What Macronutrient Balance Is Right For You?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I want to learn more about macros. Can you cover that topic?❞
That’s a little broader than we usually go for, given the amount of space we have, but let’s give it a go!
Macronutrients, or “macros”, are the nutrients that we typically measure in grams rather than milligrams or micrograms, and are:
- Carbohydrates
- …and what kinds, of which usually the focus is on how much is sugars as opposed to more complex carbs that take longer to break down. See also: Should You Go Light Or Heavy On Carbs?
- …and of the sugars, the interested may further categorize them into sucrose, fructose, etc. See also: Which Sugars Are Healthier, And Which Are Just The Same?
- Proteins
- …of which, the amino acid make-up is generally considered a matter of micronutrients. See also: Protein: How Much Do We Need, Really?
- Fats
- …and what kinds, i.e. monounsaturated vs polyunsaturated vs saturated. See also: Saturated Fat: What’s The Truth?
- …and then the interested may further categorize them for their fatty acids / triglycerides profile, etc. See also: What Omega-3 Fatty Acids Really Do For Us
- Fiber
- …which often gets ignored by people counting macros, as “stuff that doesn’t do anything”, despite it in fact being very important for health. See also: Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Water
- …which again tends to get disregarded but is very arguably a critical macronutrient. See also: Busting The Myth of “Eight Glasses Of Water A Day”
In terms of how much we need of each, you can read more in the above-linked articles, but:
- General scientific consensus is we need plenty of fiber (30 or 40g per day is good) and water (highly dependent on climate and activity), and there’s a clear minimum requisite for protein (usually put at around 1g of protein per day per 1kg of body weight).
- There is vigorous debate in the general health community about what the best ratio of carbs to fat is.
The reality is that humans are quite an adaptable species, and while we absolutely do need at least some of both (carbohydrates and fats), we can play around with the ratios quite a bit, provided we don’t get too extreme about it.
While some influence is social and often centered around weight loss (see for example keto which seeks to minimize carbs, and volumetrics, which seeks maximise volume-to-calorie ratio, which de facto tends to minimize fats), some of what drives us to lean one way or the other will be genetics, too—dependent on what our ancestors ate more or less of.
Writer’s example: my ancestors could not grow much grain (or crops in general) where they were, so they got more energy from such foods as whale and seal fat (with protein coming more from reindeer). Now, biology is not destiny, and I personally enjoy a vegan diet, but my genes are probably why I am driven to get most of my daily calories from fat (of which, a lot of fatty nuts (don’t tell almonds, but I prefer walnuts and cashews) and healthy oils such as olive oil, avocado oil, and coconut oil).
However! About that adaptability. Provided we make changes slowly, we can usually adjust our diet to whatever we want it to be, including whether we get our energy more from carbs or fats. The reason we need to make changes slowly is because our gut needs time to adjust. For example, if your vegan writer here were to eat her ancestrally-favored foods now, I’d be very ill, because my gut microbiome has no idea what to do with animal products anymore, no matter what genes I have. In contrast, if an enthusiastic enjoyer of a meat-heavy diet were to switch to my fiber-rich diet overnight, they’d be very ill.
So: follow your natural inclinations, make any desired changes slowly, and if in doubt, it’s hard to go wrong with enjoying carbs and fats in moderation.
Learn more: Intuitive Eating Might Not Be What You Think
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Can Medical Schools Funnel More Doctors Into the Primary Care Pipeline?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Throughout her childhood, Julia Lo Cascio dreamed of becoming a pediatrician. So, when applying to medical school, she was thrilled to discover a new, small school founded specifically to train primary care doctors: NYU Grossman Long Island School of Medicine.
Now in her final year at the Mineola, New York, school, Lo Cascio remains committed to primary care pediatrics. But many young doctors choose otherwise as they leave medical school for their residencies. In 2024, 252 of the nation’s 3,139 pediatric residency slots went unfilled and family medicine programs faced 636 vacant residencies out of 5,231 as students chased higher-paying specialties.
Lo Cascio, 24, said her three-year accelerated program nurtured her goal of becoming a pediatrician. Could other medical schools do more to promote primary care? The question could not be more urgent. The Association of American Medical Colleges projects a shortage of 20,200 to 40,400 primary care doctors by 2036. This means many Americans will lose out on the benefits of primary care, which research shows improves health, leading to fewer hospital visits and less chronic illness.
Many medical students start out expressing interest in primary care. Then they end up at schools based in academic medical centers, where students become enthralled by complex cases in hospitals, while witnessing little primary care.
The driving force is often money, said Andrew Bazemore, a physician and a senior vice president at the American Board of Family Medicine. “Subspecialties tend to generate a lot of wealth, not only for the individual specialists, but for the whole system in the hospital,” he said.
A department’s cache of federal and pharmaceutical-company grants often determines its size and prestige, he said. And at least 12 medical schools, including Harvard, Yale, and Johns Hopkins, don’t even have full-fledged family medicine departments. Students at these schools can study internal medicine, but many of those graduates end up choosing subspecialties like gastroenterology or cardiology.
One potential solution: eliminate tuition, in the hope that debt-free students will base their career choice on passion rather than paycheck. In 2024, two elite medical schools — the Albert Einstein College of Medicine and the Johns Hopkins University School of Medicine — announced that charitable donations are enabling them to waive tuition, joining a handful of other tuition-free schools.
But the contrast between the school Lo Cascio attends and the institution that founded it starkly illustrates the limitations of this approach. Neither charges tuition.
In 2024, two-thirds of students graduating from her Long Island school chose residencies in primary care. Lo Cascio said the tuition waiver wasn’t a deciding factor in choosing pediatrics, among the lowest-paid specialties, with an average annual income of $260,000, according to Medscape.
At the sister school, the Manhattan-based NYU Grossman School of Medicine, the majority of its 2024 graduates chose specialties like orthopedics (averaging $558,000 a year) or dermatology ($479,000).
Primary care typically gets little respect. Professors and peers alike admonish students: If you’re so smart, why would you choose primary care? Anand Chukka, 27, said he has heard that refrain regularly throughout his years as a student at Harvard Medical School. Even his parents, both PhD scientists, wondered if he was wasting his education by pursuing primary care.
Seemingly minor issues can influence students’ decisions, Chukka said. He recalls envying the students on hospital rotations who routinely were served lunch, while those in primary care settings had to fetch their own.
Despite such headwinds, Chukka, now in his final year, remains enthusiastic about primary care. He has long wanted to care for poor and other underserved people, and a one-year clerkship at a community practice serving low-income patients reinforced that plan.
When students look to the future, especially if they haven’t had such exposure, primary care can seem grim, burdened with time-consuming administrative tasks, such as seeking prior authorizations from insurers and grappling with electronic medical records.
While specialists may also face bureaucracy, primary care practices have it much worse: They have more patients and less money to hire help amid burgeoning paperwork requirements, said Caroline Richardson, chair of family medicine at Brown University’s Warren Alpert Medical School.
“It’s not the medical schools that are the problem; it’s the job,” Richardson said. “The job is too toxic.”
Kevin Grumbach, a professor of family and community medicine at the University of California-San Francisco, spent decades trying to boost the share of students choosing primary care, only to conclude: “There’s really very little that we can do in medical school to change people’s career trajectories.”
Instead, he said, the U.S. health care system must address the low pay and lack of support.
And yet, some schools find a way to produce significant proportions of primary care doctors — through recruitment and programs that provide positive experiences and mentors.
U.S. News & World Report recently ranked 168 medical schools by the percentage of graduates who were practicing primary care six to eight years after graduation.
The top 10 schools are all osteopathic medical schools, with 41% to 47% of their students still practicing primary care. Unlike allopathic medical schools, which award MD degrees, osteopathic schools, which award DO degrees, have a history of focusing on primary care and are graduating a growing share of the nation’s primary care physicians.
At the bottom of the U.S. News list is Yale, with 10.7% of its graduates finding lasting careers in primary care. Other elite schools have similar rates: Johns Hopkins, 13.1%; Harvard, 13.7%.
In contrast, public universities that have made it a mission to promote primary care have much higher numbers.
The University of Washington — No. 18 in the ranking, with 36.9% of graduates working in primary care — has a decades-old program placing students in remote parts of Washington, Wyoming, Alaska, Montana, and Idaho. UW recruits students from those areas, and many go back to practice there, with more than 20% of graduates settling in rural communities, according to Joshua Jauregui, assistant dean for clinical curriculum.
Likewise, the University of California-Davis (No. 22, with 36.3% of graduates in primary care) increased the percentage of students choosing family medicine from 12% in 2009 to 18% in 2023, even as it ranks high in specialty training. Programs such as an accelerated three-year primary care “pathway,” which enrolls primarily first-generation college students, help sustain interest in non-specialty medical fields.
The effort starts with recruitment, looking beyond test scores to the life experiences that forge the compassionate, humanistic doctors most needed in primary care, said Mark Henderson, associate dean for admissions and outreach. Most of the students have families who struggle to get primary care, he said. “So they care a lot about it, and it’s not just an intellectual, abstract sense.”
Establishing schools dedicated to primary care, like the one on Long Island, is not a solution in the eyes of some advocates, who consider primary care the backbone of medicine and not a separate discipline. Toyese Oyeyemi Jr., executive director of the Social Mission Alliance at the Fitzhugh Mullan Institute of Health Workforce Equity, worries that establishing such schools might let others “off the hook.”
Still, attending a medical school created to produce primary care doctors worked out well for Lo Cascio. Although she underwent the usual specialty rotations, her passion for pediatrics never flagged — owing to her 23 classmates, two mentors, and her first-year clerkship shadowing a community pediatrician. Now, she’s applying for pediatric residencies.
Lo Cascio also has deep personal reasons: Throughout her experience with a congenital heart condition, her pediatrician was a “guiding light.”
“No matter what else has happened in school, in life, in the world, and medically, your pediatrician is the person that you can come back to,” she said. “What a beautiful opportunity it would be to be that for someone else.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
Easy Quinoa Falafel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Falafel is a wonderful snack or accompaniment to a main, and if you’ve only had shop-bought, you’re missing out. Plus, with this quinoa-based recipe, it’s almost impossible to accidentally make them dry.
You will need
- 1 cup cooked quinoa
- 1 cup chopped fresh parsley
- ½ cup wholewheat breadcrumbs (or rye breadcrumbs if you’re avoiding wheat/gluten)
- 1 can chickpeas, drained
- 4 green onions, chopped
- ½ bulb garlic, minced
- 2 tbsp extra virgin olive oil, plus more for frying
- 2 tbsp tomato paste
- 1 tbsp apple cider vinegar
- 2 tsp nutritional yeast
- 2 tsp ground cumin
- 1 tsp red pepper flakes
- 1 tsp black pepper, coarse ground
- 1 tsp dried thyme
- ½ tsp MSG or 1 tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Blend all the ingredients in a food processor until it has an even, but still moderately coarse, texture.
2) Shape into 1″ balls, and put them in the fridge to chill for about 20 minutes.
3) Fry the balls over a medium-high heat until evenly browned—just do a few at a time, taking care to not overcrowd the pan.
4) Serve! Great with salad, hummus, and other such tasty healthy snack items:
Enjoy!
Want to learn more?
For those interested in more of what we have going on today:
- Cilantro vs Parsley – Which is Healthier?
- Our Top 5 Spices: How Much Is Enough For Benefits?
- What Matters Most For Your Heart?
- An Apple (Cider Vinegar) A Day…
- Hero Homemade Hummus Recipe ← perfect accompaniment!
- Tasty Tabbouleh with Tahini Recipe ← also a great option!
Take care!
Share This Post
-
Insomnia Decoded – by Dr. Audrey Porter
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written about sleep books before, so what makes this one different? Its major selling point is: most of the focus isn’t on the things that everyone already knows.
Yes, there’s a section on sleep hygiene and yes it’ll tell you to cut the caffeine and alcohol, but most of the advice here is beyond that.
Rather, it looks at finding out (if you don’t already know for sure) what is keeping you from healthy sleep, be it environmental, directly physical, or psychological, and breaking out of the stress-sleep cycle that often emerges from such.
The style is light and conversational, but includes plenty of science too; Dr. Porter knows her stuff.
Bottom line: if you feel like you know what you should be doing, but somehow life keeps conspiring to stop you from doing it, then this is the book that could help you break out that cycle.
Click here to check out Insomnia Decoded, and get regular healthy sleep!
Share This Post
Related Posts
-
Is Vitamin C Worth The Hype? (Doctorly Investigates)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Double Board-Certified Dermatologists Dr. Muneeb Shah & Dr. Luke Maxfield weigh in on vitamin C; is it worth the hype?
Yes it is, but…
There are some caveats, for example:
- It’s best to apply vitamin C on clean, dry skin and let it set before layering other products.
- Avoid mixing with oxidants like benzoyl peroxide (cancels out antioxidant effects).
- Avoid combining with copper (may negate brightening benefits).
- Do not use with hypochlorous acid (oxidative reactions cancel out benefits).
- Be cautious with retinol due to irritation risks.
However, used correctly, it does give very worthy benefits, and they recommend:
- Morning use: acts as an antioxidant, pairs well with sunscreen for better protection from sun and environmental damage.
- Night use: maximizes functions like improving tone, collagen production, texture, and reducing wrinkles.
That’s not to say that at night it stops being an antioxidant or during the day it isn’t critical for collagen synthesis, but it is to say: because of the different things our bodies typically encounter and/or do during the day or night, those are the best times to get the most out of those benefits.
They also review some popular products; here are some notes on their comments about them:
- Skinceuticals C E Ferulic: research-backed, $180, effective but potentially irritating.
- Skinceuticals Phloretin CF: includes 0.5% salicylic acid, good for acne-prone skin.
- Dermatology Vitamin C E Ferulic: relatively more affordable ($70), fragrance-free, includes peptides and ceramides.
- Drunk Elephant C-Firma: powder-to-serum formula, sued for patent infringement.
- Paula’s Choice C15 Booster: reformulated, fragrance-free, similar to Skinceuticals.
- Neutrogena Vitamin C Capsules: stabilized 20% ascorbic acid, single-use, travel-friendly.
- La Roche-Posay Vitamin C Serum: contains fragrance and alcohol, not ideal for sensitive skin.
- Matter of Fact Vitamin C Serum: includes ascorbic acid and ferulic acid, oily texture for dry skin.
- Medik8 Super C Ferulic: stable 30% ethyl ascorbic acid, lightweight texture.
- Naturium Vitamin C Complex: multi-form Vitamin C with niacinamide, alpha arbutin, and turmeric.
- Timeless Vitamin C Serum: affordable ($20), 20% ascorbic acid with E and ferulic acid.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
More Than Skin-Deep: Six Ways To Eat For Healthier Skin ← this one’s about a lot more than just vitamin C 😎
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Secret Easy Tips to Loosen Your Hips In 10 Minutes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Stiff hips can often cause discomfort, and ultimately back pain because of how one thing relies on the other as its seat. However, there are ways to improve it without taking years to get to where you want to be:
One bit at a time
Warm up and massage:
- Massage the front and back of the thighs to loosen tight muscles.
- Use your body weight for effective massaging.
- Relax and breathe slowly while massaging.
Vary your stretches:
- Perform a seated butterfly stretch, but avoid overexertion.
- Move knees gently within a comfortable range of motion.
- Perform stretches like placing one foot on the opposite knee or holding legs to open hips.
- Stretch the hips while lying on the floor with bent knees.
And now for the “magic move”: lie on your stomach, bend one knee, and gently rock to loosen hip stiffness.
Generally speaking, for most stretches one can usually stretch further on one side at once, than both at the same time. So, leverage this in your flexibility training, to get each side of your body accustomed to going that bit further. Then, when your body is comfortable with that, put it together.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
How Tight Are Your Hips? Test (And Fix!) With This
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
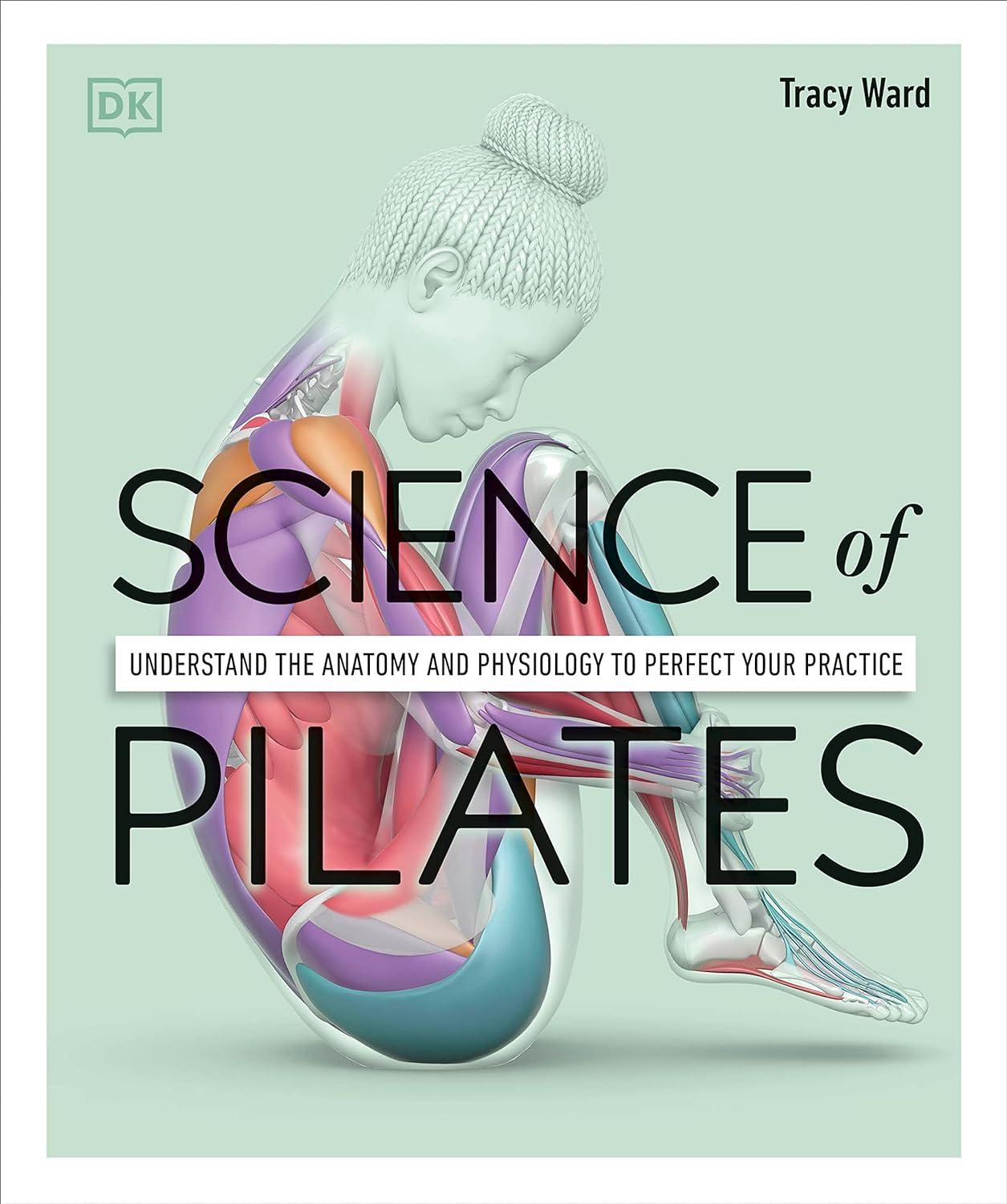
Science of Pilates – by Tracy Ward
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed other books in this series, “Science of Yoga” and “Science of HIIT” (they’re great too; check them out!). What does this one add to the mix?
Pilates is a top-tier “combination exercise” insofar as it checks a lot of boxes, e.g:
- Strength—especially core strength, but also limbs
- Mobility—range of motion and resultant reduction in injury risk
- Stability—impossible without the above two things, but Pilates trains this too
- Fitness—many dynamic Pilates exercises can be performed as cardio and/or HIIT.
The author, a physiotherapist, explains (as the title promises!) the science of Pilates, with:
- the beautifully clear diagrams we’ve come to expect of this series,
- equally clear explanations, with a great balance of simplicity of terms and depth where necessary, and
- plenty of citations for the claims made, linking to lots of the best up-to-date science.
Bottom line: if you are in a position to make a little time for Pilates (if you don’t already), then there is nobody who would not benefit from reading this book.
Click here to check out Science of Pilates, and keep your body well!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: