Wholewheat Bread vs Seeded White – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing wholewheat bread to seeded bread, we picked the wholewheat.
Why?
First, we will acknowledge that this is a false dichotomy; it is possible to have seeded wholewheat bread. However, it is very common to have wholewheat bread that isn’t seeded, and white bread that is seeded. So, it’s important to be able to decide which is the healthier option, since very often, this false dichotomy is what’s on offer.
We will also advise checking labels (or the baker, if getting from a bakery) to ensure that visibly brown bread is actually wholewheat, and not just dyed brown with caramel coloring or such (yes, that is a thing that some companies do).
Now, as for why we chose the wholewheat over the seeded white…
In terms of macronutrients, wholewheat bread has (on average; individual breads may vary of course) has 2x the protein and a lot more fiber.
Those seeds in seeded bread? They just aren’t enough to make a big impact on the overall nutritional value of the bread in those regards. Per slice, you are getting, what, 10 seeds maybe? This is not a meaningful dietary source of much.
Seeded bread does have proportionally more healthy fats, but the doses are still so low as to make it not worth the while; it just looks like a lot of expressed as a percentage of comparison, because of the wholewheat bread has trace amounts, and the seeded bread has several times those trace amounts, it’s still a tiny amount. So, we’d recommend looking to other sources for those healthy fats.
Maybe dip your bread, of whatever kind, into extra virgin olive oil, for example.
Wholewheat bread of course also has a lower glycemic index. Those seeds in seeded white bread don’t really slow it down at all, because they’re not digested until later.
Want to learn more?
You might like to read:
- Carb-Strong or Carb-Wrong?
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Gluten: What’s The Truth?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
WHO Overturns Dogma on Airborne Disease Spread. The CDC Might Not Act on It.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The World Health Organization has issued a report that transforms how the world understands respiratory infections like covid-19, influenza, and measles.
Motivated by grave missteps in the pandemic, the WHO convened about 50 experts in virology, epidemiology, aerosol science, and bioengineering, among other specialties, who spent two years poring through the evidence on how airborne viruses and bacteria spread.
However, the WHO report stops short of prescribing actions that governments, hospitals, and the public should take in response. It remains to be seen how the Centers for Disease Control and Prevention will act on this information in its own guidance for infection control in health care settings.
The WHO concluded that airborne transmission occurs as sick people exhale pathogens that remain suspended in the air, contained in tiny particles of saliva and mucus that are inhaled by others.
While it may seem obvious, and some researchers have pushed for this acknowledgment for more than a decade, an alternative dogma persisted — which kept health authorities from saying that covid was airborne for many months into the pandemic.
Specifically, they relied on a traditional notion that respiratory viruses spread mainly through droplets spewed out of an infected person’s nose or mouth. These droplets infect others by landing directly in their mouth, nose, or eyes — or they get carried into these orifices on droplet-contaminated fingers. Although these routes of transmission still happen, particularly among young children, experts have concluded that many respiratory infections spread as people simply breathe in virus-laden air.
“This is a complete U-turn,” said Julian Tang, a clinical virologist at the University of Leicester in the United Kingdom, who advised the WHO on the report. He also helped the agency create an online tool to assess the risk of airborne transmission indoors.
Peg Seminario, an occupational health and safety specialist in Bethesda, Maryland, welcomed the shift after years of resistance from health authorities. “The dogma that droplets are a major mode of transmission is the ‘flat Earth’ position now,” she said. “Hurray! We are finally recognizing that the world is round.”
The change puts fresh emphasis on the need to improve ventilation indoors and stockpile quality face masks before the next airborne disease explodes. Far from a remote possibility, measles is on the rise this year and the H5N1 bird flu is spreading among cattle in several states. Scientists worry that as the H5N1 virus spends more time in mammals, it could evolve to more easily infect people and spread among them through the air.
Traditional beliefs on droplet transmission help explain why the WHO and the CDC focused so acutely on hand-washing and surface-cleaning at the beginning of the pandemic. Such advice overwhelmed recommendations for N95 masks that filter out most virus-laden particles suspended in the air. Employers denied many health care workers access to N95s, insisting that only those routinely working within feet of covid patients needed them. More than 3,600 health care workers died in the first year of the pandemic, many due to a lack of protection.
However, a committee advising the CDC appears poised to brush aside the updated science when it comes to its pending guidance on health care facilities.
Lisa Brosseau, an aerosol expert and a consultant at the Center for Infectious Disease Research and Policy in Minnesota, warns of a repeat of 2020 if that happens.
“The rubber hits the road when you make decisions on how to protect people,” Brosseau said. “Aerosol scientists may see this report as a big win because they think everything will now follow from the science. But that’s not how this works and there are still major barriers.”
Money is one. If a respiratory disease spreads through inhalation, it means that people can lower their risk of infection indoors through sometimes costly methods to clean the air, such as mechanical ventilation and using air purifiers, and wearing an N95 mask. The CDC has so far been reluctant to press for such measures, as it updates foundational guidelines on curbing airborne infections in hospitals, nursing homes, prisons, and other facilities that provide health care. This year, a committee advising the CDC released a draft guidance that differs significantly from the WHO report.
Whereas the WHO report doesn’t characterize airborne viruses and bacteria as traveling short distances or long, the CDC draft maintains those traditional categories. It prescribes looser-fitting surgical masks rather than N95s for pathogens that “spread predominantly over short distances.” Surgical masks block far fewer airborne virus particles than N95s, which cost roughly 10 times as much.
Researchers and health care workers have been outraged about the committee’s draft, filing letters and petitions to the CDC. They say it gets the science wrong and endangers health. “A separation between short- and long-range distance is totally artificial,” Tang said.
Airborne viruses travel much like cigarette smoke, he explained. The scent will be strongest beside a smoker, but those farther away will inhale more and more smoke if they remain in the room, especially when there’s no ventilation.
Likewise, people open windows when they burn toast so that smoke dissipates before filling the kitchen and setting off an alarm. “You think viruses stop after 3 feet and drop to the ground?” Tang said of the classical notion of distance. “That is absurd.”
The CDC’s advisory committee is comprised primarily of infection control researchers at large hospital systems, while the WHO consulted a diverse group of scientists looking at many different types of studies. For example, one analysis examined the puff clouds expelled by singers, and musicians playing clarinets, French horns, saxophones, and trumpets. Another reviewed 16 investigations into covid outbreaks at restaurants, a gym, a food processing factory, and other venues, finding that insufficient ventilation probably made them worse than they would otherwise be.
In response to the outcry, the CDC returned the draft to its committee for review, asking it to reconsider its advice. Meetings from an expanded working group have since been held privately. But the National Nurses United union obtained notes of the conversations through a public records request to the agency. The records suggest a push for more lax protection. “It may be difficult as far as compliance is concerned to not have surgical masks as an option,” said one unidentified member, according to notes from the committee’s March 14 discussion. Another warned that “supply and compliance would be difficult.”
The nurses’ union, far from echoing such concerns, wrote on its website, “The Work Group has prioritized employer costs and profits (often under the umbrella of ‘feasibility’ and ‘flexibility’) over robust protections.” Jane Thomason, the union’s lead industrial hygienist, said the meeting records suggest the CDC group is working backward, molding its definitions of airborne transmission to fit the outcome it prefers.
Tang expects resistance to the WHO report. “Infection control people who have built their careers on this will object,” he said. “It takes a long time to change people’s way of thinking.”
The CDC declined to comment on how the WHO’s shift might influence its final policies on infection control in health facilities, which might not be completed this year. Creating policies to protect people from inhaling airborne viruses is complicated by the number of factors that influence how they spread indoors, such as ventilation, temperature, and the size of the space.
Adding to the complexity, policymakers must weigh the toll of various ailments, ranging from covid to colds to tuberculosis, against the burden of protection. And tolls often depend on context, such as whether an outbreak happens in a school or a cancer ward.
“What is the level of mortality that people will accept without precautions?” Tang said. “That’s another question.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
What’s the difference between miscarriage and stillbirth?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
Former US First Lady Michelle Obama revealed in her memoir she had a miscarriage. UK singer-songwriter and actor Lily Allen has gone on the record about her stillbirth.
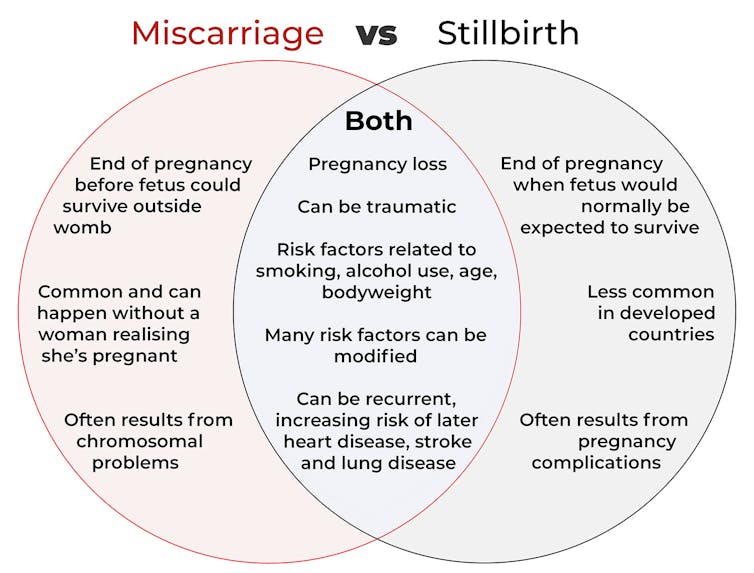
Both miscarriage and stillbirth are sadly familiar terms for pregnancy loss. They can be traumatic life events for the prospective parents and family, and their impacts can be long-lasting. But the terms can be confused.
Here are some similarities and differences between miscarriage and stillbirth, and why they matter.
christinarosepix/Shutterstock Let’s start with some definitions
In broad terms, a miscarriage is when a pregnancy ends while the fetus is not yet viable (before it could survive outside the womb).
This is the loss of an “intra-uterine” pregnancy, when an embryo is implanted in the womb to then develop into a fetus. The term miscarriage excludes ectopic pregnancies, where the embryo is implanted outside the womb.
However, stillbirth refers to the end of a pregnancy when the fetus is normally viable. There may have been sufficient time into the pregnancy. Alternatively, the fetus may have grown large enough to be normally expected to survive, but it dies in the womb or during delivery.
The Australian Institute of Health and Welfare defines stillbirth as a fetal death of at least 20 completed weeks of gestation or with a birthweight of at least 400 grams.
Internationally, definitions of stillbirth vary depending on the jurisdiction.
How common are they?
It is difficult to know how common miscarriages are as they can happen when a woman doesn’t know she is pregnant. There may be no obvious symptoms or something that looks like a heavier-than-normal period. So miscarriages are likely to be more common than reported.
Studies from Europe and North America suggest a miscarriage occurs in about one in seven pregnancies (15%). More than one in eight women (13%) will have a miscarriage at some time in her life.
Around 1–2% of women have recurrent miscarriages. In Australia this is when someone has three or more miscarriages with no pregnancy in between.
Australia has one of the lowest rates of stillbirth in the world. The rate has been relatively steady over the past 20 years at 0.7% or around seven per 1,000 pregnancies.
Who’s at risk?
Someone who has already had a miscarriage or stillbirth has an increased risk of that outcome again in a subsequent pregnancy.
Compared with women who have had a live birth, those who have had a stillbirth have double the risk of another. For those who have had recurrent miscarriages, the risk of another miscarriage is four-fold higher.
Some factors have a u-shaped relationship, with the risk of miscarriage and stillbirth lowest in the middle.
For instance, maternal age is a risk factor for both miscarriage and stillbirth, especially if under 20 years old or older than 35. Increasing age of the male is only a risk factor for stillbirth, especially for fathers over 40.
An older dad can be a risk factor for stillbirth, but not miscarriage. Elizaveta Galitckaia/Shutterstock Similarly for maternal bodyweight, women with a body mass index or BMI in the normal range have the lowest risk of miscarriage and stillbirth compared with those in the obese or underweight categories.
Lifestyle factors such as smoking and heavy alcohol drinking while pregnant are also risk factors for both miscarriage and stillbirth.
So it’s important to not only avoid smoking and alcohol while pregnant, but before getting pregnant. This is because early in the pregnancy, women may not know they have conceived and could unwittingly expose the developing fetus.
Why do they happen?
Miscarriage often results from chromosomal problems in the developing fetus. However, genetic conditions or birth defects account for only 7-14% of stillbirths.
Instead, stillbirths often relate directly to pregnancy complications, such as a prolonged pregnancy or problems with the umbilical cord.
Maternal health at the time of pregnancy is another contributing factor in the risk of both miscarriage and stillbirths.
Chronic diseases, such as high blood pressure, diabetes, hypothyroidism (underactive thyroid), polycystic ovary syndrome, problems with the immune system (such as an autoimmune disorder), and some bacterial and viral infections are among factors that can increase the risk of miscarriage.
Similarly mothers with diabetes, high blood pressure, and untreated infections, such as malaria or syphilis, face an increased risk of stillbirth.
In many cases, however, the specific cause of pregnancy loss is not known.
How about the long-term health risks?
Miscarriage and stillbirth can be early indicators of health issues later in life.
For instance, women who have had recurrent miscarriages or recurrent stillbirths are at higher risk of cardiovascular disease (such as heart disease or stroke).
Our research has also looked at the increased risk of stroke. Compared with women who had never miscarried, we found women with a history of three or more miscarriages had a 35% higher risk of non-fatal stroke and 82% higher risk of fatal stroke.
Women who had a stillbirth had a 31% higher risk of a non-fatal stroke, and those who had had two or more stillbirths were at a 26% higher risk of a fatal stroke.
We saw similar patterns in chronic obstructive pulmonary disease or COPD, a progressive lung disease with respiratory symptoms such as breathlessness and coughing.
Our data showed women with a history of recurrent miscarriages or stillbirths were at a 36% or 67% higher risk of COPD, respectively, even after accounting for a history of asthma.
Long-term health risks of recurrent miscarriages or stillbirths include developing lung disease later in life. PRPicturesProduction/Shutterstock Why is all this important?
Being well-informed about the similarities and differences between these two traumatic life events may help explain what has happened to you or a loved one.
Where risk factors can be modified, such as smoking and obesity, this information can be empowering for individuals who wish to reduce their risk of miscarriage and stillbirth and make lifestyle changes before they become pregnant.
More information and support about miscarriage and stillbirth is available from SANDS and Pink Elephants.
Gita Mishra, Professor of Life Course Epidemiology, Faculty of Medicine, The University of Queensland; Chen Liang, PhD student, reproductive history and non-communicable diseases in women, The University of Queensland, and Jenny Doust, Clinical Professorial Research Fellow, School of Public Health, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Yoga for Better Sleep – by Mark Stephens
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book has, as you might expect:
- postural exercises
- breathing exercises
- meditation exercises
Instructions given in all of the above categories are clear and easy to follow, and there are photographic illustrations too where appropriate.
What sets it apart from many books of this kind is that it also has chapters dedicated to various specific circumstances; the many actual reasons people seriously struggle to sleep; not just “screentime too late”, but for example deprepression, sleep apnea, hyperarousal, or even just aging.
As well as the comprehensive exercises, there are also many tips, tricks, hacks, and workarounds—it’s a practical guidebook with practical advice.
While the book is about yogic practices, the author also does tackle this holistically, acknowledging that there are many factors going on, and that yogic practices should be one more string to our sleep-improving bow—as we continue with other general good advice for good sleep too, have medical tests if it seems appropriate, that kind of thing. Basically, to have one’s assorted approaches work together with synergistic effect.
Bottom line: this book will quite possibly put you to sleep! But only in the best possible way.
Click here to check out Yoga for Better Sleep, and get those valuable Zs in, healthily!
Share This Post
Related Posts
-
The “Love Drug”
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Get PEA-Brained!
Today we’ll be looking at phenylethylamine, or PEA, to its friends.
Not to be mistaken for the related amino acid phenylalanine! Both ultimately have effects on the dopaminergic system, but the process and benefits are mostly quite different.
We thought we’d do this one in the week of Valentine’s Day, because of its popular association with love:
❝Phenylethylamine (PEA), an amphetamine-like substance that has been alluringly labeled the “chemical of love,” makes the best case for the love-chocolate connection since it has been shown that people in love may actually have higher levels of PEA in their brain, as surmised from the fact that their urine is richer in a metabolite of this compound. In other words, people thrashing around in the throes of love pee differently from others.❞
Source: Office for Science and Society | The Chemical of Love
What is it?
It’s an amino acid. Because we are mammals, we can synthesize it inside our bodies, so it’s not considered an “essential amino acid”, i.e. one that we need to get from our diet. It is found in some foods, though, including:
- Other animals, especially other mammals
- Various beans, legumes, nuts, seeds. In particular almonds, soybeans, lentils, and chickpeas score highly
- Fermented foods
- Chocolate (popular lore holds this to be a good source of PEA; science finds it to be a fair option, but not in the same ballpark as the other items)
Fun fact: the reason Marvel’s Venom has a penchant for eating humans and chocolate is (according to the comics) because phenylethylamine is an essential amino acid for it.
What does it do for us?
It’s a Central Nervous System (CNS) stimulant, and also helps us synthesize critical neurotransmitters such as dopamine, norepinephrine (adrenaline) and serotonin:
It works similarly, but not identically, to amphetamines:
Is it safe?
We normally do this after the benefits, but “it works similarly to amphetamines” may raise an eyebrow or two, so let’s do it here:
- It is recommended to take no more than 500mg/day, with 100mg–500mg being typical doses
- It is not recommended to take it at all if you have, or have a predisposition to, any kind of psychotic disorder (especially schizophrenia, or bipolar disorder wherein you sometimes experience mania)
- This isn’t a risk for most people, but if you fall into the above category, the elevated dopamine levels could nudge you into a psychotic/manic episode that you probably don’t want.
See for example: Does phenylethylamine cause schizophrenia?
There are other contraindications too, so speak with your doctor/pharmacist before trying it.
On the other hand, if you are considering ADHD medication, then phenylethylamine could be a safer thing to try first, to see if it helps, before going to the heavy guns of actual amphetamines (as are commonly prescribed for ADHD). Same goes for depression and antidepressants.
What can I expect from PEA?
More dopamine, norepinephrine, and serotonin. Mostly the former two. Which means, you can expect stimulation.
For focus and attention, it’s so effective that it has been suggested (as we mentioned above) as a safer alternative to ADHD meds:
β-phenylethylamine, a small molecule with a large impact
…and may give similar benefits to people without ADHD, namely improved focus, attention, and mental stamina:
It also improves mood:
❝Phenylethylamine (PEA), an endogenous neuroamine, increases attention and activity in animals and has been shown to relieve depression in 60% of depressed patients. It has been proposed that PEA deficit may be the cause of a common form of depressive illness.
Effective dosage did not change with time. There were no apparent side effects. PEA produces sustained relief of depression in a significant number of patients, including some unresponsive to the standard treatments. PEA improves mood as rapidly as amphetamine but does not produce tolerance.❞
Source: Sustained antidepressant effect of PEA replacement
Where can I get it?
We don’t sell it, but here is an example product on Amazon for your convenience 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Do Probiotics Work For Weight Loss?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Can you talk about using probiotics for weight loss? Thanks❞
Great question! First, a quick catch-up:
How Much Difference Do Probiotic Supplements Make, Really?
Our above-linked article covers a number of important benefits of probiotic supplements, but we didn’t talk about weight loss at all. So let’s examine whether probiotics are useful for weight loss.
Up-front summary: the science is unclear
This 2021 systematic review found that they are indeed very effective:
❝The intake of probiotics or synbiotics could lead to significant weight reductions, either maintaining habitual lifestyle habits or in combination with energy restriction and/or increased physical activity for an average of 12 weeks.
Specific strains belonging to the genus Lactobacillus and Bifidobacterium were the most used and those that showed the best results in reducing body weight.
Both probiotics and synbiotics have the potential to help in weight loss in overweight and obese populations.❞
This slightly older (2015) systematic review and meta-analysis found the opposite:
❝Collectively, the RCTs examined in this meta-analysis indicated that probiotics have limited efficacy in terms of decreasing body weight and BMI and were not effective for weight loss.❞
Source: Probiotics for weight loss: a systematic review and meta-analysis
And in case that’s not balanced enough, this 2020 randomized controlled trial got mixed results:
❝Regression analysis performed to correlate abundance of species following supplementation with body composition parameters and biomarkers of obesity found an association between a decrease over time in blood glucose and an increase in Lactobacillus abundance, particularly in the synbiotic group.
However, the decrease over time in body mass, BMI, waist circumstance, and body fat mass was associated with a decrease in Bifidobacterium abundance.❞
Source: Effects of Synbiotic Supplement on Human Gut Microbiota, Body Composition and Weight Loss in Obesity
Summary
Probiotics may or may not work for weight loss.
In all likelihood, it depends on the blend of cultures contained in the supplement. It’s possible that Lactobacillus is more beneficial for weight loss than Bifidobacterium, which latter may actually reduce weight loss.
Or it might not, because that was just one study and correlation ≠ causation!
We’d love to give you a hard-and-fast answer, but if the data doesn’t support a hard-and-fast answer, we’re not going to lie to you.
What we can say for sure though is that probiotics come with very many health benefits, so whether or not weight loss is one of them, they’re a good thing to have for most people.
Some further articles that may interest you:
- How Much Difference Do Probiotic Supplements Make, Really? ← the aforementioned article
- Making Friends With Your Gut (You Can Thank Us Later) ← gut health 101
- Burn! How To Boost Your Metabolism ← these things can help change your metabolic base rate, which is highly relevant to weight loss
- How To Do HIIT (Without Wrecking Your Body) ←unlike most forms of exercise, which cause the body to slow the metabolism afterwards to compensate, high-intensity interval training results in an increased metabolic rate (so generally: fat-burning) for several hours after training.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What you need to know about H5N1 bird flu
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
On May 30, the Centers for Disease Control and Prevention reported that a Michigan dairy worker tested positive for H5N1 bird flu. It was the fourth person to test positive for H5N1 in the United States, following another recent case in Michigan, an April case in Texas, and an initial case in Colorado in 2022.
H5N1 bird flu has been spreading among bird species in the U.S. since 2021, killing millions of wild birds and poultry. In late March 2024, H5N1 bird flu was found in cows for the first time, causing an outbreak in dairy cows across several states.
U.S. public health officials and researchers are particularly concerned about this outbreak because the virus has infected cows and other mammals and has spread from a cow to a human for the first time.
This bird flu strain has shown to not only make wild mammals, including marine mammals and bears, very sick but to also cause high rates of death among species, says Jane Sykes, professor of small animal medicine at the University of California, Davis, School of Veterinary Medicine.
“And now that it has been found in cattle, [it] raises particular concern for spread to all the animal species, including people,” adds Sykes.
Even though the risk for human infection is low and there has never been human-to-human transmission of H5N1, there are several actions you can take to stay protected. Read on to learn more about H5N1 bird flu and the current outbreak.
What is H5N1?
H5N1 is a type of influenza virus that most commonly affects birds, causing them severe respiratory illness and death.
The H5N1 strain first emerged in China in the 1990s, and it has continued to spread around the world since then. In 1997, the virus spread from animals to humans in Hong Kong for the first time, infecting 18 people, six of whom died.
Since 2020, the H5N1 strain has caused “an unprecedented number of deaths in wild birds and poultry in many countries,” according to the World Health Organization.
Even though bird flu is rare in humans, an H5N1 infection can cause mild to severe illness and can be fatal in some cases. It can cause eye infection, upper respiratory symptoms, and pneumonia.
What do we know about the 2024 human cases of H5N1 in the U.S.?
The Michigan worker who tested positive for H5N1 in late May is a dairy worker who was exposed to infected livestock. They were the first to experience respiratory symptoms—including a cough without a fever—during the current outbreak. They were given an antiviral and the CDC says their symptoms are resolving.
The Michigan farm worker who tested positive earlier in May only experienced eye-related symptoms and has already recovered. And the dairy worker who tested positive for the virus in Texas in April only experienced eye redness as well, was treated with an antiviral medication for the flu, and is recovering.
Is H5N1 bird flu in the milk we consume?
The Food and Drug Administration has found traces of H5N1 bird flu virus in raw or unpasteurized milk. However, pasteurized milk is safe to drink.
Pasteurization, the process of heating milk to high temperatures to kill harmful bacteria (which the majority of commercially sold milk goes through), deactivates the virus. In 20 percent of pasteurized milk samples, the FDA found small, inactive (not live nor infectious) traces of the virus, but these fragments do not make pasteurized milk dangerous.
In a recent Infectious Diseases Society of America briefing, Dr. Maximo Brito, a professor at the University of Illinois College of Medicine, said that it’s important for people to avoid “drinking unpasteurized or raw milk [because] there are other diseases, not only influenza, that could be transmitted by drinking unpasteurized milk.”
What can I do to prevent bird flu?
While the risk of H5N1 infection in humans is low, people with exposure to infected animals (like farmworkers) are most at risk. But there are several actions you can take to stay protected.
One of the most important things, according to Sykes, is taking the usual precautions we’ve taken with COVID-19 and other respiratory viruses, including frequent handwashing, especially before eating.
“Handwashing and mask-wearing [are important], just as we learned from the pandemic,” Sykes adds. “And it’s not wearing a mask at all times, but thinking about high-risk situations, like when you’re indoors in a crowded environment, where transmission of respiratory viruses is much more likely to occur.”
There are other steps you can take to prevent H5N1, according to the CDC:
- Avoid direct contact with sick or dead animals, including wild birds and poultry.
- Don’t touch surfaces that may have been contaminated with animal poop, saliva, or mucus.
- Cook poultry and eggs to an internal temperature of 165 degrees Fahrenheit to kill any bacteria or virus, including H5N1. Generally, avoid eating undercooked food.
- Avoid consuming unpasteurized or raw milk or products like cheeses made with raw milk.
- Avoid eating uncooked or undercooked food.
- Poultry and livestock farmers and workers and bird flock owners should wear masks and other personal protective equipment “when in direct or close physical contact with sick birds, livestock, or other animals; carcasses; feces; litter; raw milk; or surfaces and water that might be contaminated with animal excretions from potentially or confirmed infected birds, livestock, or other animals.” (The CDC has more recommendations for this population here.)
Is there a vaccine for H5N1?
The CDC said there are two candidate H5N1 vaccines ready to be made and distributed in case the virus starts to spread from person to person, and the country is now moving forward with plans to produce millions of vaccine doses.
The FDA has approved several bird flu vaccines since 2007. The U.S. has flu vaccines in stockpile through the National Pre-Pandemic Influenza Vaccine Stockpile program, which allows for quick response as strains of the flu virus evolve.
Could this outbreak become a pandemic?
Scientists and researchers are concerned about the possibility of H5N1 spreading among people and causing a pandemic. “Right now, the risk is low, but as time goes on, the potential for mutation to cause widespread human infection increases,” says Sykes.
“I think this virus jumping into cows has shown the urgency to keep tracking [H5N1] a lot more closely now,” Peter Halfmann, research associate professor at the University of Wisconsin-Madison’s Influenza Research Institute tells PGN. “We have our eyes on surveillance now. … We’re keeping a much closer eye, so it’s not going to take us by surprise.”
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: