Breathe; Don’t Vent (At Least In The Moment)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Zen And The Art Of Breaking Things
We’ve talked before about identifying emotions and the importance of being able to express them:
Answering The Most Difficult Question: How Are You?
However, there can be a difference between “expressing how we feel” and “being possessed by how we feel and bulldozing everything in our path”
…which is, of course, primarily a problem in the case of anger—and by extension, emotions that are often contemporaneous with anger, such as jealousy, shame, fear, etc.
How much feeling is too much?
While this is in large part a subjective matter, clinically speaking the key question is generally: is it adversely affecting daily life to the point of being a problem?
For example, if you have to spend half an hour every day actively managing a certain emotion, that’s probably indicative of something unusual, but “unusual” is not inherently bad. If you’re managing it safely and in a way that doesn’t negatively affect the rest of your life, then that is generally considered fine, unless you feel otherwise about it.
A good example of this is complicated grief and/or prolonged grief.
But what about when it comes to anger? How much is ok?
When it comes to those around you, any amount of anger can seem like too much. Anger often makes us short-tempered even with people who are not the object of our anger, and it rarely brings out the best in us.
We can express our feelings in non-aggressive ways, for example:
and
Seriously Useful Communication Skills!
Sometimes, there’s another way though…
Breathe; don’t vent
That’s a great headline, but we can’t take the credit for it, because it came from:
Breathe, don’t vent: turning down the heat is key to managing anger
…in which it was found that, by all available metrics, the popular wisdom of “getting it off your chest” doesn’t necessarily stand up to scrutiny, at least in the short term:
❝The work was inspired in part by the rising popularity of rage rooms that promote smashing things (such as glass, plates and electronics) to work through angry feelings.
I wanted to debunk the whole theory of expressing anger as a way of coping with it,” she said. “We wanted to show that reducing arousal, and actually the physiological aspect of it, is really important.❞
And indeed, he and his team did find that various arousal-increasing activities (such as hitting a punchbag, breaking things, doing vigorous exercise) did not help as much as arousal-decreasing activities, such as mindfulness-based relaxation techniques.
If you’d like to read the full paper, then so would we, but we couldn’t get full access to this one yet. However, the abstract includes representative statistics, so that’s worth a once-over:
Caveat!
Did you notice the small gap between their results and their conclusion?
In a lab or similar short-term observational setting, their recommendation is clearly correct.
However, if the source of your anger is something chronic and persistent, it could well be that calming down without addressing the actual cause is just “kicking the can down the road”, and will still have to actually be dealt with eventually.
So, while “here be science”, it’s not a mandate for necessarily suffering in silence. It’s more about being mindful about how we go about tackling our anger.
As for a primer on mindfulness, feel free to check out:
No-Frills, Evidence-Based Mindfulness
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Case of the Armadillo: Is It Spreading Leprosy in Florida?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
GAINESVILLE, Fla. — In an open-air barn at the edge of the University of Florida, veterinarian Juan Campos Krauer examines a dead armadillo’s footpads and ears for signs of infection.
Its claws are curled tight and covered in blood. Campos Krauer thinks it was struck in the head while crossing a nearby road.
He then runs a scalpel down its underside. He removes all the important organs: heart, liver, kidneys. Once the specimens are bottled up, they’re destined for an ultra-cold freezer in his lab at the college.
Campos Krauer plans to test the armadillo for leprosy, an ancient illness also known as Hansen’s disease that can lead to nerve damage and disfigurement in humans. He and other scientists are trying to solve a medical mystery: why Central Florida has become a hot spot for the age-old bacteria that cause it.
Leprosy remains rare in the United States. But Florida, which often reports the most cases of any state, has seen an uptick in patients. The epicenter is east of Orlando. Brevard County reported a staggering 13% of the nation’s 159 leprosy cases in 2020, according to a Tampa Bay Times analysis of state and federal data.
Many questions about the phenomenon remain unanswered. But leprosy experts believe armadillos play a role in spreading the illness to people. To better understand who’s at risk and to prevent infections, about 10 scientists teamed up last year to investigate. The group includes researchers from the University of Florida, Colorado State University, and Emory University in Atlanta.
“How this transmission is happening, we really don’t know,” said Ramanuj Lahiri, chief of the laboratory research branch for the National Hansen’s Disease Program, which studies the bacteria involved and cares for leprosy patients across the country.
‘Nothing Was Adding Up’
Leprosy is believed to be the oldest human infection in history. It probably has been sickening people for at least 100,000 years. The disease is highly stigmatized — in the Bible, it was described as a punishment for sin. In more modern times, patients were isolated in “colonies” around the world, including in Hawaii and Louisiana.
In mild cases, the slow-growing bacteria cause a few lesions. If left untreated, they can paralyze the hands and feet.
But it’s actually difficult to fall ill with leprosy, as the infection isn’t very contagious. Antibiotics can cure the ailment in a year or two. They’re available for free through the federal government and the World Health Organization, which launched a campaign in the 1990s to eliminate leprosy as a public health problem.
In 2000, reported U.S. cases dropped to their lowest point in decades with 77 infections. But they later increased, averaging about 180 per year from 2011 to 2020, according to data from the National Hansen’s Disease Program.
During that time, a curious trend emerged in Florida.
In the first decade of the 21st century, the state logged 67 cases. Miami-Dade County noted 20 infections — the most of any Florida county. The vast majority of its cases were acquired outside the U.S., according to a Times analysis of Florida Department of Health data.
But over the next 10 years, recorded cases in the state more than doubled to 176 as Brevard County took center stage.
The county, whose population is about a fifth the size of Miami-Dade’s, logged 85 infections during that time — by far the most of any county in the state and nearly half of all Florida cases. In the previous decade, Brevard noted just five cases.
Remarkably, at least a quarter of Brevard’s infections were acquired within the state, not while the individuals were abroad. India, Brazil, and Indonesia diagnose more leprosy cases than anywhere, reporting over 135,000 infections combined in 2022 alone. People were getting sick even though they hadn’t traveled to such areas or been in close contact with existing leprosy patients, said Barry Inman, a former epidemiologist at the Brevard health department who investigated the cases and retired in 2021.
“Nothing was adding up,” Inman said.
A few patients recalled touching armadillos, which are known to carry the bacteria. But most didn’t, he said. Many spent a lot of time outdoors, including lawn workers and avid gardeners. The cases were usually mild.
It was difficult to nail down where people got the illness, he added. Because the bacteria grow so slowly, it can take anywhere from nine months to 20 years for symptoms to begin.
Amoeba or Insect Culprits?
Heightened awareness of leprosy could play a role in Brevard’s groundswell of cases.
Doctors must report leprosy to the health department. Yet Inman said many in the county didn’t know that, so he tried to educate them after noticing cases in the late 2000s.
But that’s not the sole factor at play, Inman said.
“I don’t think there’s any doubt in my mind that something new is going on,” he said.
Other parts of Central Florida have also recorded more infections. From 2011 to 2020, Polk County logged 12 cases, tripling its numbers compared with the previous 10 years. Volusia County noted 10 cases. It reported none the prior decade.
Scientists are honing in on armadillos. They suspect the burrowing critters may indirectly cause infections through soil contamination.
Armadillos, which are protected by hard shells, serve as good hosts for the bacteria, which don’t like heat and can thrive in the animals whose body temperatures range from a cool 86-95 degrees.
Colonists probably brought the disease to the New World hundreds of years ago, and somehow armadillos became infected, said Lahiri, the National Hansen’s Disease Program scientist. The nocturnal mammals can develop lesions from the illness just as humans can. More than 1 million armadillos occupy Florida, estimated Campos Krauer, an assistant professor in the University of Florida’s Department of Large Animal Clinical Sciences.
How many carry leprosy is unclear. A study published in 2015 of more than 600 armadillos in Alabama, Florida, Georgia, and Mississippi found that about 16% showed evidence of infection. Public health experts believe leprosy was previously confined to armadillos west of the Mississippi River, then spread east.
Handling the critters is a known hazard. Lab research shows that single-cell amoebas, which live in soil, can also carry the bacteria.
Armadillos love to dig up and eat earthworms, frustrating homeowners whose yards they damage. The animals may shed the bacteria while hunting for food, passing it to amoebas, which could later infect people.
Leprosy experts also wonder if insects help spread the disease. Blood-sucking ticks might be a culprit, lab research shows.
“Some people who are infected have little to no exposure to the armadillo,” said Norman Beatty, an assistant professor of medicine at the University of Florida. “There is likely another source of transmission in the environment.”
Campos Krauer, who’s been searching Gainesville streets for armadillo roadkill, wants to gather infected animals and let them decompose in a fenced-off area, allowing the remains to soak into a tray of soil while flies lay eggs. He hopes to test the dirt and larvae to see if they pick up the bacteria.
Adding to the intrigue is a leprosy strain found only in Florida, according to scientists.
In the 2015 study, researchers discovered that seven armadillos from the Merritt Island National Wildlife Refuge, which is mostly in Brevard but crosses into Volusia, carried a previously unseen version of the pathogen.
Ten patients in the region were stricken with it, too. At the genetic level, the strain is similar to another type found in U.S. armadillos, said Charlotte Avanzi, a Colorado State University researcher who specializes in leprosy.
It’s unknown if the strain causes more severe disease, Lahiri said.
Reducing Risk
The public should not panic about leprosy, nor should people race to euthanize armadillos, researchers warn.
Scientists estimate that over 95% of the global human population has a natural ability to ward off the disease. They believe months of exposure to respiratory droplets is needed for person-to-person transmission to occur.
But when infections do happen, they can be devastating.
“If we better understand it,” Campos Krauer said, “the better we can learn to live with it and reduce the risk.”
The new research may also provide insight for other Southern states. Armadillos, which don’t hibernate, have been moving north, Campos Krauer said, reaching areas like Indiana and Virginia. They could go farther due to climate change.
People concerned about leprosy can take simple precautions, medical experts say. Those working in dirt should wear gloves and wash their hands afterward. Raising garden beds or surrounding them with a fence may limit the chances of soil contamination. If digging up an armadillo burrow, consider wearing a face mask, Campos Krauer said.
Don’t play with or eat the animals, added John Spencer, a scientist at Colorado State University who studies leprosy transmission in Brazil. They’re legal to hunt year-round in Florida without a license.
Campos Krauer’s team has so far examined 16 dead armadillos found on Gainesville area roads, more than 100 miles from the state’s leprosy epicenter, trying to get a preliminary idea of how many carry the bacteria.
None has tested positive yet.
This article was produced through a partnership between KFF Health News and the Tampa Bay Times.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Taurine’s Benefits For Heart Health And More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Taurine: Research Review
First, what is taurine, beyond being an ingredient in many energy drinks?
It’s an amino acid that many animals, including humans, can synthesize in our bodies. Some other animals—including obligate carnivores such as cats (but not dogs, who are omnivorous by nature) cannot synthesize taurine and must get it from food.
So, as humans are very versatile omnivorous frugivores by nature, we have choices:
- Synthesize it—no need for any conscious action; it’ll just happen
- Eat it—by eating meat, which contains taurine
- Supplement it—by taking supplements, including energy drinks, which generally (but not always) use a bioidentical lab-made taurine. Basically, lab-made taurine is chemically identical to the kind found in meat, it’s just cheaper and doesn’t involve animals as a middleman.
What does it do?
Taurine does a bunch of essential things, including:
- Maintaining hydration/electrolyte balance in cells
- Regulating calcium/magnesium balance in cells
- Forming bile salts, which are needed for digestion
- Supporting the integrity of the central nervous system
- Regulating the immune system and antioxidative processes
Thus, a shortage of taurine can lead to such issues as kidney problems, eye tissue damage (since the eyes are a particularly delicate part of the CNS), and cardiomyopathy.
If you want to read more, here’s an academic literature review:
Taurine: A “very essential” amino acid
On the topic of eye health, a 2014 study found that taurine is the most plentiful amino acid in the eye, and helps protect against retinal degeneration, in which they say:
❝We here review the evidence for a role of taurine in retinal ganglion cell survival and studies suggesting that this compound may be involved in the pathophysiology of glaucoma or diabetic retinopathy. Along with other antioxidant molecules, taurine should therefore be seriously reconsidered as a potential treatment for such retinal diseases❞
Read more: Taurine: the comeback of a neutraceutical in the prevention of retinal degenerations
Taurine for muscles… In more than sports!
We’d be remiss not to mention that taurine is enjoyed by athletes to enhance athletic performance; indeed, it’s one of its main selling-points:
See: Taurine in sports and exercise
But! It’s also useful for simply maintaining skeleto-muscular health in general, and especially in the context of age-related decline and chronic disease:
Taurine: the appeal of a safe amino acid for skeletal muscle disorders
On the topic of safety… How safe is it?
There’s an interesting answer to that question. Within safe dose ranges (we’ll get to that), taurine is not only relatively safe, but also, studies that looked to explore its risks found new benefits in the process. Specifically of interest to us were that it appears to promote better long-term memory, especially as we get older (as taurine levels in the brain decline with age):
Taurine, Caffeine, and Energy Drinks: Reviewing the Risks to the Adolescent Brain
^Notwithstanding the title, we assure you, the research got there; they said:
❝Interestingly, the levels of taurine in the brain decreased significantly with age, which led to numerous studies investigating the potential neuroprotective effects of supplemental taurine in several different experimental models❞
What experimental models were those? These ones:
- Taurine protects cerebellar neurons of the external granular layer
- Effects of taurine on alterations of neurobehavior and neurodevelopment key proteins expression
- Neuroprotective role of taurine in developing offspring affected by maternal alcohol consumption
…which were all animal studies, however.
The same systematic review also noted that not only was more research needed on humans, but also, existing studies have had a strong bias to male physiology (in both human and assorted other animal studies), so more diverse study is needed too.
What are the safe dose ranges?
Before we get to toxicity, let’s look at some therapeutic doses. In particular, some studies that found that 500mg 3x daily, i.e. 1.5g total daily, had benefits for heart health:
- Taurine and atherosclerosis
- The Anti-Inflammatory Effect of Taurine on Cardiovascular Disease
- Taurine supplementation has anti-atherogenic and anti-inflammatory effects before and after incremental exercise in heart failure
- Taurine Supplementation Lowers Blood Pressure and Improves Vascular Function in Prehypertension
- Taurine improves the vascular tone through the inhibition of TRPC3 function in the vasculature
Bottom line on safety: 3g/day has been found to be safe:
Share This Post
-
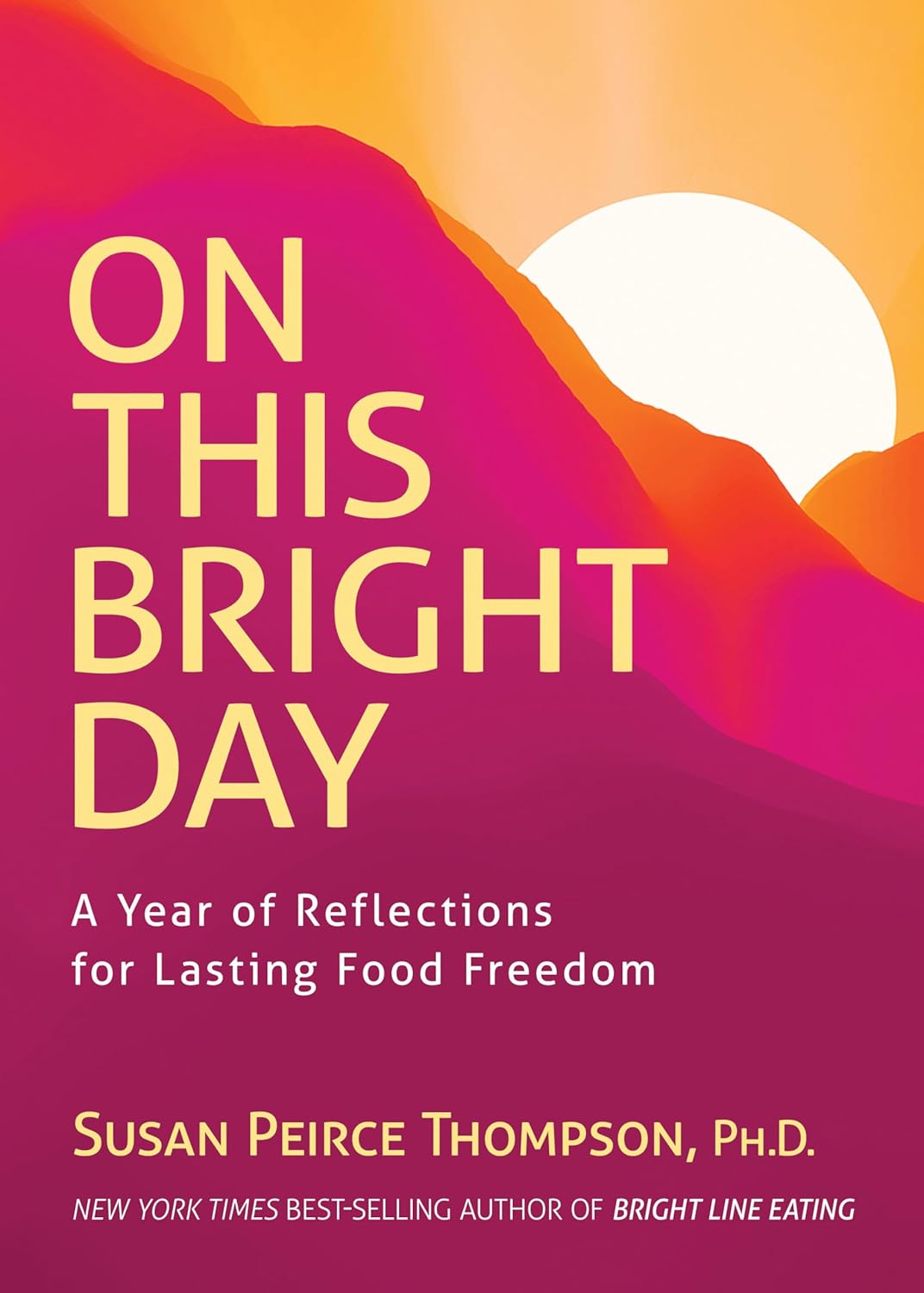
On This Bright Day – by Dr. Susan Thompson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is principally aimed at those who have struggled with emotional/comfort eating, over-eating, and/or compulsive eating of some kind.
However, its advices go for the “little compulsions” too, the many small unhealthy choices that add up. Thus, this book has value for most if not all of us.
The format is: each day has a little quotation, followed by a short discussion of that, which is then underlined by an affirmation for the day.
The main thrust of the book is to promote mindful eating, and it does this well with daily reminders that are helpful without being preachy.
Bottom line: if you enjoy “daily reader” type books and would like a daily reminder to practice mindful eating, then this book is for you!
Click here to check out On This Bright Day, and enjoy your food mindfully, every day!
Share This Post
Related Posts
-
Relationships: When To Stick It Out & When To Call It Quits
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Like A Ship Loves An Anchor?
Today’s article may seem a little bit of a downer to start with, but don’t worry, it picks up again too. Simply put, we’ve written before about many of the good parts of relationships, e.g:
Only One Kind Of Relationship Promotes Longevity This Much!
…but what if that’s not what we have?
Note: if you have a very happy, secure, fulfilling, joyous relationship, then, great! Or if you’re single and happy, then, also great! Hopefully you will still find today’s feature of use if you find yourself advising a friend or family member one day. So without further ado, let’s get to it…
You may be familiar with the “sunk cost fallacy”; if not: it’s what happens when a person or group has already invested into a given thing, such that even though the thing is not going at all the way they hoped, they now want to continue trying to make that thing work, lest their previous investment be lost. But the truth is: if it’s not going to work, then the initial investment is already lost, and pouring out extra won’t help—it’ll just lose more.
That “investment” in a given thing could be money, time, energy, or (often the case) a combination of the above.
In the field of romance, the “sunk cost fallacy” keeps a lot of bad relationships going for longer than perhaps they should, and looking back (perhaps after a short adjustment period), the newly-single person says “why did I let that go on?” and vows to not make the same mistake again.
But that prompts the question: how can we know when it’s right to “keep working on it, because relationships do involve work”, as perfectly reasonable relationship advice often goes, and when it’s right to call it quits?
Should I stay or should I go?
Some questions for you (or perhaps a friend you might find yourself advising) to consider:
- What qualities do you consider the most important for a partner to have—and does your partner have them?
- If you described the worst of your relationship to a close friend, would that friend feel bad for you?
- Do you miss your partner when they’re away, or are you glad of the break? When they return, are they still glad to see you?
- If you weren’t already in this relationship, would you seek to enter it now? (This takes away sunk cost and allows a more neutral assessment)
- Do you feel completely safe with your partner (emotionally as well as physically), or must you tread carefully to avoid conflict?
- If your partner decided tomorrow that they didn’t want to be with you anymore and left, would that be just a heartbreak, or an exciting beginning of a new chapter in your life?
- What things would you generally consider dealbreakers in a relationship—and has your partner done any of them?
The last one can be surprising, by the way. We often see or hear of other people’s adverse relationship situations and think “I would never allow…” yet when we are in a relationship and in love, there’s a good chance that we might indeed allow—or rather, excuse, overlook, and forgive.
And, patience and forgiveness certainly aren’t inherently bad traits to have—it’s just good to deploy them consciously, and not merely be a doormat.
Either way, reflect (or advise your friend/family member to reflect, as applicable) on the “score” from the above questions.
- If the score is good, then maybe it really is just a rough patch, and the tools we link at the top and bottom of this article might help.
- If the score is bad, the relationship is bad, and no amount of historic love or miles clocked up together will change that. Sometimes it’s not even anyone’s fault; sometimes a relationship just ran its course, and now it’s time to accept that and turn to a new chapter.
“At my age…”
As we get older, it’s easy for that sunk cost fallacy to loom large. Inertia is heavy, the mutual entanglement of lives is far-reaching, and we might not feel we have the same energy for dating that we did when we were younger.
And there may sometimes be a statistical argument for “sticking it out” at least for a while, depending on where we are in the relationship, per this study (with 165,039 participants aged 20–76), which found:
❝Results on mean levels indicated that relationship satisfaction decreased from age 20 to 40, reached a low point at age 40, then increased until age 65, and plateaued in late adulthood.
As regards the metric of relationship duration, relationship satisfaction decreased during the first 10 years of the relationship, reached a low point at 10 years, increased until 20 years, and then decreased again.❞
Source: Development of Relationship Satisfaction Across the Life Span: A Systematic Review and Meta-Analysis
And yet, when it comes to prospects for a new relationship…
- If our remaining life is growing shorter, then it’s definitely too short to spend in an unhappy relationship
- Maybe we really won’t find romance again… And maybe that’s ok, if w’re comfortable making our peace with that and finding joy in the rest of life (this widowed writer (hi, it’s me) plans to remain single now by preference, and her life is very full of purpose and beauty and joy and yes, even love—for family, friends, etc, plus the memory of my wonderful late beloved)
- Nevertheless, the simple fact is: many people do find what they go on to describe as their best relationship yet, late in life ← this study is with a small sample size, but in this case, even anecdotal evidence seems sufficient to make the claim reasonable; probably you personally know someone who has done so. If they can, so can you, if you so wish.
- Adding on to that last point… Later life relationships can also offer numerous significant advantages unique to such (albeit some different challenges too—but with the right person, those challenges are just a fun thing to tackle together). See for example:
An exploratory investigation into dating among later‐life women
And about those later-life relationships that do work? They look like this:
this one looks like the title says it all, but it really doesn’t, and it’s very much worth at least reading the abstract, if not the entire paper—because it talks a lot about the characteristics that make for happy or unhappy relationships, and the effect that those things have on people. It really is very good, and quite an easy read.
See again: Healthy Relationship, Healthy Life
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Snooze-Button Controversy
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
To Snooze Or Not To Snooze? (Science Has Answers)
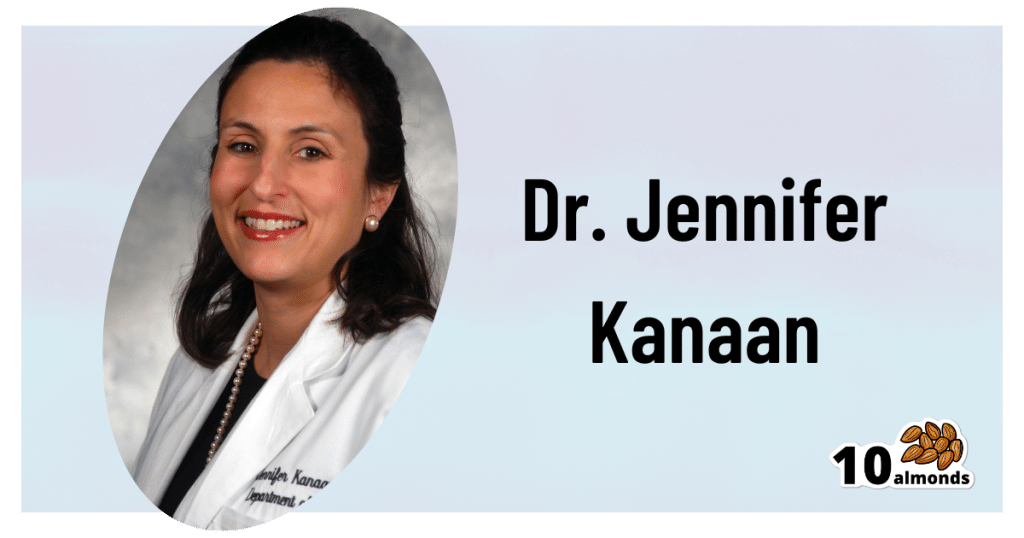
This is Dr. Jennifer Kanaan. She’s a medical doctor with a focus on pulmonary critical care, sleep disorders, and sleep medicine.
What does she want to tell us?
She wants us to be wary of the many news articles that have jumped on a certain recent sleep study, such as:
- Is hitting the snooze button really a bad idea? Study sheds light on the impact of morning alarms on sleep and cognition
- Hitting Snooze May Help You Feel Less Sleepy and More Alert, Research Says
- Is it okay to press the snooze button?
- Hitting Snooze May Help You Feel Less Sleepy and More Alert, Research Says
- Hitting the snooze button on your alarm doesn’t make you more tired
For the curious, here is the paper itself, by Dr. Tina Sundelin et al. It’s actually two studies, by the way, but one paper:
The authors of this study concluded:
❝There were no clear effects of snoozing on the cortisol awakening response, morning sleepiness, mood, or overnight sleep architecture.
A brief snooze period may thus help alleviate sleep inertia, without substantially disturbing sleep, for late chronotypes and those with morning drowsiness.❞
Notably, people tend to snooze because an alarm clock will, if not “smart” about it, wake us up mid sleep-cycle more often than not, and that will produce a short “sleep hangover”. By snoozing, we are basically re-rolling the dice on being woken up between sleep cycles, and thus feeling more refreshed.
What’s Dr. Kanaan’s counterpoint?
Dr. Kanaan says:
❝If you’re coming in and out of sleep for 30 minutes, after the alarm goes off the first time, you’re costing yourself 30 minutes of uninterrupted, quality, restorative sleep. This study doesn’t change that fact.❞
She advises that rather than snoozing, we should prioritize getting good sleep in the first place, and once we do wake up, mid sleep-cycle or not, get sunlight. That way, our brain will start promptly scrubbing melatonin and producing the appropriate wakefulness hormones instead. That means serotonin, and also a spike of cortisol.
Remember: cortisol is only bad when it’s chronically elevated. It’s fine, and even beneficial, to have a short spike of cortisol. We make it for a reason!
If you’d like to hear more from Dr. Kanaan, you might like this interview with her at the University of Connecticut:
Want the best of both worlds?
A great option to avoid getting woken in the middle of a sleep cycle, and also not needing to hit snooze, is a sunrise alarm clock. Specifics of these devices vary, but for example, the kind this writer has starts gently glowing an hour before the set alarm time,and gradually gets brighter and lighter over the course of the hour.
We don’t sell them, but here’s an example sunrise alarm clock on Amazon, for your convenience
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Best Salt for Neti Pots?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
❓ Q&A With 10almonds Subscribers!
Q: What kind of salt is best for neti pots?
A: Non-iodised salt is usually recommended, but really, any human-safe salt is fine. By this we mean for example:
- Sodium chloride (like most kitchen salts),
- Potassium chloride (as found in “reduced sodium” kitchen salts), or
- Magnesium sulfate (also known as epsom salts).
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: