Be Needed for Different Ancestries
The more variants a test screens for, the better the chance of finding rarer gene forms in ethnically diverse populations. For example, different variants are responsible for the worst deficiencies in people of African and European ancestry, respectively. There are tests that scan for hundreds of variants that might slow metabolism of the drug, but they take longer and cost more.
These are bitter facts for Scott Kapoor, a Toronto-area emergency room physician whose brother, Anil Kapoor, died in February 2023 of 5-FU poisoning.
Anil Kapoor was a well-known urologist and surgeon, an outgoing speaker, researcher, clinician, and irreverent friend whose funeral drew hundreds. His death at age 58, only weeks after he was diagnosed with stage 4 colon cancer, stunned and infuriated his family.
In Ontario, where Kapoor was treated, the health system had just begun testing for four gene variants discovered in studies of mostly European populations. Anil Kapoor and his siblings, the Canadian-born children of Indian immigrants, carry a gene form that’s apparently associated with South Asian ancestry.
Scott Kapoor supports broader testing for the defect — only about half of Toronto’s inhabitants are of European descent — and argues that an antidote to fluoropyrimidine poisoning, approved by the FDA in 2015, should be on hand. However, it works only for a few days after ingestion of the drug and definitive symptoms often take longer to emerge.
Most importantly, he said, patients must be aware of the risk. “You tell them, ‘I am going to give you a drug with a 1 in 1,000 chance of killing you. You can take this test. Most patients would be, ‘I want to get that test and I’ll pay for it,’ or they’d just say, ‘Cut the dose in half.’”
Alan Venook, the University of California-San Francisco oncologist who co-chairs the panel that sets guidelines for colorectal cancers at the National Comprehensive Cancer Network, has led resistance to mandatory testing because the answers provided by the test, in his view, are often murky and could lead to undertreatment.
“If one patient is not cured, then you giveth and you taketh away,” he said. “Maybe you took it away by not giving adequate treatment.”
Instead of testing and potentially cutting a first dose of curative therapy, “I err on the latter, acknowledging they will get sick,” he said. About 25 years ago, one of his patients died of 5-FU toxicity and “I regret that dearly,” he said. “But unhelpful information may lead us in the wrong direction.”
In September, seven months after his brother’s death, Kapoor was boarding a cruise ship on the Tyrrhenian Sea near Rome when he happened to meet a woman whose husband, Atlanta municipal judge Gary Markwell, had died the year before after taking a single 5-FU dose at age 77.
“I was like … that’s exactly what happened to my brother.”
Murray senses momentum toward mandatory testing. In 2022, the Oregon Health & Science University paid $1 million to settle a suit after an overdose death.
“What’s going to break that barrier is the lawsuits, and the big institutions like Dana-Farber who are implementing programs and seeing them succeed,” she said. “I think providers are going to feel kind of bullied into a corner. They’re going to continue to hear from families and they are going to have to do something about it.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Avoid Age-Related Macular Degeneration
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Avoiding Age-Related Macular Degeneration
Eye problems can strike at any age, but as we get older, it becomes a lot more likely. In particular, age-related macular degeneration is, as the name suggests, an age-bound disease.
Is there no escaping it, then?
The risk factors for age-related macular degeneration are as follows:
- Being over the age of 55 (can’t do much about this one)
- Being over the age of 65 (risk climbs sharply now)
- Having a genetic predisposition (can’t do much about this one)
- Having high cholesterol (this one we can tackle)
- Having cardiovascular disease (this one we can tackle)
- Smoking (so, just don’t)
Genes predispose; they don’t predetermine. Or to put it another way: genes load the gun, but lifestyle pulls the trigger.
Preventative interventions against age-related macular degeneration
Prevention is better than a cure in general, and this especially goes for things like age-related macular degeneration, because the most common form of it has no known cure.
So first, look after your heart (because your heart feeds your eyes).
See also: The Mediterranean Diet
Next, eat to feed your eyes specifically. There’s a lot of research to show that lutein helps avoid age-related diseases in the eyes and the rest of the brain, too:
See also: Brain Food? The Eyes Have It
Do supplements help?
They can! There was a multiple-part landmark study by the National Eye Institute, a formula was developed that reduced the 5-year risk of intermediate disease progressing to late disease by 25–30%. It also reduced the risk of vision loss by 19%.
You can read about both parts of the study here:
Age-Related Eye Disease Studies (AREDS/AREDS2): major findings
As you can see, an improvement was made between the initial study and the second one, by replacing beta-carotene with lutein and zeaxanthin.
The AREDS2 formula contains:
- 500 mg vitamin C
- 180 mg vitamin E
- 80 mg zinc
- 10 mg lutein
- 2 mg copper
You can learn more about these supplements, and where to get them, here on the NEI’s corner of the official NIH website:
AREDS 2 Supplements for Age-Related Macular Degeneration
Take care of yourself!
Share This Post
-
Are You Taking PIMs?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Getting Off The Overmedication Train
The older we get, the more likely we are to be on more medications. It’s easy to assume that this is because, much like the ailments they treat, we accumulate them over time. And superficially at least, that’s what happens.
And yet, almost half of people over 65 in Canada are taking “potentially inappropriate medications”, or PIMs—in other words, medications that are not needed and perhaps harmful. This categorization includes medications where the iatrogenic harms (side effects, risks) outweigh the benefits, and/or there’s a safer more effective medication available to do the job.
You may be wondering: what does this mean for the US?
Well, we don’t have the figures for the US because we’re working from Canadian research today, but given the differences between the two country’s healthcare systems (mostly socialized in Canada and mostly private in the US), it seems a fair hypothesis that if it’s almost half in Canada, it’s probably more than half in the US. Socialized healthcare systems are generally quite thrifty and seek to spend less on healthcare, while private healthcare systems are generally keen to upsell to new products/services.
The three top categories of PIMs according to the above study:
- Gabapentinoids (anticonvulsants also used to treat neuropathic pain)
- Proton pump inhibitors (PPIs)
- Antipsychotics (especially, to people without psychosis)
…but those are just the top of the list; there are many many more.
The list continues: opioids, anticholinergics, sulfonlyurea, NSAIDs, benzodiazepines and related rugs, and cholinesterase inhibitors. That’s where the Canadian study cuts off (although it also includes “others” just before NSAIDs), but still, you guessed it, there are more (we’re willing to bet statins weigh heavily in the “others” section, for a start).
There are two likely main causes of overmedication:
The side effect train
This is where a patient has a condition and is prescribed drug A, which has some undesired side effects, so the patient is prescribed drug B to treat those. However, that drug also has some unwanted side effects of its own, so the patient is prescribed drug C to treat those. And so on.
For a real-life rundown of how this can play out, check out the case study in:
The Hidden Complexities of Statins and Cardiovascular Disease (CVD)
The convenience factor
No, not convenient for you. Convenient for others. Convenient for the doctor if it gets you out of their office (socialized healthcare) or because it was easy to sell (private healthcare). Convenient for the staff in a hospital or other care facility.
This latter is what happens when, for example, a patient is being too much trouble, so the staff give them promazine “to help them settle down”, notwithstanding that promazine is, besides being a sedative, also an antipsychotic whose common side effects include amenorrhea, arrhythmias, constipation, drowsiness and dizziness, dry mouth, impotence, tiredness, galactorrhoea, gynecomastia, hyperglycemia, insomnia, hypotension, seizures, tremor, vomiting and weight gain.
This kind of thing (and worse) happens more often towards the end of a patient’s life; indeed, sometimes precipitating that end, whether you want it or not:
Mortality, Palliative Care, & Euthanasia
How to avoid it
Good practice is to be “open-mindedly skeptical” about any medication. By this we mean, don’t reject it out of hand, but do ask questions about it.
Ask your prescriber not only what it’s for and what it’ll do, but also what the side effects and risks are, and an important question that many people don’t think to ask, and for which doctors thus don’t often have a well-prepared smooth-selling reply, “what will happen if I don’t take this?”
And look up unbiased neutral information about it, from reliable sources (Drugs.com and The BNF are good reference guides for this—and if it’s important to you, check both, in case of any disagreement, as they function under completely different regulatory bodies, the former being American and the latter being British. So if they both agree, it’s surely accurate, according to best current science).
Also: when you are on a medication, keep a journal of your symptoms, as well as a log of your vitals (heart rate, blood pressure, weight, sleep etc) so you know what the medication seems to be helping or harming, and be sure to have a regular meds review with your doctor to check everything’s still right for you. And don’t be afraid to seek a second opinion if you still have doubts.
Want to know more?
For a more in-depth exploration than we have room for here, check out this book that we reviewed not long back:
To Medicate or Not? That is the Question! – by Dr. Asha Bohannon
Take care!
Share This Post
-
HBD: The Human Being Diet – by Petronella Ravenshear
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We don’t often review diet books, so why did this one catch our attention? The answer lies in its comprehensive nature without being excessively long and complex.
Ravenshear (a nutritionist) brings a focus on metabolic balance, and what will and won’t work for keeping it healthy.
The first part of the book is mostly informational; covering such things as blood sugar balance, gut health, hormones, and circadian rhythm considerations, amongst others.
The second, larger part of the book is mostly instructional; do this and that, don’t do the other, guidelines on quantities and timings, and what things may be different for some people, and what to do about those.
The style is conversational and light, but well-grounded in good science.
Bottom line: if you’d like a “one-stop shop” for giving your diet an overhaul, this book is a fine choice.
Click here to check out the Human Being Diet, and enjoy the best of health!
Share This Post
Related Posts
-
100,000 People, 30 Years, One Clear Winner vs Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Generally speaking, the scientific community most highly lauds the Mediterranean diet as being best for general health:
The Mediterranean Diet: What Is It Good For? ← what isn’t it good for?!
However, even this can be tweaked with specific health considerations in mind, for example:
Four Ways To Upgrade The Mediterranean Diet ← these tweaks offer adjusted versions of the Mediterranean diet, optimized for anti-inflammation, gut health, heart health, or brain health
And today we present to you some very good research into…
The best diet for aging well
Let’s be clear on terms first: by “aging well”, this means reaching age 70 without chronic diseases and maintaining good cognitive, physical, and mental health.
105,015 participants (of whom, 66% women, average age 53 at the start of the study) were followed for up to 30 years. Not in the stalkery way, but in the longitudinal study way. We say “up to”, because as with any sizeable longitudinal study, some died before the end of the study.
9,771 of them were deemed, at the end of the study, to have achieved “healthy aging”.
So, how did those participants achieve that, in terms of diet?
The dietary patterns that had the strongest positive impact were:
- AHEI (Alternative Healthy Eating Index): best for mental and physical function, overall healthy aging.
- PHDI (Planetary Health Diet Index): best for cognitive health and survival to age 70.
- DASH (Dietary Approaches to Stop Hypertension): strongest general impact.
- MIND (Mediterranean-DASH Intervention for Neurodegenerative Delay): best for brain health.
- rEDIH (Reversed Empirical Dietary Index for Hyperinsulinemia): most effective for chronic disease prevention.
In contrast:
- EIDP (Empirically Inflammatory Dietary Pattern): shocking nobody, performed least well in all areas
You are probably wondering what those dietary patterns actually consist of, so click here to see a chart of what’s included or excluded in each dietary pattern.
As you can see, the AHEI diet that was “best for mental and physical function, overall healthy aging” is essentially the Mediterranean diet with three small tweaks:
- no seafood, but long-chain omega-3 fatty acids include to compensate
- no sugar-sweetened beverages or fruit juices
- “no” sodium (in other words, minimal sodium, since almost everything contains trace amounts)
The PHDI diet, which was “best for cognitive health and survival to age 70” is essentially a whole-foods plant-based diet. Which in turn is very consistent with the Mediterranean, except that it excludes animal products, of which the Mediterranean diet uses small amounts.
You can read the paper in its entirety here:
Optimal dietary patterns for healthy aging
Want to know more?
A panel of 69 doctors and nutritionists examined the evidence for 38 diets (including Mediterranean, MIND, DASH, Vegan, Keto, Slimfast, WeightWatchers, Nutrisystem, and more) and scored them in 21 categories (e.g. best for general health, best for weight loss, best for heart, best against diabetes, etc):
Which Diet? Top Diets Ranked By Experts
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What are ‘collarium’ sunbeds? Here’s why you should stay away
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Reports have recently emerged that solariums, or sunbeds – largely banned in Australia because they increase the risk of skin cancer – are being rebranded as “collarium” sunbeds (“coll” being short for collagen).
Commercial tanning and beauty salons in Queensland, New South Wales and Victoria are marketing collariums, with manufacturers and operators claiming they provide a longer lasting tan and stimulate collagen production, among other purported benefits.
A collarium sunbed emits both UV radiation and a mix of visible wavelength colours to produce a pink or red light. Like an old-school sunbed, the user lies in it for ten to 20 minute sessions to quickly develop a tan.
But as several experts have argued, the providers’ claims about safety and effectiveness don’t stack up.
Why were sunbeds banned?
Commercial sunbeds have been illegal across Australia since 2016 (except for in the Northern Territory) under state-based radiation safety laws. It’s still legal to sell and own a sunbed for private use.
Their dangers were highlighted by young Australians including Clare Oliver who developed melanoma after using sunbeds. Oliver featured in the No Tan Is Worth Dying For campaign and died from her melanoma at age 26 in 2007.
Sunbeds lead to tanning by emitting UV radiation – as much as six times the amount of UV we’re exposed to from the summer sun. When the skin detects enough DNA damage, it boosts the production of melanin, the brown pigment that gives you the tanned look, to try to filter some UV out before it hits the DNA. This is only partially successful, providing the equivalent of two to four SPF.
Essentially, if your body is producing a tan, it has detected a significant amount of DNA damage in your skin.
Research shows people who have used sunbeds at least once have a 41% increased risk of developing melanoma, while ten or more sunbed sessions led to a 100% increased risk.
In 2008, Australian researchers estimated that each year, sunbeds caused 281 cases of melanoma, 2,572 cases of squamous cell carcinoma (another common type of skin cancer), and $3 million in heath-care costs, mostly to Medicare.
How are collarium sunbeds supposed to be different?
Australian sellers of collarium sunbeds imply they are safe, but their machine descriptions note the use of UV radiation, particularly UVA.
UVA is one part of the spectrum of UV radiation. It penetrates deeper into the skin than UVB. While UVB promotes cancer-causing mutations by discharging energy straight into the DNA strand, UVA sets off damage by creating reactive oxygen species, which are unstable compounds that react easily with many types of cell structures and molecules. These damage cell membranes, protein structures and DNA.
Evidence shows all types of sunbeds increase the risk of melanoma, including those that use only UVA.
Some manufacturers and clinics suggest the machine’s light spectrum increases UV compatibility, but it’s not clear what this means. Adding red or pink light to the mix won’t negate the harm from the UV. If you’re getting a tan, you have a significant amount of DNA damage.
Collagen claims
One particularly odd claim about collarium sunbeds is that they stimulate collagen.
Collagen is the main supportive tissue in our skin. It provides elasticity and strength, and a youthful appearance. Collagen is constantly synthesised and broken down, and when the balance between production and recycling is lost, the skin loses strength and develops wrinkles. The collagen bundles become thin and fragmented. This is a natural part of ageing, but is accelerated by UV exposure.
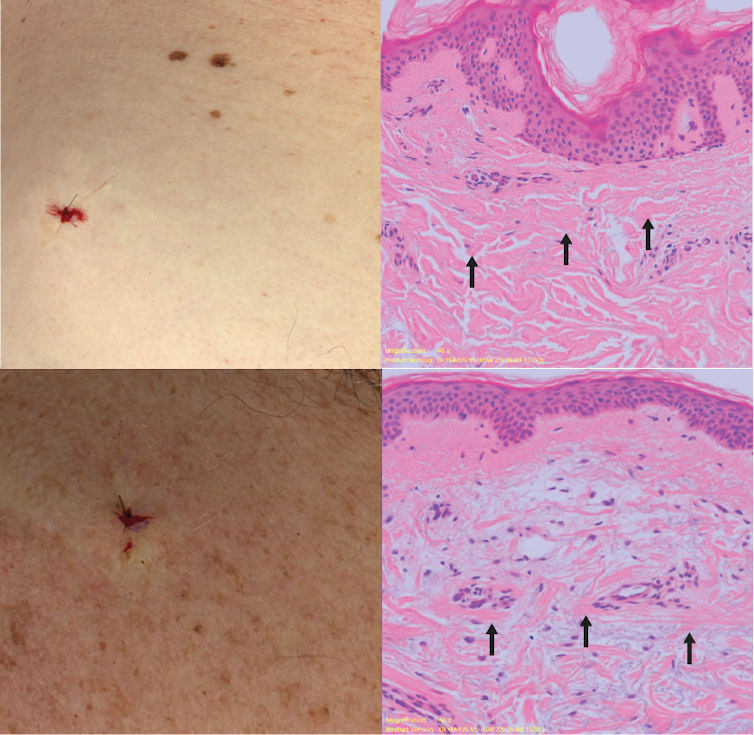
Sun-protected skin (top) has thick bands of pink collagen (arrows) in the dermis, as seen on microscopic examination. Chronically sun-damaged skin (bottom) has much thinner collagen bands.
Katie Lee/UQThe reactive oxygen species generated by UVA light damage existing collagen structures and kick off a molecular chain of events that downgrades collagen-producing enzymes and increases collagen-destroying enzymes. Over time, a build-up of degraded collagen fragments in the skin promotes even more destruction.
While there is growing evidence red light therapy alone could be useful in wound healing and skin rejuvenation, the UV radiation in collarium sunbeds is likely to undo any benefit from the red light.
What about phototherapy?
There are medical treatments that use controlled UV radiation doses to treat chronic inflammatory skin diseases like psoriasis.
The anti-collagen effects of UVA can also be used to treat thickened scars and keloids. Side-effects of UV phototherapy include tanning, itchiness, dryness, cold sore virus reactivation and, notably, premature skin ageing.
These treatments use the minimum exposure necessary to treat the condition, and are usually restricted to the affected body part to minimise risks of future cancer. They are administered under medical supervision and are not recommended for people already at high risk of skin cancer, such as people with atypical moles.
So what happens now?
It looks like many collariums are just sunbeds rebranded with red light. Queensland Health is currently investigating whether these salons are breaching the state’s Radiation Safety Act, and operators could face large fines.
As the 2024 Australians of the Year – melanoma treatment pioneers Georgina Long and Richard Scolyer – highlighted in their acceptance speech, “there is nothing healthy about a tan”, and we need to stop glamorising tanning.
However, if you’re desperate for the tanned look, there is a safer and easy way to get one – out of a bottle or by visiting a salon for a spray tan.
Katie Lee, PhD Candidate, Dermatology Research Centre, The University of Queensland and Anne Cust, Professor of Cancer Epidemiology, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cordyceps: Friend Or Foe?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cordyceps: friend or foe?
Cordyceps is a famously frightening fungus. It’s the one responsible for “zombie ants” and other zombie creatures, and it’s the basis for the existential threat to humanity in the TV show The Last of Us.
It’s a parasitic fungus that controls the central and peripheral nervous systems of its host, slowly replacing the host’s body, as well as growing distinctive spines that erupt out of the host’s body. Taking over motor functions, it compels the host to do two main things, which are to eat more food, and climb to a position that will be good to release spores from.
Fortunately, none of that matters to humans. Cordyceps does not (unlike in the TV show) affect humans that way.
What does Cordyceps do in humans?
Cordyceps (in various strains) is enjoyed as a health supplement, based on a long history of use in Traditional Chinese Medicine, and nowadays it’s coming under a scientific spotlight too.
The main health claims for it are:
- Against inflammation
- Against aging
- Against cancer
- For blood sugar management
- For heart health
- For exercise performance
Sounds great! What does the science say?
There’s a lot more science for the first three (which are all closely related to each other, and often overlapping in mechanism and effect).
So let’s take a look:
Against inflammation
The science looks promising for this, but studies so far have either been in vitro (cell cultures in petri dishes), or else murine in vivo (mouse studies), for example:
- Anti-inflammatory effects of Cordyceps mycelium in murine macrophages
- Cordyceps sinensis as an immunomodulatory agent
- Immunomodulatory functions of extracts from Cordyceps cicadae
- Cordyceps pruinosa inhibits in vitro and in vivo inflammatory mediators
In summary: we can see that it has anti-inflammatory properties for mice and in the lab; we’d love to see the results of studies done on humans, though. Also, while it has anti-inflammatory properties, it performed less well than commonly-prescribed anti-inflammatory drugs, for example:
❝C. militaris can modulate airway inflammation in asthma, but it is less effective than prednisolone or montelukast.❞
Against aging
Because examining the anti-aging effects of a substance requires measuring lifespans and repeating the experiment, anti-aging studies do not tend to be done on humans, because they would take lifetimes to perform. To this end, it’s inconvenient, but not a criticism of Cordyceps, that studies have been either mouse studies (short lifespan, mammals like us) or fruit fly studies (very short lifespan, genetically surprisingly similar to us).
The studies have had positive results, with typical lifespan extensions of 15–20%:
- The lifespan-extending effect of Cordyceps sinensis in normal mice
- Cordyceps sinensis oral liquid prolongs the lifespan of the fruit fly, Drosophila melanogaster
- Anti-aging activity of polysaccharides from Cordyceps militaris
- Anti-aging effect of Cordyceps sinensis extract
Against cancer
Once again, the studies here have been in vitro, or murine in vivo. They do look good though:
In vitro (human cell cultures in a lab):
In vivo (mouse studies):
Summary of these is: Cordyceps quite reliably inhibits tumor growth in vitro (human cell cultures) and in vivo (mouse studies). However, trials in human cancer patients are so far conspicuous by their absence.
For blood sugar management
Cordyceps appears to mimic the action of insulin, without triggering insulin sensitivity. For example:
The anti-hyperglycemic activity of the fruiting body of Cordyceps in diabetic rats
There were some other rat/mouse studies with similar results. No studies in humans yet.
For heart health
Cordyceps contains adenosine. You may remember that caffeine owes part of its stimulant effect to blocking adenosine, the hormone that makes us feel sleepy. So in this way, Cordyceps partially does the opposite of what caffeine does, and may be useful against arrhythmia:
Cardiovascular protection of Cordyceps sinensis act partially via adenosine receptors
For exercise performance
A small (30 elderly participants) study found that Cordyceps supplementation improved VO2 max by 7% over the course of six weeks:
However, another small study (22 young athletes) failed to reproduce those results:
Cordyceps Sinensis supplementation does not improve endurance exercise performance
In summary…
Cordyceps almost certainly has anti-inflammation, anti-aging, and anti-cancer benefits.
Cordyceps may have other benefits too, but the evidence is thinner on the ground for those, so far.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: