Vaccines and cancer: The myth that won’t die
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Two recent studies reported rising cancer rates among younger adults in the U.S. and worldwide. This prompted some online anti-vaccine accounts to link the studies’ findings to COVID-19 vaccines.
But, as with other myths, the data tells a very different story.
What you need to know
- Baseless claims that COVID-19 vaccines cause cancer have persisted online for several years and gained traction in late 2023.
- Two recent reports finding rising cancer rates among younger adults are based on pre-pandemic cancer incidence data. Cancer rates in the U.S. have been on the rise since the 1990s.
- There is no evidence of a link between COVID-19 vaccination and increased cancer risk.
False claims about COVID-19 vaccines began circulating months before the vaccines were available. Chief among these claims was misinformed speculation that vaccine mRNA could alter or integrate into vaccine recipients’ DNA.
It does not. But that didn’t prevent some on social media from spinning that claim into a persistent myth alleging that mRNA vaccines can cause or accelerate cancer growth. Anti-vaccine groups even coined the term “turbo cancer” to describe a fake phenomenon of abnormally aggressive cancers allegedly linked to COVID-19 vaccines.
They used the American Cancer Society’s 2024 cancer projection—based on incidence data through 2020—and a study of global cancer trends between 1999 and 2019 to bolster the false claims. This exposed the dishonesty at the heart of the anti-vaccine messaging, as data that predated the pandemic by decades was carelessly linked to COVID-19 vaccines in viral social media posts.
Some on social media cherry-pick data and use unfounded evidence because the claims that COVID-19 vaccines cause cancer are not true. According to the National Cancer Institute and American Cancer Society, there is no evidence of any link between COVID-19 vaccines and an increase in cancer diagnosis, progression, or remission.
Why does the vaccine cancer myth endure?
At the root of false cancer claims about COVID-19 vaccines is a long history of anti-vaccine figures falsely linking vaccines to cancer. Polio and HPV vaccines have both been the target of disproven cancer myths.
Not only do HPV vaccines not cause cancer, they are one of only two vaccines that prevent cancer.
In the case of polio vaccines, some early batches were contaminated with simian virus 40 (SV40), a virus that is known to cause cancer in some mammals but not humans. The contaminated batches were discovered, and no other vaccine has had SV40 contamination in over 60 years.
Follow-up studies found no increase in cancer rates in people who received the SV40-contaminated polio vaccine. Yet, vaccine opponents have for decades claimed that polio vaccines cause cancer.
Recycling of the SV40 myth
The SV40 myth resurfaced in 2023 when vaccine opponents claimed that COVID-19 vaccines contain the virus. In reality, a small, nonfunctional piece of the SV40 virus is used in the production of some COVID-19 vaccines. This DNA fragment, called the promoter, is commonly used in biomedical research and vaccine development and doesn’t remain in the finished product.
Crucially, the SV40 promoter used to produce COVID-19 vaccines doesn’t contain the part of the virus that enters the cell nucleus and is associated with cancer-causing properties in some animals. The promoter also lacks the ability to survive on its own inside the cell or interact with DNA. In other words, it poses no risk to humans.
Over 5.6 billion people worldwide have received COVID-19 vaccines since December 2020. At that scale, even the tiniest increase in cancer rates in vaccinated populations would equal hundreds of thousands of excess cancer diagnoses and deaths. The evidence for alleged vaccine-linked cancer would be observed in real incidence, treatment, and mortality data, not social media anecdotes or unverifiable reports.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A Correction, And A New, Natural Way To Boost Daily Energy Levels
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
First: a correction and expansion!
After yesterday’s issue of 10almonds covering breast cancer risks and checks, a subscriber wrote to say, with regard to our opening statement, which was:
“Anyone (who has not had a double mastectomy, anyway) can get breast cancer”
❝I have been enjoying your newsletter. This statement is misleading and should have a disclaimer that says even someone who has had a double mastectomy can get breast cancer, again. It is true and nothing…nothing is 100% including a mastectomy. I am a 12 year “thriver” (I don’t like to use the term survivor) who has had a double mastectomy. I work with a local hospital to help newly diagnosed patients deal with their cancer diagnosis and the many decisions that follow. A double mastectomy can help keep recurrence from happening but there are no guarantees. I tried to just delete this and let it go but it doesn’t feel right. Thank you!❞
Thank you for writing in about this! We wouldn’t want to mislead, and we’re always glad to hear from people who have been living with conditions for a long time, as (assuming they are a person inclined to learning) they will generally know topics far more deeply than someone who has researched it for a short period of time.
Regards a double mastectomy (we’re sure you know this already, but noting here for greater awareness, prompted by your message), a lot of circumstances can vary. For example, how far did a given cancer spread, and especially, did it spread to the lymph nodes at the armpits? And what tissue was (and wasn’t) removed?
Sometimes a bilateral prophylactic mastectomy will leave the lymph nodes partially or entirely intact, and a cancer could indeed come back, if not every last cancerous cell was removed.
A total double mastectomy, by definition, should have removed all tissue that could qualify as breast tissue for a breast cancer, including those lymph nodes. However, if the cancer spread unnoticed somewhere else in the body, then again, you’re quite correct, it could come back.
Some people have a double mastectomy without having got cancer first. Either because of a fear of cancer due to a genetic risk (like Angelina Jolie), or for other reasons (like Elliot Page).
This makes a difference, because doing it for reasons of cancer risk may mean surgeons remove the lymph nodes too, while if that wasn’t a factor, surgeons will tend to leave them in place.
In principle, if there is no breast tissue, including lymph nodes, and there was no cancer to spread, then it can be argued that the risk of breast cancer should now be the same “zero” as the risk of getting prostate cancer when one does not have a prostate.
But… Surgeries are not perfect, and everyone’s anatomy and physiology can differ enough from “textbook standard” that surprises can happen, and there’s almost always a non-zero chance of certain health outcomes.
For any unfamiliar, here’s a good starting point for learning about the many types of mastectomy, that we didn’t go into in yesterday’s edition. It’s from the UK’s National Health Service:
NHS: Mastectomy | Types of Mastectomy
And for the more sciency-inclined, here’s a paper about the recurrence rate of cancer after a prophylactic double mastectomy, after a young cancer was found in one breast.
The short version is that the measured incidence rate of breast cancer after prophylactic bilateral mastectomy was zero, but the discussion (including notes about the limitations of the study) is well worth reading:
Breast Cancer after Prophylactic Bilateral Mastectomy in Women with a BRCA1 or BRCA2 Mutation
❝[Can you write about] the availability of geriatric doctors Sometimes I feel my primary isn’t really up on my 70 year old health issues. I would love to find a doctor that understands my issues and is able to explain them to me. Ie; my worsening arthritis in regards to food I eat; in regards to meds vs homeopathic solutions.! Thanks!❞
That’s a great topic, worthy of a main feature! Because in many cases, it’s not just about specialization of skills, but also about empathy, and the gap between studying a condition and living with a condition.
About arthritis, we’re going to do a main feature specifically on that quite soon, but meanwhile, you might like our previous article:
Keep Inflammation At Bay (arthritis being an inflammatory condition)
As for homeopathy, your question prompts our poll today!
(and then we’ll write about that tomorrow)
Share This Post
-
Ginkgo Biloba, For Memory And, Uh, What Else Again?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ginkgo biloba, for memory and, uh, what else again?
Ginkgo biloba extract has enjoyed use for thousands of years for an assortment of uses, and has made its way from Traditional Chinese Medicine, to the world supplement market at large. See:
Ginkgo biloba: A Treasure of Functional Phytochemicals with Multimedicinal Applications
But what does the science say about the specific claims?
Antioxidant & anti-inflammatory
We’re going to lump these two qualities together for examination, since one invariably leads to the other.
A quick note: things that have antioxidant and anti-inflammatory properties, often also help guard against cancer and aging. However, in this case, there are few good studies pertaining to anti-aging, and none that we could find pertaining to anti-cancer potential.
So, does it have antioxidant and anti-inflammatory properties, first?
Yes, it has potent antioxidants that do fight inflammation; this is clear, from an abundance of in vitro and in vivo studies, including with human patients:
- Properties of Ginkgo biloba L.: incl. Antioxidant Characterization
- Anti-inflammatory effects of Ginkgo biloba extract against hippocampal neuronal injury
- Gingko biloba-derived lactone prevents osteoarthritis by activating anti-inflammatory signaling pathway
- The anti-inflammatory properties of Ginkgo biloba for the treatment of pulmonary diseases
In short: it helps, and there’s plenty of science for it.
What about anti-aging effects?
For this, there is science, but a lot of the science is not great. As one team of researchers concluded while doing a research review of their own:
❝Based on the reviewed information regarding EGb’s effects in vitro and in vivo, most have reported very positive outcomes with strong statistical analyses, indicating that EGb must have some sort of beneficial effect.
However, information from the reported clinical trials involving EGb are hardly conclusive since many do not include information such as the participant’s age and physical condition, drug doses administered, duration of drug administered as well as suitable control groups for comparison.
We therefore call on clinicians and clinician-scientists to establish a set of standard and reliable standard operating procedure for future clinical studies to properly evaluate EGb’s effects in the healthy and diseased person since it is highly possible it possesses beneficial effects.❞
Translation from sciencese: “These results are great, but come on, please, we are begging you to use more robust methodology”
If you’d like to read the review in question, here it is:
Advances in the Studies of Ginkgo Biloba Leaves Extract on Aging-Related Diseases
Does it have cognitive enhancement effects?
The claims here are generally that it helps:
- improve memory
- improve focus
- reduce cognitive decline
- reduce anxiety and depression
Let’s break these down:
Does it improve memory and cognition?
Ginkgo biloba was quite popular for memory 20+ years ago, and perhaps had an uptick in popularity in the wake of the 1999 movie “Analyze This” in which the protagonist psychiatrist mentions taking ginkgo biloba, because “it helps my memory, and I forget what else”.
Here are a couple of studies from not long after that:
- A double-blind, placebo-controlled, randomized trial of Ginkgo biloba in cognitively intact older adults: neuropsychological findings
- Effects of Ginkgo biloba on mental functioning in healthy volunteers
In short:
- in the first study, it helped in standardized tests of memory and cognition (quite convincing)
- In the second study, it helped in subjective self-reports of mental wellness (also placebo-controlled)
On the other hand, here’s a more recent research review ten years later, that provides measures of memory, executive function and attention in 1132, 534 and 910 participants, respectively. That’s quite a few times more than the individual studies we cited above, by the way. They concluded:
❝We report that G. biloba had no ascertainable positive effects on a range of targeted cognitive functions in healthy individuals❞
Read: Is Ginkgo biloba a cognitive enhancer in healthy individuals? A meta-analysis
Our (10almonds) conclusion: we can’t say either way, on this one.
Does it have neuroprotective effects (i.e., against cognitive decline)?
Yes—probably by the same mechanism will discuss shortly.
- Ginkgo Biloba for Mild Cognitive Impairment and Alzheimer’s Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
- Treatment effects of Ginkgo biloba extract on symptoms of dementia: meta-analysis of randomized controlled trials
Can it help against depression and anxiety?
Yes—but probably indirectly by the mechanism we’ll get to in a moment:
- Role of Ginkgo biloba extract as an adjunctive treatment of elderly patients with depression
- Ginkgo biloba in generalized anxiety disorder and adjustment disorder with anxious mood
Likely this helps by improving blood flow, as illustrated better per:
Efficacy of ginkgo biloba extract as augmentation of venlafaxine in treating post-stroke depression
Which means…
Bonus: improved blood flow
This mechanism may support the other beneficial effects.
See: Ginkgo biloba extract improves coronary blood flow in healthy elderly adults
Is it safe?
Ginkgo biloba extract* is generally recognized as safe.
- However, as it improves blood flow, please don’t take it if you have a bleeding disorder.
- Additionally, it may interact badly with SSRIs, so you might want to avoid it if you’re taking such (despite it having been tested and found beneficial as an adjuvant to citalopram, an SSRI, in one of the studies above).
- No list of possible contraindications can be exhaustive, so please consult your own doctor/pharmacist before taking something new.
*Extract, specifically. The seeds and leaves of this plant are poisonous. Sometimes “all natural” is not better.
Where can I get it?
As ever, we don’t sell it (or anything else), but here’s an example product on Amazon
Enjoy!
Share This Post
Share This Post
-
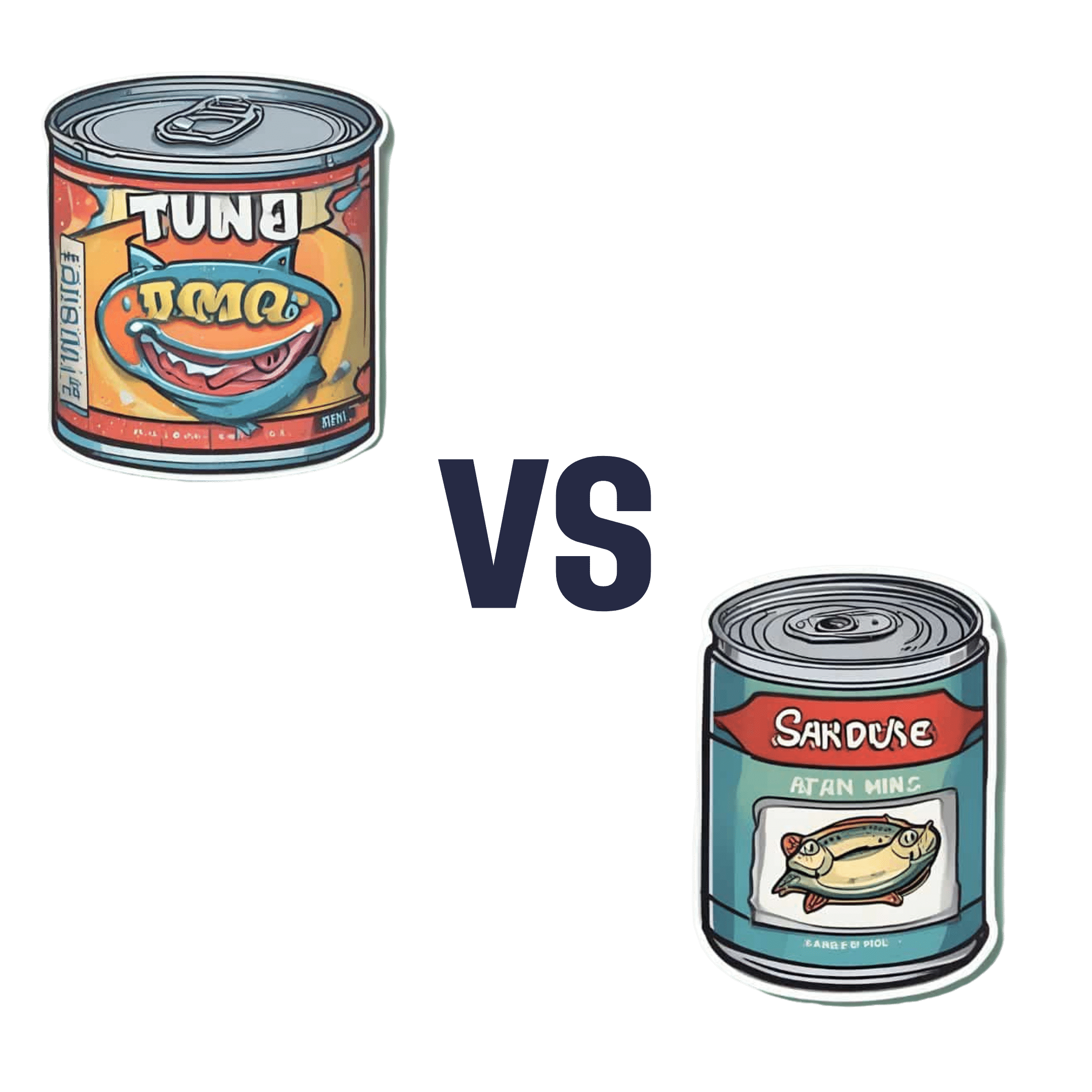
Canned Tuna vs Canned Sardines – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing canned tuna to canned sardines, we picked the sardines.
Why?
This comparison is unfair, but practical—because both are sold next to each other in the supermarket and often used for similar things.
It’s unfair because in a can of tuna, there is tuna meat, whereas in a can of sardines, there is sardine meat, skin, and bones.
Consequently, sardines outperform tuna in almost everything, because a lot of nutrients are in the skin and bones.
To be completely unambiguous:
Sardines have more vitamins and minerals by far (special shout-out to calcium, of which sardines contain 6000% more), and more choline (which is sometimes reckoned as a vitamin, sometimes not).
Tuna does have marginally more protein, and less fat. If you are trying to limit your cholesterol intake, then that could be an argument for choosing tuna over sardines.
All in all: the sardines are more nutrient dense by far, are good sources of vitamins and minerals that tuna contains less of (and in many cases only trace amounts of), and for most people this will more than offset the difference in cholesterol, especially if having not more than one can per day.
About that skin and bones…
That’s where the real benefit for your joints lies, by the way!
See: We Are Such Stuff As Fish Are Made Of
Enjoy!
Share This Post
Related Posts
-
How Not To Get Sick: A Cookbook – by Dr. Benjamin Bikman and Diana Keuilian
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Bikman’s excellent “Why We Get Sick”, and if you haven’t read that yet, we recommend doing so.
Nevertheless, you don’t need to have read it to benefit from this one, which is about cooking with those learnings (from the other book) in mind.
Before getting to the recipes, we get a section recapping what we learned previously, as well as adding some more general lifestyle advices beyond the kitchen. The science is also expanded a bit, to include such things as the two-way relationship between insulin and aging, as well as the interplay with other metrics of health, including blood lipids, for example.
The authors then provide a plan, in the three stages: reverse (insulin resistance), prevent (insulin resistance), maintain (insulin sensitivity).
The recipes themselves, of which there are 70, are of course tailored to do the above three things; they’re also quite diverse, albeit if you are vegetarian or vegan, you should know in advance that most of these recipes are not.
Bottom line: if the above doesn’t apply to you, and you would like to improve your insulin sensitivity, this book can indeed help.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tribulus Terrestris For Testosterone?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
(Clinical) Trials and Tribul-ations
In the category of supplements that have enjoyed use as aphrodisiacs, Tribulus terrestris (also called caltrop, goat’s head, gokshura, or puncture vine) has a long history, having seen wide use in both Traditional Chinese Medicine and in Ayurveda.
It’s been used for other purposes too, and has been considered a “general wellness” plant.
So, what does the science say?
Good news: very conclusive evidence!
Bad news: the conclusion is not favorable…
Scientists are known for their careful use of clinical language, and it’s very rare for a study/review to claim something as proven (scientists leave journalists to do that part), and in this case, when it comes to Tribulus’s usefulness as a testosterone-enhancing libido-boosting supplement…
❝analysis of empirical evidence from a comprehensive review of available literature proved this hypothesis wrong❞
Strong words! You can read it in full here; they do make some concessions along the way (e.g. mentioning unclear or contradictory findings, suggesting that it may have some effect, but by an as-yet unknown mechanism if it does—although some potential effect on nitric oxide levels has been hypothesized, which is reasonable if so, as NO does feature in arousal-signalling), but the general conclusion is “no, this doesn’t have androgen-enhancing properties”:
Pro-sexual and androgen enhancing effects of Tribulus terrestris L.: Fact or Fiction
That’s a review though, what about taking a look at a representative RCT? Here we go:
❝Tribulus terrestris was not more effective than placebo on improving symptoms of erectile dysfunction or serum total testosterone❞
As a performance-enhancer in sport
We’ll be brief here: it doesn’t seem to work and it may not be safe:
Insights into Supplements with Tribulus Terrestris used by Athletes
From sport, into general wellness?
Finally, a study that finds it may be useful for something!
❝Overall, participants supplemented with TT displayed significant improvements in lipid profile. Inflammatory and hematological biomarkers showed moderate beneficial effects with no significant changes on renal biomarkers. No positive effects were observed on the immune system response. Additionally, no TT-induced toxicity was reported.
In conclusion, there was no clear evidence of the beneficial effects of TT supplementation on muscle damage markers and hormonal behavior.❞
About those lipids…
Animal studies have shown that it may not only improve lipid profiles, but also may partially repair the endothelial dysfunction resulting from hyperlipidemia:
Want to try some?
In the unlikely event that today’s research review has inspired you with an urge to try Tribulus terrestris, here’s an example product on Amazon
If on the other hand you’d like to actually increase testosterone levels, then we suggest:
Topping Up Testosterone? ← a previous main feature did earlier this year
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What does it mean to be transgender?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Transgender media coverage has surged in recent years for a wide range of reasons. While there are more transgender television characters than ever before, hundreds of bills are targeting transgender people’s access to medical care, sports teams, gender-specific public spaces, and other institutions.
Despite the increase in conversation about the transgender community, public confusion around transgender identity remains.
Read on to learn more about what it means to be transgender and understand challenges transgender people may face.
What does it mean to be transgender?
Transgender—or “trans”—is an umbrella term for people whose gender identity or gender expression does not conform to their sex assigned at birth. People can discover they are trans at any age.
Gender identity refers to a person’s inner sense of being a woman, a man, neither, both, or something else entirely. Trans people who don’t feel like women or men might describe themselves as nonbinary, agender, genderqueer, or two-spirit, among other terms.
Gender expression describes the way a person communicates their gender through their appearance—such as their clothing or hairstyle—and behavior.
A person whose gender expression doesn’t conform to the expectations of their assigned sex may not identify as trans. The only way to know for sure if someone is trans is if they tell you.
Cisgender—or “cis”—describes people whose gender identities match the sex they were assigned at birth.
How long have transgender people existed?
Being trans isn’t new. Although the word “transgender” only dates back to the 1960s, people whose identities defy traditional gender expectations have existed across cultures throughout recorded history.
How many people are transgender?
A 2022 Williams Institute study estimates that 1.6 million people over the age of 13 identify as transgender in the United States.
Is being transgender a mental health condition?
No. Conveying and communicating about your gender in a way that feels authentic to you is a normal and necessary part of self-expression.
Social and legal stigma, bullying, discrimination, harassment, negative media messages, and barriers to gender-affirming medical care can cause psychological distress for trans people. This is especially true for trans people of color, who face significantly higher rates of violence, poverty, housing instability, and incarceration—but trans identity itself is not a mental health condition.
What is gender dysphoria?
Gender dysphoria describes a feeling of unease that some trans people experience when their perceived gender doesn’t match their gender identity, or their internal sense of gender. A 2021 study of trans adults pursuing gender-affirming medical care found that most participants started experiencing gender dysphoria by the time they were 7.
When trans people don’t receive the support they need to manage gender dysphoria, they may experience depression, anxiety, social isolation, suicidal ideation, substance use disorder, eating disorders, and self-injury.
How do trans people manage gender dysphoria?
Every trans person’s experience with gender dysphoria is unique. Some trans people may alleviate dysphoria by wearing gender-affirming clothing or by asking others to refer to them by a new name and use pronouns that accurately reflect their gender identity. The 2022 U.S. Trans Survey found that nearly all trans participants who lived as a different gender than the sex they were assigned at birth reported that they were more satisfied with their lives.
Some trans people may also manage dysphoria by pursuing medical transition, which may involve taking hormones and getting gender-affirming surgery.
Access to gender-affirming medical care has been shown to reduce the risk of depression and suicide among trans youth and adults.
To learn more about the trans community, visit resources from the National Center for Transgender Equality, the Trevor Project, PFLAG, and Planned Parenthood.
If you or anyone you know is considering suicide or self-harm or is anxious, depressed, upset, or needs to talk, call the Suicide & Crisis Lifeline at 988 or text the Crisis Text Line at 741-741. For international resources, here is a good place to begin.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: