How gender-affirming care improves trans mental health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In recent years, a growing number of states have passed laws restricting or banning gender-affirming care for transgender people, particularly minors. As conversations about gender-affirming care increase, so do false narratives about it, with some opponents falsely suggesting that it’s harmful to mental health.
Despite widespread attacks against gender-affirming care, research clearly shows that it improves mental health outcomes for transgender people.
Read on to learn more about what gender-affirming care is, how it benefits mental well-being, and how you can access it.
What is gender-affirming care?
Gender-affirming care describes a range of medical interventions that help align people’s bodies with their gender identities. While anyone can seek gender-affirming care in the form of laser hair removal, breast augmentation, erectile dysfunction medication, or hormone therapy, among other treatments, most conversations about gender-affirming care center around transgender people, whose gender identity or gender expression does not conform to their sex assigned at birth.
Gender-affirming care for trans people varies based on age. For example, some trans adults seek hormone replacement therapy (HRT) or gender-affirming surgeries that help their bodies match their internal sense of gender.
Trans kids entering adolescence might be prescribed puberty blockers, which temporarily delay the production of hormones that initiate puberty, to give them more time to figure out their gender identities before deciding on next steps. This is the same medication given to cisgender kids—whose gender identities match the sex they were assigned at birth—experiencing early puberty.
What is gender dysphoria?
Gender dysphoria describes a feeling of unease that some trans people experience when their perceived gender doesn’t match their gender identity. This can lead to a range of mental health conditions that affect their quality of life
Some trans people may manage gender dysphoria by wearing gender-affirming clothing, opting for a gender-affirming hairstyle, or asking others to refer to them by a name and pronouns that authentically represent them. Others may need gender-affirming care to feel at home in their bodies.
Trans people who desire gender-affirming care and have not been able to access it experience psychological distress, including depression, anxiety, self-harm, and suicidal ideation. The Trevor Project’s 2023 U.S. National Survey on the Mental Health of LGBTQ Young People found that roughly half of trans youth “seriously considered attempting suicide in the past year.”

How does gender-affirming care improve mental health?
For trans adults, gender-affirming care can alleviate gender dysphoria, which has been shown to improve both short-term and long-term mental health. A 2018 study found that trans adults who do not undergo HRT are four times more likely to experience depression than those who do, although not all trans people desire HRT.
Extensive research has shown that gender-affirming care also alleviates gender dysphoria and improves mental health outcomes in trans kids, teens, and young adults. A 2022 study found that access to HRT and puberty blockers lowered the odds of depression in trans people between the ages of 13 and 20 by 60 percent and reduced the risk of self-harm and suicidal thoughts by 73 percent.
Both the Endocrine Society—which aims to advance hormone research—and the American Academy of Pediatrics recommend that trans kids and teens have access to developmentally appropriate gender-affirming care.
How can I access gender-affirming care?
If you’re a trans adult seeking gender-affirming care or a guardian of a trans kid or teen who’s seeking gender-affirming care, talk to your health care provider about your options. You can find a trans-affirming provider by searching the World Professional Association for Transgender Health directory or visiting your local LGBTQ+ health center or Planned Parenthood.
Some gender-affirming care may not be covered by insurance. Learn how to make the most of your coverage from the National Center for Transgender Equality. Find insurance plans available through the Marketplace that cover gender-affirming care in some states through Out2Enroll.
Some states restrict or ban gender-affirming care. Learn about the laws in your state by visiting the Trans Legislation Tracker.
Where can trans people and their families find mental health support?
In addition to working with a trans-affirming therapist, trans people and their families can find mental health support through these free services:
- PFLAG offers resources for families and friends of LGBTQ+ people. Find a PFLAG chapter near you.
- The Trevor Project’s hotline has trained counselors who help LGBTQ+ youth in crisis. Call the TrevorLifeline 1-866-488-7386 or text START to 678-678.
- The Trans Lifeline was created by and for the trans community to support trans people in crisis. You can reach the Trans Lifeline hotline at 1-877-565-8860.
For more information, talk to your health care provider.
If you or anyone you know is considering suicide or self-harm or is anxious, depressed, upset, or needs to talk, call the Suicide & Crisis Lifeline at 988 or text the Crisis Text Line at 741-741. For international resources, here is a good place to begin.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Strong Bones Forever − by Dr. Raymond Hinish
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This doctor of pharmacy would like for fewer people to take (or need to take) osteoporosis medications. Indeed, as the subtitle suggests, the focus here is on drug-free solutions.
And not just because “natural is better” as an argument without evidence, rather, he talks about the limitations and drawbacks of osteoporosis medications (which we wrote about previously, but he has more room to go into more detail), whereupon some osteoporosis meds may do more harm than good.
His method boasts improvements in bone density by 11% or more in two years, and covers such topics as:
- which calcium (and why no, dairy is not what you want; it contains things that inhibit calcium absorption, so the calcium will be stuck in your arteries instead of your bones)
- which minerals are more important than calcium, and why
- common mistakes that many people make that sabotage their bone density
It’s about more than just diet though; he does also talk about hormones, and not just other lifestyle factors, but also many “industry secrets” that aren’t really secrets per se, it’s just, people outside of the industry don’t usually know them—pertaining to things like how to get the most out of bone density tests (i.e. how to get better accuracy), how to meaningfully assess fracture risk, and, if choosing to take osteoporosis meds, how to minimize the risks and maximize the benefits.
The style is very direct and informational, very easy to read, remarkably jargon-free, and our only criticism is that there is no bibliography.
Bottom line: if you’d like to improve your bone density, this book can certainly help with that.
Click here to check out Strong Bones Forever, and have strong bones forever!
Share This Post
-
An RSV vaccine has been approved for people over 60. But what about young children?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Therapeutic Goods Administration (TGA) has approved a vaccine against respiratory syncytial virus (RSV) in Australia for the first time. The shot, called Arexvy and manufactured by GSK, will be available by prescription to adults over 60.
RSV is a contagious respiratory virus which causes an illness similar to influenza, most notably in babies and older adults.
So while it will be good to have an RSV vaccine available for older people, where is protection up to for the youngest children?
A bit about RSV
RSV was discovered in chimpanzees with respiratory illness in 1956, and was soon found to be a common cause of illness in humans.
There are two key groups of people we would like to protect from RSV: babies (up to about one year old) and people older than 60.
Babies tend to fill up hospitals during the RSV season in late spring and winter in large numbers, but severe infection requiring admission to intensive care is less common.
In babies and younger children, RSV generally causes a wheezing asthma-like illness (bronchiolitis), but can also cause pneumonia and croup.
Although there are far fewer hospital admissions among older people, they can develop severe disease and die from an infection.
Babies account for the majority of hospitalisations with RSV.
Prostock-studio/ShutterstockRSV vaccines for older people
For older adults, there are actually several RSV vaccines in the pipeline. The recent Australian TGA approval of Arexvy is likely to be the first of several, with other vaccines from Pfizer and Moderna currently in development.
The GSK and Pfizer RSV vaccines are similar. They both contain a small component of the virus, called the pre-fusion protein, that the immune system can recognise.
Both vaccines have been shown to reduce illness from RSV by more than 80% in the first season after vaccination.
In older adults, side effects following Arexvy appear to be similar to other vaccines, with a sore arm and generalised aches and fatigue frequently reported.
Unlike influenza vaccines which are given each year, it is anticipated the RSV vaccine would be a one-off dose, at least at this stage.
Protecting young children from RSV
Younger babies don’t tend to respond well to some vaccines due to their immature immune system. To prevent other diseases, this can be overcome by giving multiple vaccine doses over time. But the highest risk group for RSV are those in the first few months of life.
To protect this youngest age group from the virus, there are two potential strategies available instead of vaccinating the child directly.
The first is to give a vaccine to the mother and rely on the protective antibodies passing to the infant through the placenta. This is similar to how we protect babies by vaccinating pregnant women against influenza and pertussis (whooping cough).
The second is to give antibodies directly to the baby as an injection. With both these strategies, the protection provided is only temporary as antibodies wane over time, but this is sufficient to protect infants through their highest risk period.
Women could be vaccinated during pregnancy to protect their baby in its first months of life.
Image Point Fr/ShutterstockAbrysvo, the Pfizer RSV vaccine, has been trialled in pregnant women. In clinical trials, this vaccine has been shown to reduce illness in infants for up to six months. It has been approved in pregnant women in the United States, but is not yet approved in Australia.
An antibody product called palivizumab has been available for many years, but is only partially effective and extremely expensive, so has only been given to a small number of children at very high risk.
A newer antibody product, nirsevimab, has been shown to be effective in reducing infections and hospitalisations in infants. It was approved by the TGA in November, but it isn’t yet clear how this would be accessed in Australia.
What now?
RSV, like influenza, is a major cause of respiratory illness, and the development of effective vaccines represents a major advance.
While the approval of the first vaccine for older people is an important step, many details are yet to be made available, including the cost and the timing of availability. GSK has indicated its vaccine should be available soon. While the vaccine will initially only be available on private prescription (with the costs paid by the consumer), GSK has applied for it to be made free under the National Immunisation Program.
In the near future, we expect to hear further news about the other vaccines and antibodies to protect those at higher risk from RSV disease, including young children.
Allen Cheng, Professor of Infectious Diseases, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
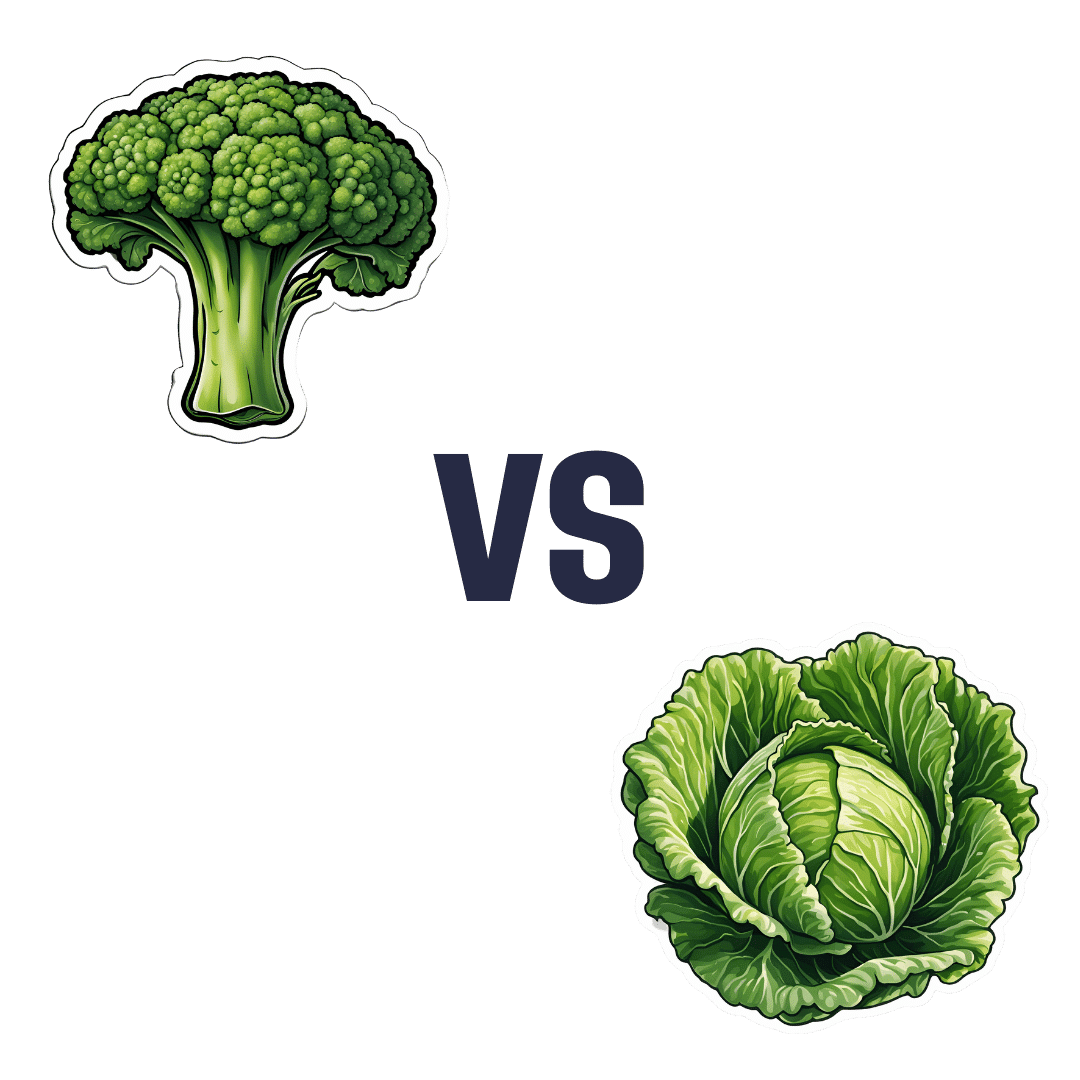
Broccoli vs Cabbage – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing broccoli to cabbage, we picked the broccoli.
Why?
Here we go once again pitting two different cultivars of the same species (Brassica oleracea) against each other, and/but once again, there is one that comes out as nutritionally best.
In terms of macros, broccoli has more protein, carbs, and fiber, while they are both low glycemic index foods. The differences are small though, so it’s fairest to call this category a tie.
When it comes to vitamins, broccoli has more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, E, K, and choline, while cabbage is not higher in any vitamins. It should be noted that cabbage is still good for these, especially vitamins C and K, but broccoli is simply better.
In the category of minerals, broccoli has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while cabbage is not higher in any minerals. Again though, cabbage is still good, especially in calcium, iron, and manganese, but again, broccoli is simply better.
Of course, enjoy either or both! But if you want the nutritionally densest option, it’s broccoli.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Share This Post
Related Posts
-
Peach vs Papaya – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing peach to papaya, we picked the peach.
Why?
It was close!
In terms of macros, there’s not much between them; they are close to identical on protein, carbs, and fiber. Technically peach has slightly more protein (+0.4g/100g) and papaya has slightly more carbs and fiber (+1.28g/100g carbs, +0.2g/100g fiber), but since the differences are so tiny, we’re calling this section a tie—bearing in mind, these numbers are based on averages, which means that when they’re very close, they’re meaningless—one could easily, for example, pick up a peach that has more fiber than a papaya, because that 0.2g/100g is well within the margin of variation. So, as we say: a tie.
When it comes to vitamins, things are also close; peaches have more of vitamins B1, B2, B3, and E, while papaya has more of vitamins A, B6, B9, and C. This is a 4:4 tie, but since the most notable margin of difference is vitamin C (of which papayas have 9x more) while the others are much closer, we’ll call this a tie-breaker win for papaya.
The category of minerals sets things apart more: peaches have more copper, iron, manganese, phosphorus, potassium, and zinc, while papaya has more calcium, magnesium, and selenium. That’s already a 6:3 win for peaches, before we take into account that the numbers for papaya’s calcium and selenium are tiny, so adding this to the already 6:3 win for peaches makes for a clear and easy win for peaches in this category.
Adding up the sections is 1W/1D/1L for both fruits, but looking at the win/loss for each, it’s clear which won/lost on a tiebreaker, and which won/lost by a large margin, so peaches get the victory here.
Of course, enjoy either or both, though! And see below for a bonus feature of peaches:
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer ← peaches are high on this list! They kill cancer cells while sparing healthy ones 🙂
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Functional Exercise For Seniors – by James Atkinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of exercises books are tailored to 20-year-old athletes training for their first Tough Mudder. Others, that the only thing standing between us and a perfect Retroflex Countersupine Divine Pretzel position is a professionally-lit Instagrammable photo.
This one’s not like that.
But! Nor does it think being over a certain age is a reason to not have genuinely robust health, of the kind that may make some younger people envious. So, it lays out, in progressive format, guidelines for exercises targeted at everything we need to build and maintain as we get older.
The writing style is clear, and the illustrations too (the cover art is the same style as the illustrations inside).
Bottom line: if you’re looking for a workout guide that understands you are nearer 80 than 18, and/but also doesn’t assume your age limits your exercise potential to “wrist exercises in chair”, then this book is a fine pick.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Your Simplest Life – by Lisa Turner
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We probably know how to declutter, and perhaps even do a “unnecessary financial expenditures” audit. So, what does this offer beyond that?
A large portion of this book focuses on keeping our general life in a state of “flow”, and strategies include:
- How to make sure you’re doing the right part of the 80:20 split on a daily basis
- Knowing when to switch tasks, and when not to
- Knowing how to plan time for tasks
- No more reckless optimism, but also without falling foul of Parkinson’s Law (i.e. work expands to fill the time allotted to it)
- Decluttering your head, too!
When it comes to managing life responsibilities in general, Turner is very attuned to generational differences… Including the different challenges faced by each generation, what’s more often expected of us, what we’re used to, and how we probably initially learned to do it (or not).
To this end, a lot of strategies are tailored with variations for each age group. Not often does an author take the time to address each part of their readership like that, and it’s really helpful that she does!
All in all, a great book for simplifying your daily life.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: