Diet Tips for Crohn’s Disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Doctors are great at saving lives like mine. I’m a two time survivor of colon cancer and have recently been diagnosed with Chron’s disease at 62. No one is the health system can or is prepared to tell me an appropriate diet to follow or what to avoid. Can you?❞
Congratulations on the survivorship!
As to Crohn’s, that’s indeed quite a pain, isn’t it? In some ways, a good diet for Crohn’s is the same as a good diet for most other people, with one major exception: fiber
…and unfortunately, that changes everything, in terms of a whole-foods majority plant-based diet.
What stays the same:
- You still ideally want to eat a lot of plants
- You definitely want to avoid meat and dairy in general
- Eating fish is still usually* fine, same with eggs
- Get plenty of water
What needs to change:
- Consider swapping grains for potatoes or pasta (at least: avoid grains)
- Peel vegetables that are peelable; discard the peel or use it to make stock
- Consider steaming fruit and veg for easier digestion
- Skip spicy foods (moderate spices, like ginger, turmeric, and black pepper, are usually fine in moderation)
Much of this latter list is opposite to the advice for people without Crohn’s Disease.
*A good practice, by the way, is to keep a food journal. There are apps that you can get for free, or you can do it the old-fashioned way on paper if prefer.
But the important part is: make a note not just of what you ate, but also of how you felt afterwards. That way, you can start to get a picture of patterns, and what’s working (or not) for you, and build up a more personalized set of guidelines than anyone else could give to you.
We hope the above pointers at least help you get going on the right foot, though!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

The Vagus Nerve (And How You Can Make Use Of It)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Vagus Nerve: The Brain-Gut Highway
The longest cranial nerve is the vagus nerve; it runs all the way from your brain to your colon. It’s very important, and (amongst other tasks) it largely regulates your parasympathetic nervous system, and autonomous functions like:
- Breathing
- Heart rate
- Vasodilation & vasoconstriction
- Blood pressure
- Reflex actions (e.g. coughing, sneezing, swallowing, vomiting, hiccuping)
That’s great, but how does knowing about it help us?
Because of vagal maneuvers! This means taking an action to stimulate the vagus nerve, and prompt it to calm down various bodily functions that need calming down. This can take the form of:
- Massage
- Electrostimulation
- Diaphragmatic breathing
Massage is perhaps the simplest; “vagus” means “wandering”, and the nerve is accessible in various places, including behind the ears. That’s the kind of thing that’ easier to show than tell, though, so we’ll include a video at the end.
Electrostimulation is the fanciest, and has been used to treat migraines and cluster headaches. Check out, for example:
Update on noninvasive neuromodulation for migraine treatment-Vagus nerve stimulation
Diaphragmatic breathing means breathing from the diaphragm—the big muscular tissue that sits under your lungs. You might know it as “abdominal breathing”, and refers to breathing “to the abdomen” rather than merely to the chest.
Even though your lungs are obviously in your chest not your abdomen, breathing with a focus on expanding the abdomen (rather than the chest) when breathing in, will result in much deeper breathing as the diaphragm allows the lungs to fill downwards as well as outwards.
Why this helps when it comes to the vagus nerve is simply that the vagus nerve passes by the diaphragm, such that diaphragmatic breathing will massage the vagus nerve deep inside your body.
More than just treating migraines
Vagus nerve stimulation has also been researched and found potentially helpful for managing:
- Depression, inflammation, and heart disease
- Diabetes and glycemic issues in general
- Multiple sclerosis and autoimmune disease in general
- Alzheimer’s disease and dementia in general
- Rheumatoid arthritis (we already mentioned inflammation and autoimmune diseases, but this is an interesting paper so we included it)
All this is particularly important as we get older, because vagal response reduces with age, and vagus nerve stimulation, which improves vagal tone, makes it easier not just to manage the aforementioned maladies, but also simply to relax more easily and more deeply.
See: Influence of age and gender on autonomic regulation of heart
We promised a video for the massage, so here it is:
! Share This Post

4 Critical Things Female Runners Should Know
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to keeping up performance in the face of menopause, Shona Hendricks has advice:
Don’t let menopause run you down
- Prioritize recovery! Overtraining without adequate recovery just leads to decreased performance in the long term, and remember, you may not recover as quickly as you used to. If you’re still achey from your previous run, give it another day, or at least make it a lighter run.
- Slow down in easy and long runs! This isn’t “taking the easy way out”; it will improve your overall performance, reducing muscle damage, allowing for quicker recovery and ultimately better fitness gains.
- Focus on nutrition! And that means carbs too. A lot of people fighting menopausal weight gain reduce their intake of food, but without sufficient energy availability, you will not be able to run well. In particular, carbohydrates are vital for energy. Consume them sensibly and with fiber and proteins and fats rather than alone, but do consume them.
- Incorporate strength training! Your run is not “leg day” by itself. Furthermore, do whole-body strength training, to prevent injuries and improve overall performance. A strong core is particularly important.
For more on each of these (and some bonus comments about mobility training for runners), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post

A new government inquiry will examine women’s pain and treatment. How and why is it different?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Victorian government has announced an inquiry into women’s pain. Given women are disproportionately affected by pain, such a thorough investigation is long overdue.
The inquiry, the first of its kind in Australia and the first we’re aware of internationally, is expected to take a year. It aims to improve care and services for Victorian girls and women experiencing pain in the future.
The gender pain gap
Globally, more women report chronic pain than men do. A survey of over 1,750 Victorian women found 40% are living with chronic pain.
Approximately half of chronic pain conditions have a higher prevalence in women compared to men, including low back pain and osteoarthritis. And female-specific pain conditions, such as endometriosis, are much more common than male-specific pain conditions such as chronic prostatitis/chronic pelvic pain syndrome.
These statistics are seen across the lifespan, with higher rates of chronic pain being reported in females as young as two years old. This discrepancy increases with age, with 28% of Australian women aged over 85 experiencing chronic pain compared to 18% of men.
It feels worse
Women also experience pain differently to men. There is some evidence to suggest that when diagnosed with the same condition, women are more likely to report higher pain scores than men.
Similarly, there is some evidence to suggest women are also more likely to report higher pain scores during experimental trials where the same painful pressure stimulus is applied to both women and men.
Pain is also more burdensome for women. Depression is twice as prevalent in women with chronic pain than men with chronic pain. Women are also more likely to report more health care use and be hospitalised due to their pain than men.

Women seem to feel pain more acutely and often feel ignored by doctors.
ShutterstockMedical misogyny
Women in pain are viewed and treated differently to men. Women are more likely to be told their pain is psychological and dismissed as not being real or “all in their head”.
Hollywood actor Selma Blair recently shared her experience of having her symptoms repeatedly dismissed by doctors and put down to “menstrual issues”, before being diagnosed with multiple sclerosis in 2018.
It’s an experience familiar to many women in Australia, where medical misogyny still runs deep. Our research has repeatedly shown Australian women with pelvic pain are similarly dismissed, leading to lengthy diagnostic delays and serious impacts on their quality of life.
Misogyny exists in research too
Historically, misogyny has also run deep in medical research, including pain research. Women have been viewed as smaller bodied men with different reproductive functions. As a result, most pre-clinical pain research has used male rodents as the default research subject. Some researchers say the menstrual cycle in female rodents adds additional variability and therefore uncertainty to experiments. And while variability due to the menstrual cycle may be true, it may be no greater than male-specific sources of variability (such as within-cage aggression and dominance) that can also influence research findings.
The exclusion of female subjects in pre-clinical studies has hindered our understanding of sex differences in pain and of response to treatment. Only recently have we begun to understand various genetic, neurochemical, and neuroimmune factors contribute to sex differences in pain prevalence and sensitivity. And sex differences exist in pain processing itself. For instance, in the spinal cord, male and female rodents process potentially painful stimuli through entirely different immune cells.
These differences have relevance for how pain should be treated in women, yet many of the existing pharmacological treatments for pain, including opioids, are largely or solely based upon research completed on male rodents.
When women seek care, their pain is also treated differently. Studies show women receive less pain medication after surgery compared to men. In fact, one study found while men were prescribed opioids after joint surgery, women were more likely to be prescribed antidepressants. In another study, women were more likely to receive sedatives for pain relief following surgery, while men were more likely to receive pain medication.
So, women are disproportionately affected by pain in terms of how common it is and sensitivity, but also in how their pain is viewed, treated, and even researched. Women continue to be excluded, dismissed, and receive sub-optimal care, and the recently announced inquiry aims to improve this.
What will the inquiry involve?
Consumers, health-care professionals and health-care organisations will be invited to share their experiences of treatment services for women’s pain in Victoria as part of the year-long inquiry. These experiences will be used to describe the current service delivery system available to Victorian women with pain, and to plan more appropriate services to be delivered in the future.
Inquiry submissions are now open until March 12 2024. If you are a Victorian woman living with pain, or provide care to Victorian women with pain, we encourage you to submit.
The state has an excellent track record of improving women’s health in many areas, including heart, sexual, and reproductive health, but clearly, we have a way to go with women’s pain. We wait with bated breath to see the results of this much-needed investigation, and encourage other states and territories to take note of the findings.

Jane Chalmers, Senior Lecturer in Pain Sciences, University of South Australia and Amelia Mardon, PhD Candidate, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts

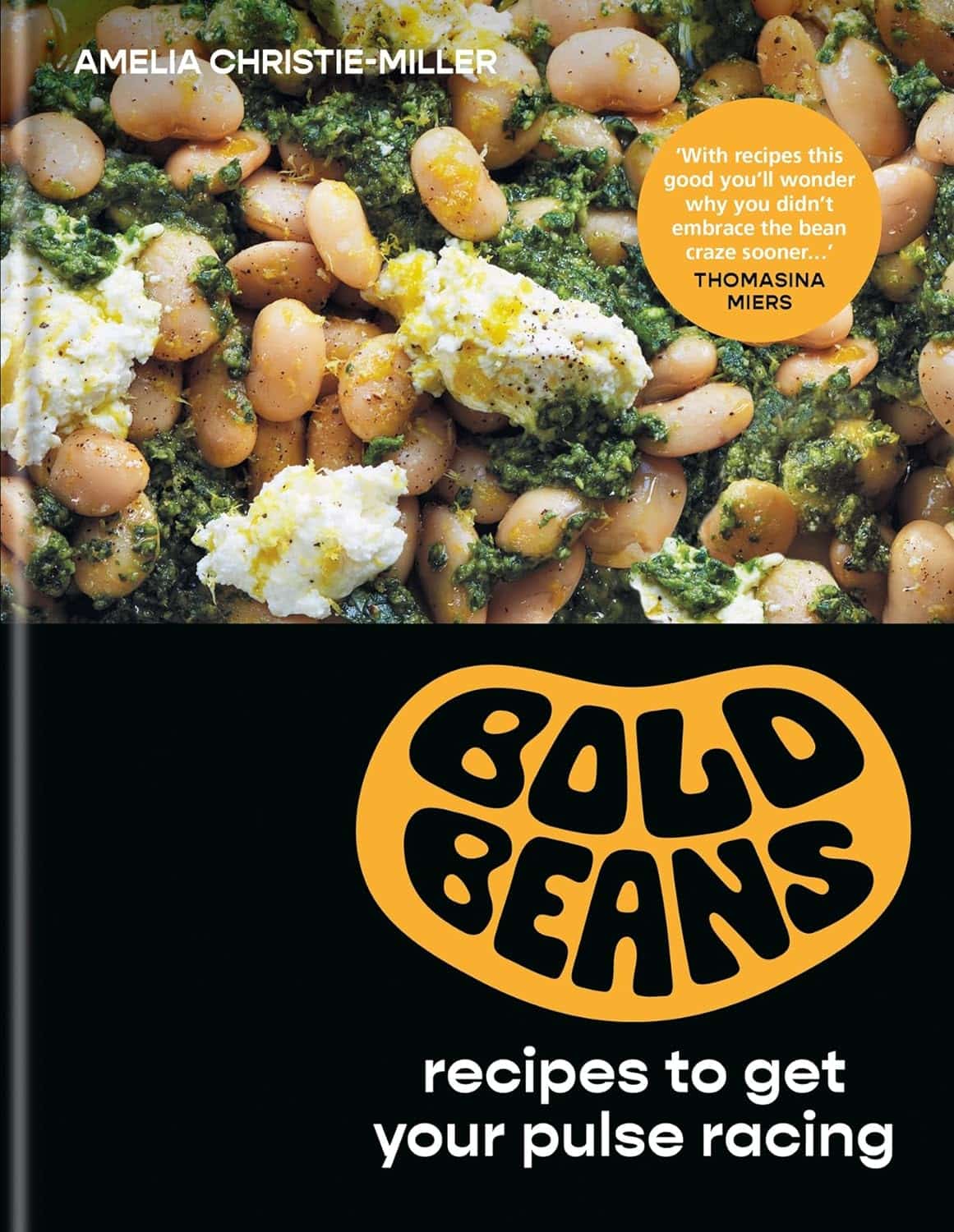
Bold Beans – by Amelia Christie-Miller
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We all know beans are one of the most healthful foods around, but how to include more of them, without getting boring?
This book has the answer, giving 80 exciting recipes, divided into the following sections:
- Speedy beans
- Bean snacks & sharing plates
- Brothy beans
- Bean bowls
- Hearty salads
- Bean feasts
The recipes are obviously all bean-centric, though if you have a particular dietary restriction, watch out for the warning labels on some (e.g. meat, fish, dairy, gluten, etc), and make a substitution if appropriate.
The recipes themselves have a happily short introductory paragraph, followed by all you’d expect from a recipe book (ingredients, measurements, method, picture)
There’s also a reference section, to learn about different kinds of beans and bean-related culinary methods that can be applied per your preferences.
Bottom line: if you’d like to include more beans in your daily diet but are stuck for making them varied and interesting, this is the book for you!
Click here to check out Bold Beans, and get your pulse racing (in a good way!)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Peas vs Broad Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing peas to broad beans, we picked the peas.
Why?
Both are great of course, but…
Looking at the macros to start with, peas have more protein and more fiber. The differences aren’t huge, but they are clear.
In terms of vitamins, peas have more of vitamins A, B1, B2, B3, B5, B6, B9, E, K, and choline (some with very large margins, some with small), while broad beans contain a little more vitamin C (the margin is quite narrow though).
When it comes to minerals, peas have more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while broad beans have more sodium. So this category wasn’t close.
Adding up the win from each of the categories makes for a clear triple-win for peas.
Easy-peasy!
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Statins and Brain Fog?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I was wondering if you had done any info about statins. I’ve tried 3, and keep quitting them because they give me brain fog. Am I imagining this as the research suggests?❞
If you are female, the chances of adverse side-effects are a lot higher:
As an extra kicker, not only are the adverse side-effects more likely for women, but also, the benefits are often less beneficial, too (see the above main feature for some details).
That’s not to say that statins can’t have their place for women; sometimes it will still be the right choice. Just, not as readily so as for men.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: