What causes the itch in mozzie bites? And why do some people get such a bad reaction?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Are you one of these people who loathes spending time outdoors at dusk as the weather warms and mosquitoes start biting?
Female mosquitoes need blood to develop their eggs. Even though they take a tiny amount of our blood, they can leave us with itchy red lumps that can last days. And sometimes something worse.
So why does our body react and itch after being bitten by a mosquito? And why are some people more affected than others?

What happens when a mosquito bites?
Mosquitoes are attracted to warm blooded animals, including us. They’re attracted to the carbon dioxide we exhale, our body temperatures and, most importantly, the smell of our skin.
The chemical cocktail of odours from bacteria and sweat on our skin sends out a signal to hungry mosquitoes.
Some people’s skin smells more appealing to mosquitoes, and they’re more likely to be bitten than others.
Once the mosquito has made its way to your skin, things get a little gross.
The mosquito pierces your skin with their “proboscis”, their feeding mouth part. But the proboscis isn’t a single, straight, needle-like tube. There are multiple tubes, some designed for sucking and some for spitting.
Once their mouth parts have been inserted into your skin, the mosquito will inject some saliva. This contains a mix of chemicals that gets the blood flowing better.
There has even been a suggestion that future medicines could be inspired by the anti-blood clotting properties of mosquito saliva.

It’s not the stabbing of our skin by the mosquito’s mouth parts that hurts, it’s the mozzie spit our bodies don’t like.
Are some people allergic to mosquito spit?
Once a mosquito has injected their saliva into our skin, a variety of reactions can follow. For the lucky few, nothing much happens at all.
For most people, and irrespective of the type of mosquito biting, there is some kind of reaction. Typically there is redness and swelling of the skin that appears within a few hours, but often more quickly, after just a few minutes.
Occasionally, the reaction can cause pain or discomfort. Then comes the itchiness.
Some people do suffer severe reactions to mosquito bites. It’s a condition often referred to as “skeeter syndrome” and is an allergic reaction caused by the protein in the mosquito’s saliva. This can cause large areas of swelling, blistering and fever.
The chemistry of mosquito spit hasn’t really been well studied. But it has been shown that, for those who do suffer allergic reactions to their bites, the reactions may differ depending on the type of mosquito biting.
We all probably get more tolerant of mosquito bites as we get older. Young children are certainly more likely to suffer more following mosquito bites. But as we get older, the reactions are less severe and may pass quickly without too much notice.
How best to treat the bites?
Research into treating bites has yet to provide a single easy solution.
There are many myths and home remedies about what works. But there is little scientific evidence supporting their use.
The best way to treat mosquito bites is by applying a cold pack to reduce swelling and to keep the skin clean to avoid any secondary infections. Antiseptic creams and lotions may also help.
There is some evidence that heat may alleviate some of the discomfort.
It’s particularly tough to keep young children from scratching at the bite and breaking the skin. This can form a nasty scab that may end up being worse than the bite itself.
Applying an anti-itch cream may help. If the reactions are severe, antihistamine medications may be required.
To save the scratching, stop the bites
Of course, it’s better not to be bitten by mosquitoes in the first place. Topical insect repellents are a safe, effective and affordable way to reduce mosquito bites.
Covering up with loose fitted long sleeved shirts, long pants and covered shoes also provides a physical barrier.
Mosquito coils and other devices can also assist, but should not be entirely relied on to stop bites.
There’s another important reason to avoid mosquito bites: millions of people around the world suffer from mosquito-borne diseases. More than half a million people die from malaria each year.
In Australia, Ross River virus infects more than 5,000 people every year. And in recent years, there have been cases of serious illnesses caused by Japanese encephalitis and Murray Valley encephalitis viruses.
Cameron Webb, Clinical Associate Professor and Principal Hospital Scientist, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
5 Steps To Beat Overwhelm
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dealing With Overwhelm
Whether we live a hectic life in general, or we usually casually take each day as it comes but sometimes several days gang up on us at once, everyone gets overwhelmed sometimes.
Today we’re going to look at how to deal with it healthily.
Step 1: Start anywhere
It’s easy to get stuck in “analysis paralysis” and not know how to tackle an unexpected large problem. An (unhealthy) alternative is to try to tackle everything at once, and end up doing nothing very well.
Even the most expert juggler will not successfully juggle 10 random things thrown unexpectedly at them.
So instead, just pick any part of the the mountain of to-dos, and start.
If you do want a little more finesse though, check out:
Procrastination, And How To Pay Off The To-Do List Debt
Step 2: Accept what you’re capable of
This one works both ways. It means being aware of your limitations yes, but also, of your actual abilities:
- Is the task ahead of you really beyond what you are capable of?
- Could you do it right now without hesitation if a loved one’s life depended on it?
- Could you do it, but there’s a price to pay (e.g. you can do it but it’ll wipe you out in some other life area)?
Work out what’s possible and acceptable to you, and make a decision. And remember, it could be that someone else could do it, but everyone has taken the “if you want something doing, give it to someone busy” approach. It’s flattering that people have such confidence in our competence, but it is also necessary to say “no” sometimes, or at least enlisting help.
Step 3: Listen to your body
…like a leader listening to an advisory council. Your perception of tiredness, pain, weakness, and all your emotions are simply messengers. Listen to the message! And then say “thank you for the information”, and proceed accordingly.
Sometimes that will be in the way the messengers seem to be hoping for!
Sometimes, however, maybe we (blessed with a weighty brain and not entirely a slave to our limbic system) know better, and know when it’s right to push through instead.
Similarly, that voice in your head? You get to decide where it goes and doesn’t. On which note…
Step 4: Be responsive, not reactive
We wrote previously on the difference between these:
A Bone To Pick… Up And Then Put Back Where We Found It
Measured responses will always be better than knee-jerk reactions, unless it is literally a case of a split-second making a difference. 99% of our problems in life are not so; usually the problem will still be there unchanged after a moment’s mindful consideration, so invest in that moment.
You’ve probably heard the saying “give me six hours to chop down a tree, and I’ll spend the first four sharpening the axe”. In this case, that can be your mind. Here’s a good starting point:
No-Frills, Evidence-Based Mindfulness
And if your mental state is already worse than that, mind racing with threats (real or perceived) and doom-laden scenarios, here’s how to get out of that negative spiral first, so that you can apply the rest of this:
Do remember to turn it on again afterwards, though
Step 5: Transcend discomfort
This is partly a callback to step 3, but it’s now coming from a place of a clear ready mind, so the territory should be looking quite different now. Nevertheless, it’s entirely possible that your clear view shows discomfort ahead.
You’re going to make a conscious decision whether or not to proceed through the discomfort (and if you’re not, then now’s the time to start calmly and measuredly looking at alternative plans; delegating, ditching, etc).
If you are going to proceed through discomfort, then it can help to frame the discomfort as simply a neutral part of the path to getting where you want. Maybe you’re going to be going way out of your comfort zone in order to deal with something, and if that’s the case, make your peace with it now, in advance.
“Certainly it hurts” / “Well, what’s the trick then?” / “The trick, William Potter, is not minding that it hurts”
(lines from a famous scene from the 1962 movie Lawrence of Arabia)
It’s ok to say to yourself (if it’s what you decide is the right thing to do) “Yep, this experience is going to suck terribly, but I’m going to do it anyway”.
See also (this being about Radical Acceptance):
What’s The Worst That Could Happen?
Take care!
Share This Post
-
Mocktails – by Moira Clark
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about quitting alcohol before (such as this one), but today’s is not about quitting, so much as about enjoying non-alcoholic drinks; it’s simply a recipe book of zero-alcohol cocktails, or “mocktails”.
What sets this book apart from many of its kind is that every recipe uses only natural and fresh ingredients, rather than finding in the ingredients list some pre-made store-bought component. Instead, because of its “everything from scratch” approach, this means:
- Everything is reliably as healthy as the ingredients you use
- Every recipe’s ingredients can be found easily unless you live in a food desert
Each well-photographed and well-written recipe also comes with a QR code to see a step-by-step video tutorial (or if you get the ebook version, then a direct link as well).
Bottom line: this is the perfect mocktail book to have in (and practice with!) before the summer heat sets in.
Click here to check out Mocktails: A Delicious Collection of Non-Alcoholic Drinks, and get mixing!
Share This Post
-
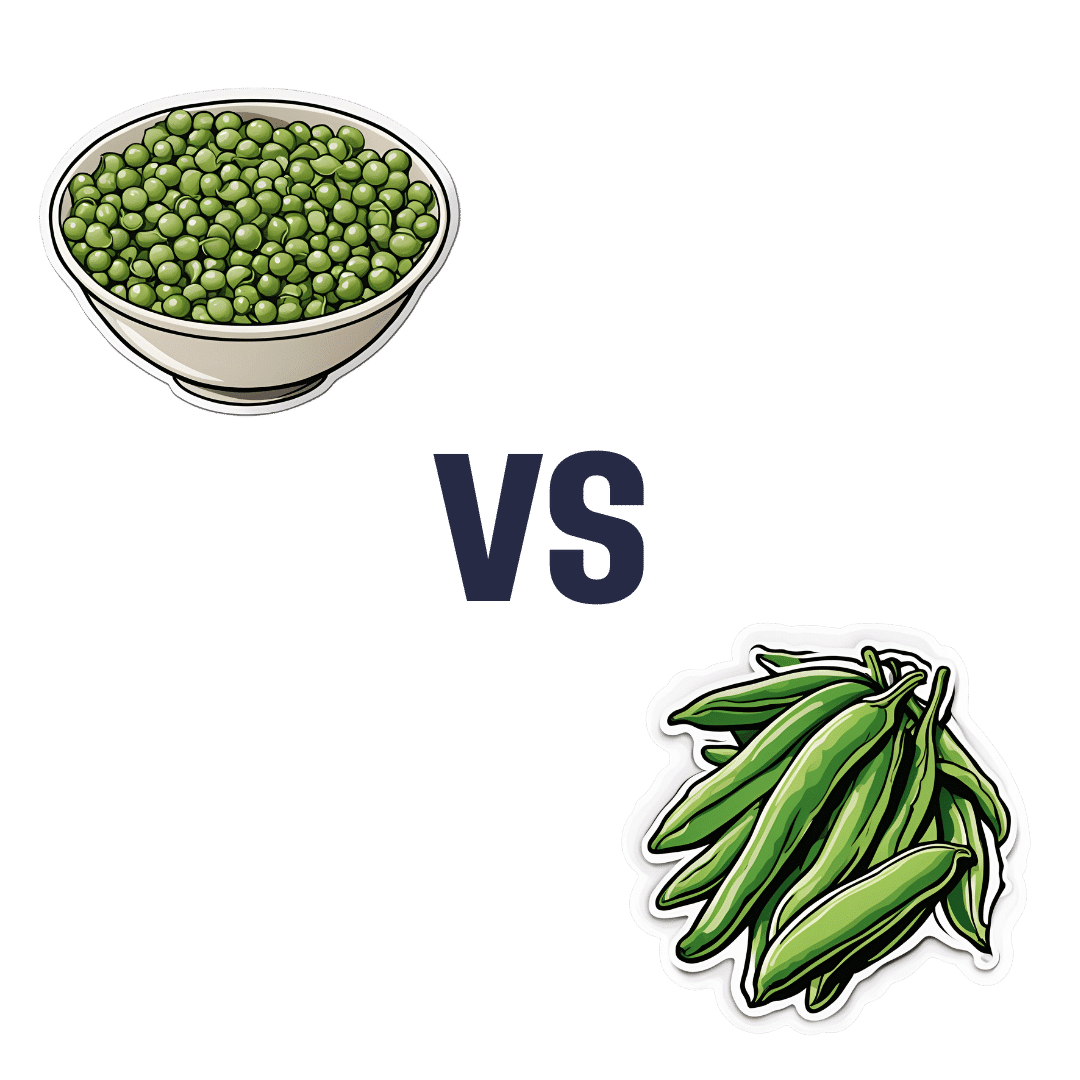
Peas vs Green Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing peas to green beans, we picked the peas.
Why?
Looking at macros first, peas have nearly 6x the protein, nearly 2x the fiber, and nearly 2x the carbs, making them the “more food per food” choice.
In terms of vitamins, peas have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, and choline, while green beans have more of vitamins E and K. An easy win for peas.
In the category of minerals, peas have more copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while green beans have more calcium. Another overwhelming win for peas.
In short, enjoy both (diversity is good), but there’s a clear winner here and it’s peas.
Want to learn more?
You might like to read:
Peas vs Broad Beans – Which is Healthier?
Take care!
Share This Post
Related Posts
-
Amid Wildfire Trauma, L.A. County Dispatches Mental Health Workers to Evacuees
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
PASADENA, Calif. — As Fernando Ramirez drove to work the day after the Eaton Fire erupted, smoke darkened the sky, ash and embers rained onto his windshield, and the air smelled of melting rubber and plastic.
He pulled to the side of the road and cried at the sight of residents trying to save their homes.
“I could see people standing on the roof, watering it, trying to protect it from the fire, and they just looked so hopeless,” said Ramirez, a community outreach worker with the Pasadena Public Health Department.
That evening, the 49-year-old volunteered for a 14-hour shift at the city’s evacuation center, as did colleagues who had also been activated for emergency medical duty. Running on adrenaline and little sleep after finding shelter for homeless people all day, Ramirez spent the night circulating among more than a thousand evacuees, offering wellness checks, companionship, and hope to those who looked distressed.
Local health departments, such as Ramirez’s, have become a key part of governments’ response to wildfires, floods, and other extreme weather events, which scientists say are becoming more intense and frequent due to climate change. The emotional toll of fleeing and possibly losing a home can help cause or exacerbate mental health conditions such as anxiety, depression, post-traumatic stress disorder, suicidal ideation, and substance use, according to health and climate experts.
Wildfires have become a recurring experience for many Angelenos, making it difficult for people to feel safe in their home or able to go about daily living, said Lisa Wong, director of the Los Angeles County Department of Mental Health. However, with each extreme weather event, the county has improved its support for evacuees, she said.
For instance, Wong said the county deployed a team of mental health workers trained to comfort evacuees without retraumatizing them, including by avoiding asking questions likely to bring up painful memories. The department has also learned to better track people’s health needs and redirect those who may find massive evacuation settings uncomfortable to other shelters or interim housing, Wong said. In those first days, the biggest goal is often to reduce people’s anxiety by providing them with information.
“We’ve learned that right when a crisis happens, people don’t necessarily want to talk about mental health,” said Wong, who staffed the evacuation site Jan. 8 with nine colleagues.
Instead, she and her team deliver a message of support: “This is really bad right now, but you’re not going to do this alone. We have a whole system set up for recovery too. Once you get past the initial shock of what happened — initial housing needs, medication needs, all those things — then there’s this whole pathway to recovery that we set up.”
The convention center in downtown Pasadena, which normally hosts home shows, comic cons, and trade shows, was transformed into an evacuation site with hundreds of cots. It was one of at least 13 shelters opened to serve more than 200,000 residents under evacuation orders.
The January wildfires have burned an estimated 64 square miles — an area larger than the city of Paris — and destroyed at least 12,300 buildings since they started Jan. 7. AccuWeather estimates the region will likely face more than $250 billion in economic losses from the blazes, surpassing the estimates from the state’s record-breaking 2020 wildfire season.
Lisa Patel, executive director of the Medical Society Consortium on Climate and Health, said she’s most concerned about low-income residents, who are less likely to access mental health support.
“There was a mental health crisis even before the pandemic,” said Patel, who is also a clinical associate professor of pediatrics at Stanford School of Medicine, referring to the covid-19 pandemic. “The pandemic made it worse. Now you lace in all of this climate change and these disasters into a health care system that isn’t set up to care for the people that already have mental health illness.”
Early research suggests exposure to large amounts of wildfire smoke can damage the brain and increase the risk of developing anxiety, she added.
At the Pasadena Convention Center, Elaine Santiago sat on a cot in a hallway as volunteers pulled wagons loaded with soup, sandwiches, bottled water, and other necessities.
Santiago said she drew comfort from being at the Pasadena evacuation center, knowing that she wasn’t alone in the tragedy.
“It sort of gives me a sense of peace at times,” Santiago said. “Maybe that’s weird. We’re all experiencing this together.”
She had been celebrating her 78th birthday with family when she fled her home in the small city of Sierra Madre, east of Pasadena. As she watched flames whip around her neighborhood, she, along with children and grandkids, scrambled to secure their dogs in crates and grabbed important documents before they left.
The widower had leaned on her husband in past emergencies, and now she felt lost.
“I did feel helpless,” Santiago said. “I figured I’m the head of the household; I should know what to do. But I didn’t know.”
Donny McCullough, who sat on a neighboring green cot draped in a Red Cross blanket, had fled his Pasadena home with his family early on the morning of Jan. 8. Without power at home, the 68-year-old stayed up listening for updates on a battery-powered radio. His eyes remained red from smoke irritation hours later.
“I had my wife and two daughters, and I was trying not to show fear, so I quietly, inside, was like, ‘Oh my God,’” said McCullough, a music producer and writer. “I’m driving away, looking at the house, wondering if it’s going to be the last time I’m going to see it.”
He saved his master recording from a seven-year music project, but he left behind his studio with all his other work from a four-decade career in music.
Not all evacuees arrived with family. Some came searching for loved ones. That’s one of the hardest parts of his shift, Ramirez said. The community outreach worker helped walk people around the building, cot by cot.
A week in, at least two dozen people had been killed in the wildfires.
The work takes a toll on disaster relief workers too. Ramirez said many feared losing their homes in the fires and some already had. He attends therapy weekly, which he said helps him manage his emotions.
At the evacuation center, Ramirez described being on autopilot.
“Some of us react differently. I tend to go into fight mode,” Ramirez said. “I react. I run towards the fire. I run towards personal service. Then once that passes, that’s when my trauma catches up with me.”
Need help? Los Angeles County residents in need of support can call the county’s mental health helpline at 1-800-854-7771. The national Suicide & Crisis Lifeline, 988, is also available for those who’d like to speak with someone confidentially, free of charge.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
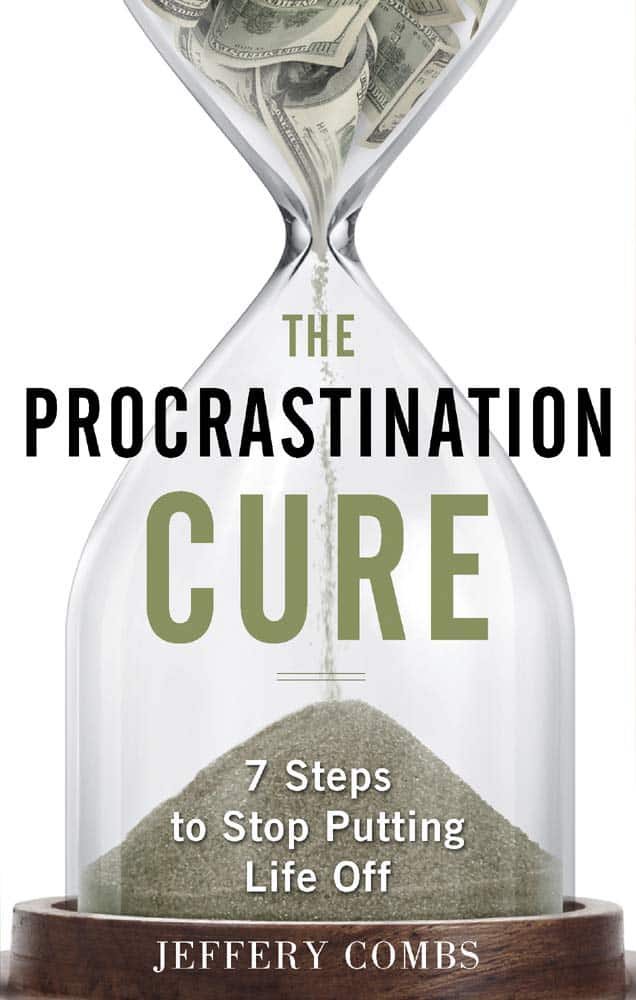
The Procrastination Cure – by Jeffery Combs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Why do we procrastinate? It’s not usually because we are lazy, and in fact we can often make ourselves very busy while procrastinating. And at some point, the bad feelings about procrastinating become worse than the experience of actually doing the thing. And still we often procrastinate. So, why?
Jeffery Combs notes that the reasons can vary, but generally fall into six mostly-distinct categories. He calls them:
- The neurotic perfectionist
- The big deal chaser
- The chronic worrier
- The rebellious rebel
- The drama addict
- The angry giver
These may overlap somewhat, but the differences are important when it comes to differences of tackling them.
Giving many illustrative examples, Combs gives the reader all we’ll need to know which category (or categories!) we fall into.
Then, he draws heavily on the work of Dr. Albert Ellis to find ways to change the feelings that we have that are holding us back.
Those feelings might be fear, shame, resentment, overwhelm, or something else entirely, but the tools are in this book.
A particular strength of this book is that it takes an approach that’s essentially Rational Emotive Behavior Therapy (REBT) repackaged for a less clinically-inclined audience (Combs’ own background is in marketing, not pyschology). Thus, for many readers, this will tend to make the ideas more relatable, and the implementations more accessible.
Bottom line: if you’ve been meaning to figure out how to beat your procrastination, but have been putting it off, now’s the time to do it.
Click here to check out The Procrastination Cure sooner rather than later!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eat All You Want (But Wisely)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Some Surprising Truths About Hunger And Satiety
This is Dr. Barbara Rolls. She’s Professor and Guthrie Chair in Nutritional Sciences, and Director of the Laboratory for the Study of Human Ingestive Behavior at Pennsylvania State University, after graduating herself from Oxford and Cambridge (yes, both). Her “awards and honors” take up four A4 pages, so we won’t list them all here.
Most importantly, she’s an expert on hunger, satiety, and eating behavior in general.
What does she want us to know?
First and foremost: you cannot starve yourself thin, unless you literally starve yourself to death.
What this is about: any weight lost due to malnutrition (“not eating enough” is malnutrition) will always go back on once food becomes available. So unless you die first (not a great health plan), merely restricting good will always result in “yo-yo dieting”.
So, to avoid putting the weight back on and feeling miserable every day along the way… You need to eat as much as you feel you need.
But, there’s a trick here (it’s about making you genuinely feel you need less)!
Your body is an instrument—so play it
Your body is the tool you use to accomplish pretty much anything you do. It is, in large part, at your command. Then there are other parts you can’t control directly.
Dr. Rolls advises taking advantage of the fact that much of your body is a mindless machine that will simply follow instructions given.
That includes instructions like “feel hungry” or “feel full”. But how to choose those?
Volume matters
An important part of our satiety signalling is based on a physical sensation of fullness. This, by the way, is why bariatric surgery (making a stomach a small fraction of the size it was before) works. It’s not that people can’t eat more (the stomach is stretchy and can also be filled repeatedly), it’s that they don’t want to eat more because the pressure sensors around the stomach feel full, and signal the hormone leptin to tell the brain we’re full now.
Now consider:
- On the one hand, 20 grapes, fresh and bursting with flavor
- On the other hand, 20 raisins (so, dried grapes), containing the same calories
Which do you think will get the leptin flowing sooner? Of course, the fresh grapes, because of the volume.
So if you’ve ever seen those photos that show two foods side by side with the same number of calories but one is much larger (say, a small slice of pizza or a big salad), it’s not quite the cheap trick that it might have appeared.
Or rather… It is a cheap trick; it’s just a cheap trick that works because your stomach is quite a simple organ.
So, Dr. Rolls’ advice: generally speaking, go for voluminous food. Fruit is great from this, because there’s so much water. Air-popped popcorn also works great. Vegetables, too.
Water matters, but differently than you might think
A well-known trick is to drink water before and with a meal. That’s good, it’s good to be hydrated. However, it can be better. Dr. Rolls did an experiment:
The design:
❝Subjects received 1 of 3 isoenergetic (1128 kJ) preloads 17 min before lunch on 3 d and no preload on 1 d.
The preloads consisted of 1) chicken rice casserole, 2) chicken rice casserole served with a glass of water (356 g), and 3) chicken rice soup.
The soup contained the same ingredients (type and amount) as the casserole that was served with water.❞
The results:
❝Decreasing the energy density of and increasing the volume of the preload by adding water to it significantly increased fullness and reduced hunger and subsequent energy intake at lunch.
The equivalent amount of water served as a beverage with a food did not affect satiety.❞
The conclusion:
❝Consuming foods with a high water content more effectively reduced subsequent energy intake than did drinking water with food.❞
You can read the study in full (it’s a worthwhile read!) here:
Water incorporated into a food but not served with a food decreases energy intake in lean women
Protein matters
With all those fruits and vegetables and water, you may be wondering Dr. Rolls’ stance on proteins. It’s simple: protein is an appetite suppressant.
However, it takes about 20 minutes to signal the brain about that, so having some protein in a starter (if like this writer, you’re the cook of the household, a great option is to enjoy a small portion of nuts while cooking!) gets that clock ticking, to signal satiety sooner.
It may also help in other ways:
Clinical Evidence and Mechanisms of High-Protein Diet-Induced Weight Loss
As for other foods that can suppress appetite, by the way, you might like;
25 Foods That Act As Natural Appetite Suppressants
Variety matters, and in ways other than you might think
A wide variety of foods (especially: a wide variety of plants) in one’s diet is well recognized as a key to a good balanced diet.
However…
A wide variety of dishes at the table, meanwhile, promotes greater consumption of food.
Dr. Rolls did a study on this too, a while ago now (you’ll see how old it is) but the science seems robust:
Variety in a Meal Enhances Food Intake in Man
Notwithstanding the title, it wasnot about a man (that was just how scientists wrote in ye ancient times of 1981). The test subjects were, in order: rats, cats, a mixed group of men and women, the same group again, and then a different group of all women.
So, Dr. Rolls’ advice is: it’s better to have one 20-ingredient dish, than 10 dishes with 20 ingredients between them.
Sorry! We love tapas and buffets too, but that’s the science!
So, “one-pot” meals are king in this regard; even if you serve it with one side (reasonable), that’s still only two dishes, which is pretty good going.
Note that the most delicious many-ingredient stir-fries and similar dishes from around the world also fall into this category!
Want to know more?
If you have the time (it’s an hour), you can enjoy a class of hers for free:
Want to watch it, but not right now? Bookmark it for later
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: