What you need to know about menopause
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Menopause describes the time when a person with ovaries has gone one full year without a menstrual period. Reaching this phase is a natural aging process that marks the end of reproductive years.
Read on to learn more about the causes, stages, signs, and management of menopause.
What causes menopause?
As you age, your ovaries begin making less estrogen and progesterone—two of the hormones involved in menstruation—and your fertility declines, causing menopause.
Most people begin perimenopause, the transitional time that ends in menopause, in their late 40s, but it can start earlier. On average, people in the U.S. experience menopause in their early 50s.
Your body may reach early menopause for a variety of reasons, including having an oophorectomy, a surgery that removes the ovaries. In this case, the hormonal changes happen abruptly rather than gradually.
Chemotherapy and radiation therapy for cancer patients may also induce menopause, as these treatments may impact ovary function.
What are the stages of menopause?
There are three stages:
- Perimenopause typically occurs eight to 10 years before menopause happens. During this stage, estrogen production begins to decline and ovaries release eggs less frequently.
- Menopause marks the point when you have gone 12 consecutive months without a menstrual period. This means the ovaries have stopped releasing eggs and producing estrogen.
- Postmenopause describes the time after menopause. Once your body reaches this phase, it remains there for the rest of your life.
How do the stages of menopause affect fertility?
Your ovaries still produce eggs during perimenopause, so it is still possible to get pregnant during that stage. If you do not wish to become pregnant, continue using your preferred form of birth control throughout perimenopause.
Once you’ve reached menopause, you can no longer get pregnant naturally. People who would like to become pregnant after that may pursue in vitro fertilization (IVF) using eggs that were frozen earlier in life or donor eggs.
What are the signs of menopause?
Hormonal shifts result in a number of bodily changes. Signs you are approaching menopause may include:
- Hot flashes (a sudden feeling of warmth).
- Irregular menstrual periods, or unusually heavy or light menstrual periods.
- Night sweats and/or cold flashes.
- Insomnia.
- Slowed metabolism.
- Irritability, mood swings, and depression.
- Vaginal dryness.
- Changes in libido.
- Dry skin, eyes, and/or mouth.
- Worsening of premenstrual syndrome (PMS).
- Urinary urgency (a sudden need to urinate).
- Brain fog.
How can I manage the effects of menopause?
You may not need any treatment to manage the effects of menopause. However, if the effects are disrupting your life, your doctor may prescribe hormone therapy.
If you have had a hysterectomy, your doctor may prescribe estrogen therapy (ET), which may be administered via a pill, patch, cream, spray, or vaginal ring. If you still have a uterus, your doctor may prescribe estrogen progesterone/progestin hormone therapy (EPT), which is sometimes called “combination therapy.”
Both of these therapies work by replacing the hormones your body has stopped making, which can reduce the physical and mental effects of menopause.
Other treatment options may include antidepressants, which can help manage mood swings and hot flashes; prescription creams to alleviate vaginal dryness; or gabapentin, an anti-seizure medication that has been shown to reduce hot flashes.
Lifestyle changes may help alleviate the effects on their own or in combination with prescription medication. Those changes include:
- Incorporating movement into your daily life.
- Limiting caffeine and alcohol.
- Quitting smoking.
- Maintaining a regular sleep schedule.
- Practicing relaxation techniques, such as meditation.
- Consuming foods rich in plant estrogens, such as grains, beans, fruits, vegetables, and seeds.
- Seeking support from a therapist and from loved ones.
What health risks are associated with menopause?
Having lower levels of estrogen may put you at greater risk of certain health complications, including osteoporosis and coronary artery disease.
Osteoporosis occurs when bones lose their density, increasing the risk of fractures. A 2022 study found that the prevalence of osteoporotic fractures in postmenopausal women was 82.2 percent.
Coronary artery disease occurs when the arteries that send blood to your heart become narrow or blocked with fatty plaque.
Estrogen therapy can reduce your risk of osteoporosis and coronary artery disease by preserving bone mass and maintaining cardiovascular function.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Red Lentils vs Green Lentils – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing red lentils to green lentils, we picked the green.
Why?
Yes, they’re both great. But there are some clear distinctions!
First, know: red lentils are, secretly, hulled brown lentils. Brown lentils are similar to green lentils, just a little less popular and with (very) slightly lower nutritional values, as a rule.
By hulling the lentils, the first thing that needs mentioning is that they lose some of their fiber, since this is what was removed. While we’re talking macros, this does mean that red lentils have proportionally more protein, because of the fiber weight lost. However, because green lentils are still a good source of protein, we think the fat that green lentils have much more fiber is a point in their favor.
In terms of micronutrients, they’re quite similar in vitamins (mostly B-vitamins, of which, mostly folate / vitamin B9), and when it comes to minerals, they’re similarly good sources of iron, but green lentils contain more magnesium and potassium.
Green lentils also contain more antixoidants.
All in all, they both continue to be very respectable parts of anyone’s diet—but in a head-to-head, green lentils do come out on top (unless you want to prioritize slightly higher protein above everything else, in which case, red).
Want to get some in? Here are the specific products we featured today:
Enjoy!
Want to learn more?
You might like to read:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Eat More (Of This) For Lower Blood Pressure ← incidentally, the potassium content of green lentils also helps minimize the harm done by sodium in one’s diet
Take care!
Share This Post
-
Clams vs Oysters – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing clams to oysters, we picked the clams.
Why?
Considering the macros first, clams have more than 2x the protein, while oysters have nearly 2x the fat, of which, a little over 5x the saturated fat. So, in all accounts, clam is the winner here.
In terms of vitamins, clams have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, B12, and C, while oysters are not higher in any vitamins. Another win for clams.
The category of minerals is more balanced; clams are higher in manganese, phosphorus, potassium, and selenium, while oysters are higher in copper, iron, magnesium, and zinc. This makes for a 4:4 tie, though it’s worth noting that the margin of difference for zinc is very large, so that can be an argument for oysters.
Nevertheless, adding up the sections makes for a clear win for clams.
A quick aside on “are oysters an aphrodisiac?”:
That zinc content is probably largely responsible for oysters’ reputation as an aphrodisiac, and zinc is important in the synthesis of both estrogen and testosterone. However, as the synthesis is not instant, and those sex hormones rise most in the morning (around 8am to 9am), to enjoy aphrodisiac benefits it’d be more sensible, on a biochemical level, to eat oysters one day, and then have morning sex the next day when those hormones are peaking. That said, while testosterone is the main driver of male libido, progesterone is usually more relevant for women’s, and unlike estrogen, progesterone usually peaks around 10pm to 2am, and is uninfluenced by having just eaten oysters.
So, in what way, if any, could oysters be responsible for libido in women? Well, the zinc is still important in energy metabolism, so that’s a factor, and also, we might hypothesize that oysters’ high saturated fat and cholesterol content may increase blood pressure which, while not fabulous for the health in general, may be considered desirable in the bedroom since the clitoris is anatomically analogous to the penis, and—while estrogen vs testosterone makes differences to the nervous system down there that are beyond the scope of today’s article—also enjoys localized increased blood pressure (and thus, a flushing response and resultant engorgement) during arousal.
Want to learn more?
You might like to read:
Does Eating Shellfish Really Contribute To Gout? ← short answer is: it can if consumed frequently over a long period of time, but that risk factor is greatly overstated, compared to some other risk factors
Take care!
Share This Post
-
Hot And Sour Shiitake Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a popular, easy, and delicious soup that nonetheless is not found in many western kitchens, despite being enjoyed in restaurants/take-out. Best of all, making it at home means that you know all the ingredients, can account for quality, and also can customize it per your preferences (i.e. how much heat/sourness you like).
You will need
- 3 cups shiitake mushrooms, sliced
- 3 cups bok choy, chopped
- 2 cups cherry tomatoes, quartered
- 1 cup carrot, grated
- 3 spring onions, chopped
- 2 shallots, sliced lengthways
- 2 serrano chilis (or similar), sliced thinly
- 2 tbsp apple cider vinegar
- 1 tbsp lemon juice
- 1 tbsp fresh ginger, sliced into 1″ strips
- 1 tsp black pepper, coarse ground
- ½ bulb garlic, crushed
- 6 cups low-sodium vegetable stock. Ideally you will have made it yourself from vegetable cuttings that you saved in the freezer until you had enough to make stock from, but if that’s not an option, then low-sodium vegetable stock cubes can be purchased and used.
- Garnish: ¼ cup (or 4 tbsp) cilantro, chopped, or if you have the soap gene, then this time we recommend chopped basil as the subsitution
Method
(we suggest you read everything at least once before doing anything)
1) Put the ginger in a big pot with the stock; cover and simmer for about 20 minutes (otherwise the ginger flavor will remain mostly concentrated in the ginger strips).
2) Bring it to a boil and add the bok choy, mushrooms, shallots, chili peppers, and the carrot; simmer for another 5 minutes
3) Add the remaining ingredients except for the garnish, and simmer for another 5 minutes
4) Serve, adding the garnish
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- The (Longevity) Magic of Mushrooms
- Our Top 5 Spices: How Much Is Enough For Benefits?
- An Apple (Cider Vinegar) A Day…
- Enjoy Bitter/Hot/Sour/Pungent Foods For Your Heart & Brain
- Brain Food? The Eyes Have It!
- Some Surprising Truths About Hunger And Satiety
Take care!
Share This Post
Related Posts
-
How To En-Joy Life (With Long-Term Benefits)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
New Year’s Dissolutions?
We have talked previously about:
The Science Of New Year’s Pre-Resolutions
…and here we are now at the end of the first week of January; how’s it going?
Hopefully, based on that article, it’s been going just great since December! For most people, statistically speaking, it hasn’t.
Around now is typically when many people enter the “bargaining” stage of New Year’s Resolutions, which at this point are often in serious danger of becoming New Year’s Dissolutions.
What’s important, really?
When trying to juggle potentially too many new items, it’s important to be able to decide where to focus one’s efforts in the case of needing to drop a ball or two.
First, the laziest way…
The path of least resistance
This is perhaps most people’s go-to. It, without too much thought, drops whatever feels most onerous, and continues with what seems easiest.
This is not a terrible approach, because what we enjoy, we will be more likely to continue. But it can be improved upon, while still getting that benefit.
Marie Kondo your
resolutionsvaluesInstead of throwing out the new habits that “don’t spark joy”, ask yourself:
“What brings me joy?”
…because often, the answer is something that’s a result of a thing that didn’t “spark joy” directly. Many things in life involve delayed gratification.
Let’s separate the [unwanted action] from the [wanted result] for a moment.
Rather than struggling on with something unpleasant for the hope of joy at the end of the rainbow, though, give yourself permission to improve the middle bit.
For example, if the idea of having lots of energy and good cardiovascular fitness is what prompted you to commit to those 6am runs each morning (but they’re not actually joyous in your experience), what would be more fun and still give you the same benefit?
Now that you know “having lots of energy and good CV fitness” is what sparks joy, not “getting up to run at 6am”, you can change lanes without pulling off the highway entirely.
Maybe a dance class will be more your speed, for example.
The key here is: you’ll have changed your resolution, without breaking it in any way that mattered
Want more ways to keep on track without burning out?
Who doesn’t? So, check out:
How To Keep On Keeping On… Long Term!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Doctors Are as Vulnerable to Addiction as Anyone. California Grapples With a Response
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
BEVERLY HILLS, Calif. — Ariella Morrow, an internal medicine doctor, gradually slid from healthy self-esteem and professional success into the depths of depression.
Beginning in 2015, she suffered a string of personal troubles, including a shattering family trauma, marital strife, and a major professional setback. At first, sheer grit and determination kept her going, but eventually she was unable to keep her troubles at bay and took refuge in heavy drinking. By late 2020, Morrow could barely get out of bed and didn’t shower or brush her teeth for weeks on end. She was up to two bottles of wine a day, alternating it with Scotch whisky.
Sitting in her well-appointed home on a recent autumn afternoon, adorned in a bright lavender dress, matching lipstick, and a large pearl necklace, Morrow traced the arc of her surrender to alcohol: “I’m not going to drink before 5 p.m. I’m not going to drink before 2. I’m not going to drink while the kids are home. And then, it was 10 o’clock, 9 o’clock, wake up and drink.”
As addiction and overdose deaths command headlines across the nation, the Medical Board of California, which licenses MDs, is developing a new program to treat and monitor doctors with alcohol and drug problems. But a fault line has appeared over whether those who join the new program without being ordered to by the board should be subject to public disclosure.
Patient advocates note that the medical board’s primary mission is “to protect healthcare consumers and prevent harm,” which they say trumps physician privacy.
The names of those required by the board to undergo treatment and monitoring under a disciplinary order are already made public. But addiction medicine professionals say that if the state wants troubled doctors to come forward without a board order, confidentiality is crucial.
Public disclosure would be “a powerful disincentive for anybody to get help” and would impede early intervention, which is key to avoiding impairment on the job that could harm patients, said Scott Hambleton, president of the Federation of State Physician Health Programs, whose core members help arrange care and monitoring of doctors for substance use disorders and mental health conditions as an alternative to discipline.
But consumer advocates argue that patients have a right to know if their doctor has an addiction. “Doctors are supposed to talk to their patients about all the risks and benefits of any treatment or procedure, yet the risk of an addicted doctor is expected to remain a secret?” Marian Hollingsworth, a volunteer advocate with the Patient Safety Action Network, told the medical board at a Nov. 14 hearing on the new program.
Doctors are as vulnerable to addiction as anyone else. People who work to help rehabilitate physicians say the rate of substance use disorders among them is at least as high as the rate for the general public, which the federal Substance Abuse and Mental Health Services Administration put at 17.3% in a Nov. 13 report.
Alcohol is a very common drug of choice among doctors, but their ready access to pain meds is also a particular risk.
“If you have an opioid use disorder and are working in an operating room with medications like fentanyl staring you down, it’s a challenge and can be a trigger,” said Chwen-Yuen Angie Chen, an addiction medicine doctor who chairs the Well-Being of Physicians and Physicians-in-Training Committee at Stanford Health Care. “It’s like someone with an alcohol use disorder working at a bar.”
From Pioneer to Lagger
California was once at the forefront of physician treatment and monitoring. In 1981, the medical board launched a program for the evaluation, treatment, and monitoring of physicians with mental illness or substance use problems. Participants were often required to take random drug tests, attend multiple group meetings a week, submit to work-site surveillance by colleagues, and stay in the program for at least five years. Doctors who voluntarily entered the program generally enjoyed confidentiality, but those ordered into it by the board as part of a disciplinary action were on the public record.
The program was terminated in 2008 after several audits found serious flaws. One such audit, conducted by Julianne D’Angelo Fellmeth, a consumer interest lawyer who was chosen as an outside monitor for the board, found that doctors in the program were often able to evade the random drug tests, attendance at mandatory group therapy sessions was not accurately tracked, and participants were not properly monitored at work sites.
Today, MDs who want help with addiction can seek private treatment on their own or in many cases are referred by hospitals and other health care employers to third parties that organize treatment and surveillance. The medical board can order a doctor on probation to get treatment.
In contrast, the California licensing boards of eight other health-related professions, including osteopathic physicians, registered nurses, dentists, and pharmacists, have treatment and monitoring programs administered under one master contract by a publicly traded company called Maximus Inc. California paid Maximus about $1.6 million last fiscal year to administer those programs.
When and if the final medical board regulations are adopted, the next step would be for the board to open bidding to find a program administrator.
Fall From Grace
Morrow’s troubles started long after the original California program had been shut down.
The daughter of a prominent cosmetic surgeon, Morrow grew up in Palm Springs in circumstances she describes as “beyond privileged.” Her father, David Morrow, later became her most trusted mentor.
But her charmed life began to fall apart in 2015, when her father and mother, Linda Morrow, were indicted on federal insurance fraud charges in a well-publicized case. In 2017, the couple fled to Israel in an attempt to escape criminal prosecution, but later they were both arrested and returned to the United States to face prison sentences.
The legal woes of Morrow’s parents, later compounded by marital problems related to the failure of her husband’s business, took a heavy toll on Morrow. She was in her early 30s when the trouble with her parents started, and she was working 16-hour days to build a private medical practice, with two small children at home. By the end of 2019, she was severely depressed and turning increasingly to alcohol. Then, the loss of her admitting privileges at a large Los Angeles hospital due to inadequate medical record-keeping shattered what remained of her self-confidence.
Morrow, reflecting on her experience, said the very strengths that propel doctors through medical school and keep them going in their careers can foster a sense of denial. “We are so strong that our strength is our greatest threat. Our power is our powerlessness,” she said. Morrow ignored all the flashing yellow lights and even the red light beyond which serious trouble lay: “I blew through all of it, and I fell off the cliff.”
By late 2020, no longer working, bedridden by depression, and drinking to excess, she realized she could no longer will her way through: “I finally said to my husband, ‘I need help.’ He said, ‘I know you do.’”
Ultimately, she packed herself off to a private residential treatment center in Texas. Now sober for 21 months, Morrow said the privacy of the addiction treatment she chose was invaluable because it shielded her from professional scrutiny.
“I didn’t have to feel naked and judged,” she said.
Morrow said her privacy concerns would make her reluctant to join a state program like the one being considered by the medical board.
Physician Privacy vs. Patient Protection
The proposed regulations would spare doctors in the program who were not under board discipline from public disclosure as long as they stayed sober and complied with all the requirements, generally including random drug tests, attendance at group sessions, and work-site monitoring. If the program put a restriction on a doctor’s medical license, it would be posted on the medical board’s website, but without mentioning the doctor’s participation in the program.
Yet even that might compromise a doctor’s career since “having a restricted license for unspecified reasons could have many enduring personal and professional implications, none positive,” said Tracy Zemansky, a clinical psychologist and president of the Southern California division of Pacific Assistance Group, which provides support and monitoring for physicians.
Zemansky and others say doctors, just like anyone else, are entitled to medical privacy under federal law, as long as they haven’t caused harm.
Many who work in addiction medicine also criticized the proposed new program for not including mental health problems, which often go hand in hand with addiction and are covered by physician health programs in other states.
“To forgo mental health treatment, I think, is a grave mistake,” Morrow said. For her, depression and alcoholism were inseparable, and the residential program she attended treated her for both.
Another point of contention is money. Under the current proposal, doctors would bear all the costs of the program.
The initial clinical evaluation, plus the regular random drug tests, group sessions, and monitoring at their work sites could cost participants over $27,000 a year on average, according to estimates posted by the medical board. And if they were required to go for 30-day inpatient treatment, that would add an additional $40,000 — plus nearly $36,000 in lost wages.
People who work in the field of addiction medicine believe that is an unfair burden. They note that most programs for physicians in other states have outside funding to reduce the cost to participants.
“The cost should not be fully borne by the doctors, because there are many other people that are benefiting from this, including the board, malpractice insurers, hospitals, the medical association,” said Greg Skipper, a semi-retired addiction medicine doctor who ran Alabama’s state physician health program for 12 years. In Alabama, he said, those institutions contribute to the program, significantly cutting the amount doctors have to pay.
The treatment program that Morrow attended in spring of 2021, at The Menninger Clinic in Houston, cost $80,000 for a six-week stay, which was covered by a concerned family member. “It saved my life,” she said.
Though Morrow had difficulty maintaining her sobriety in the first year after treatment, she has now been sober since April 2, 2022. These days, Morrow regularly attends therapy and Alcoholics Anonymous and has pivoted to become an addiction medicine doctor.
“I am a better doctor today because of my experience — no question,” Morrow said. “I am proud to be a doctor who’s an alcoholic in recovery.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
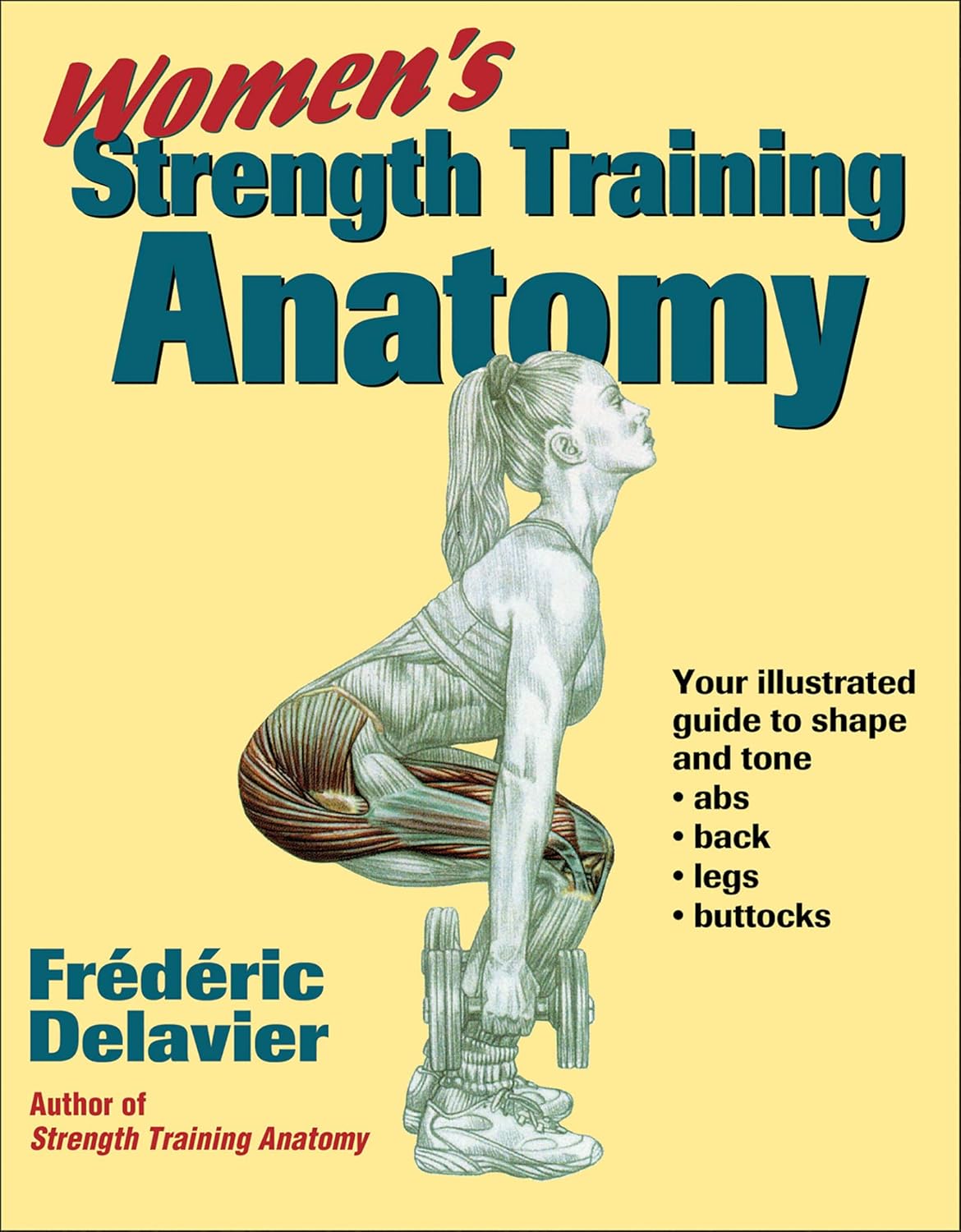
Women’s Strength Training Anatomy – by Frédéric Delavier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fitness guides for women tend to differ from fitness guides for men, in the wrong ways:
“Do some squats and jumping jacks, and here’s a exercise for your abs; you too can look like our model here”
In those other books we are left wonder: where’s the underlying information? Where are the explanations that aren’t condescending? Where, dare we ask, is the understanding that a woman might ever lift something heavier than a baby?
Delavier, in contrast, delivers. With 130 pages of detailed anatomical diagrams for all kinds of exercises to genuinely craft your body the way you want it for you. Bigger here, smaller there, functional strength, you decide.
And rest assured: no, you won’t end up looking like Arnold Schwarzenegger unless you not only eat like him, but also have his genes (and possibly his, uh, “supplement” regime).
What you will get though, is a deep understanding of how to tailor your exercise routine to actually deliver the personalized and specific results that you want.
Pick Up Today’s Book on Amazon!
Not looking for a feminine figure? You may like the same author’s book for men:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: