How To Triple Your Breast Cancer Survival Chances
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Keeping Abreast Of Your Cancer Risk
It’s the kind of thing that most people think won’t happen to them. And hopefully, it won’t!
But…
- Anyone (who has not had a double mastectomy*, anyway) can get breast cancer.
- *and even this depends on the type of double mastectomy and other circumstances, and technically there will always be a non-zero risk, because of complicating factors.
- Breast cancer, if diagnosed early (before it spreads), has a 98% survival rate.
- That survival rate drops to 31% if diagnosed after it has spread through the body.
(The US CDC’s breast cancer “stat bite” page has more stats and interactive graphs, so click here to see those charts and get the more detailed low-down on mortality/survival rates with various different situations)
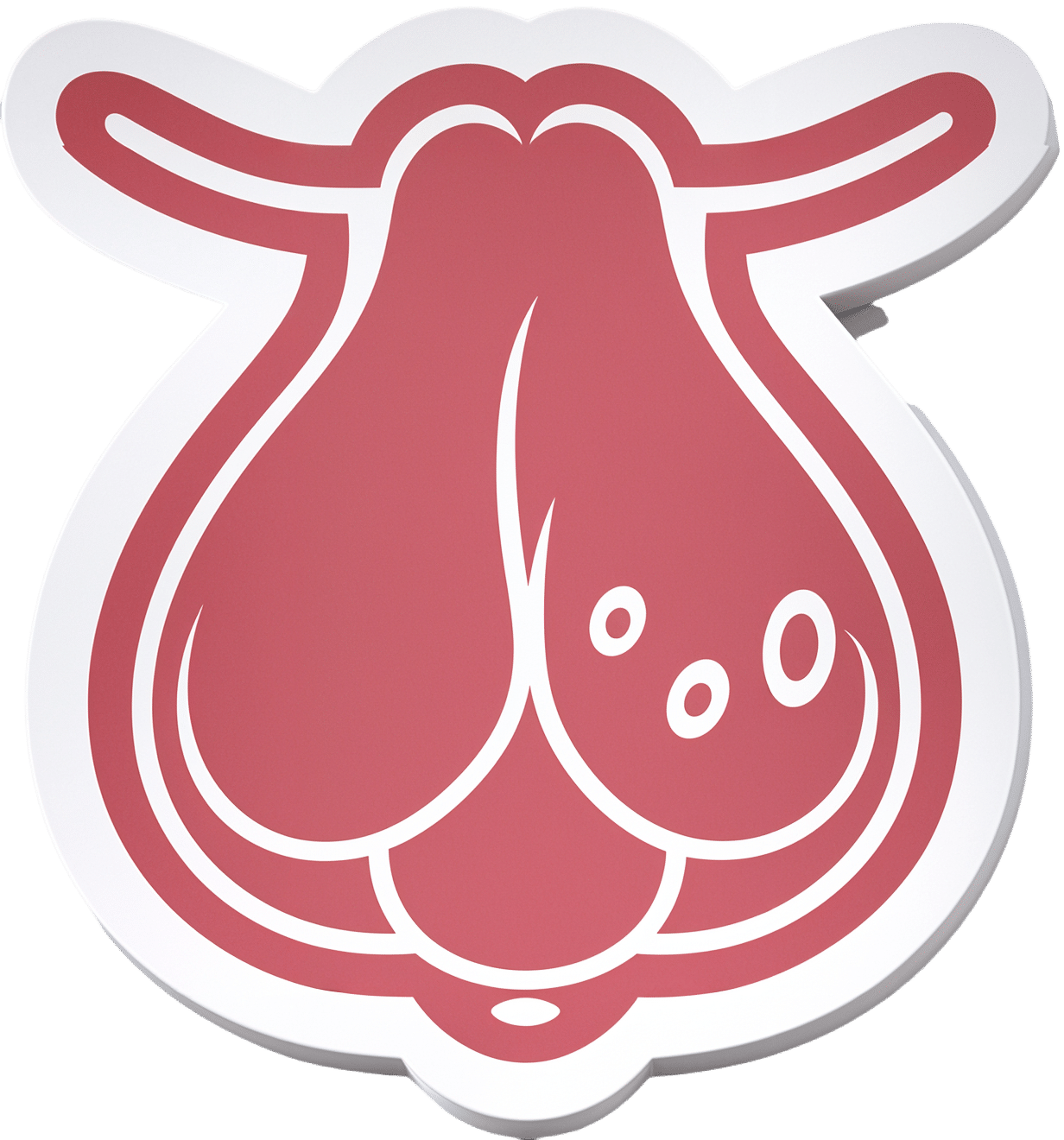
We think that the difference between 98% and 31% survival rates is more than enough reason to give ourselves a monthly self-check at the very least! You’ve probably seen how-to diagrams before, but here are instructions for your convenience:
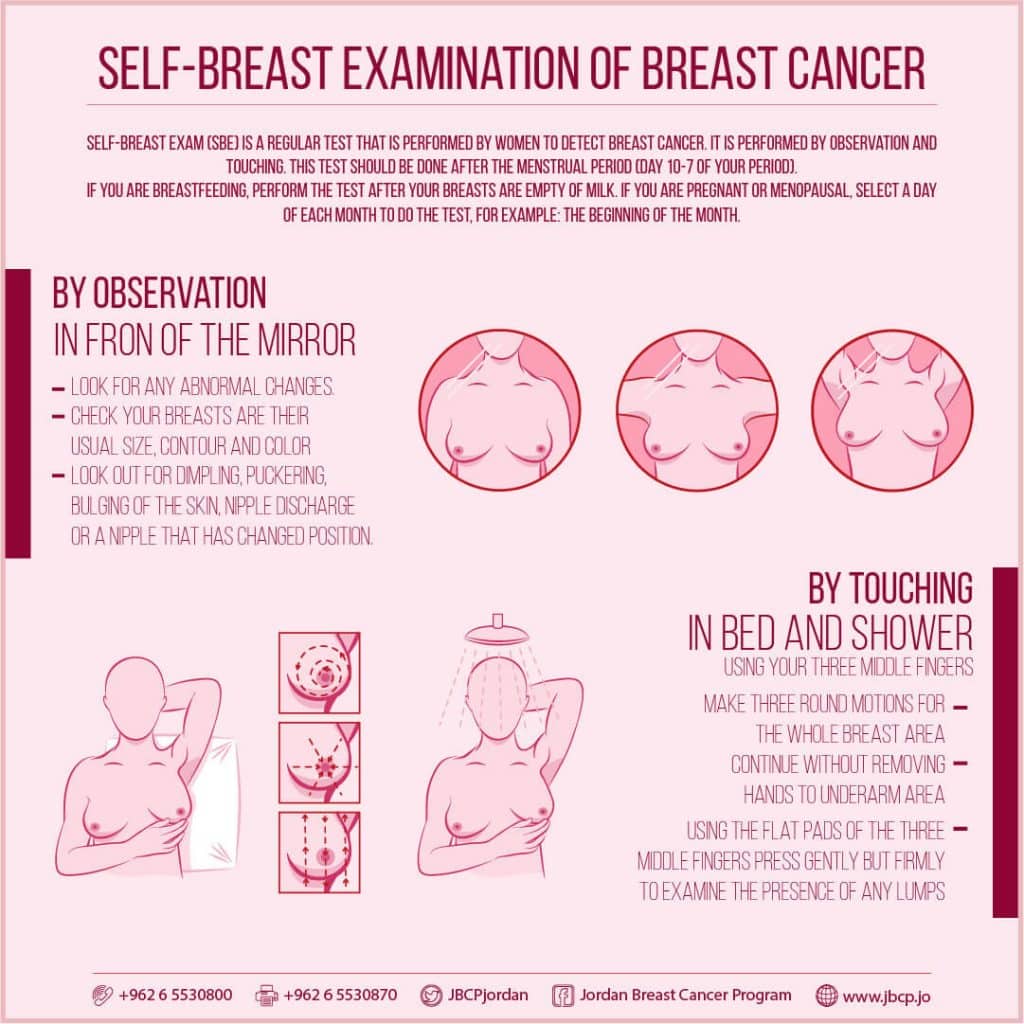
(This graphic was created by the Jordan Breast Cancer Program—check them out, as they have lots of resources)
If you don’t have the opportunity to take matters into your own hands right now, rather than just promise yourself “I’ll do that later”, take this free 4-minute Breast Health Assessment from Aurora Healthcare. Again, we think the difference early diagnosis can make to your survival chances make these tests well worth it:
Click Here To Take The Free 4-Minute Breast Health Assessment!
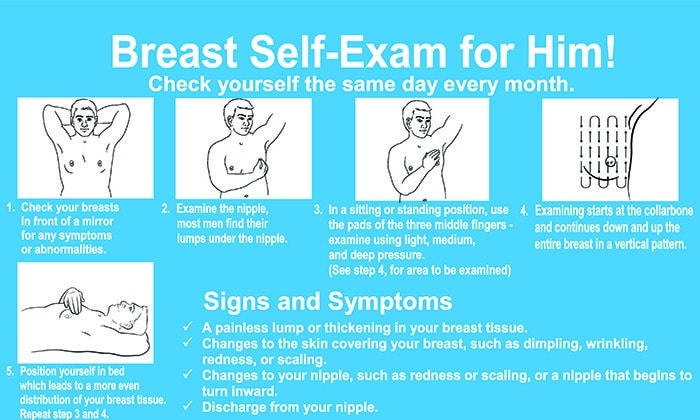
Lest we forget, men can also get breast cancer (the CDC has a page for men too), especially if over 50. But how do you check for breast cancer, when you don’t have breasts in the commonly-understood sense of the word?
So take a moment to do this (yes, really actually do it!), and set a reminder in your calendar to repeat it monthly—there really is no reason not to!
Take care of yourself; you’re important.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cashew & Chickpea Balti
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to curries, the humble balti is perhaps the best when you don’t have all day to let something simmer. Filled with healthful spices, this one also comes complete with lots of fiber as well as healthy proteins and fats, with most of its calories coming from the nuts themselves, and the haricot paste base makes for a deliciously creamy curry without having to add anything unhealthy.
You will need
- 1 cup cashews, soaked in warm water for at least 5 minutes, and drained (if allergic, omit)
- 1 can chickpeas (keep the water)
- 1 can haricot beans (keep the water)
- 1 can crushed tomatoes
- 2 medium (or 3 small) red onions, sliced
- red or green chilis, quantity per your preference re heat, chopped
- ½ bulb garlic, crushed
- ½ oz fresh ginger, peeled and finely chopped
- 1 tbsp tomato paste
- 1 tbsp garam masala
- 1 tbsp ground coriander
- 1 tbsp black pepper, coarse ground
- 2 tsp turmeric
- 1 tsp mustard seeds (if allergic, omit)
- 1 tsp sweet cinnamon
- 1 tsp coriander seeds
- ½ tsp MSG or 1 tsp low-sodium salt
- Avocado oil, for frying (extra virgin olive-oil, or cold-pressed coconut oil, are fine alternatives)
- Garnish: handful fresh cilantro, chopped (or parsley, if you have the “cilantro tastes like soap” gene)
Method
(we suggest you read everything at least once before doing anything)
1) Heat a little oil in a large sauté pan (we’re going to need space to work; a large wok is traditional but a sauté pan is convenient), and add the garlic, ginger, mustard seeds, and coriander seeds, stirring for about 2 minutes, then add the onions and chilis, stirring for another 3 minutes. The onions and chilis won’t be fully cooked yet, but that’s fine, we just needed to get them started.
2) Add the crushed tomatoes, stirring them in, and when they get to temperature, turn the heat down to a simmer.
3) Add the chickpeas to the pan, but separately put the chickpea water into a high-speed blender.
4) Add the haricot beans, including the water they came in, to the high-speed blender, as well as the tomato paste and the remaining spices (including the MSG or salt), and blend on high until smooth. Add the curry paste (that’s what you’ve just made in the blender) to the pan, and stir in well.
5) Add the cashews, stirring in well. Taste, and adjust any spices if necessary for your liking. If the onions still aren’t fully cooked, let them simmer until they are, but it shouldn’t take long.
10almonds tip: if perchance you made it too spicy, you can add a little lime juice and the acidity will counteract the heat. Adding lemon juice, lime juice, or some kind of vinegar (depending on what works with the flavor profile of your recipe) is a good last resort to have up your sleeve for fixing a dish that got too spicy.
6) Add the garnish, and serve—we recommend serving it with our Tasty Versatile Rice, but any carb is fine.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Why You Should Diversify Your Nuts!
- Three Daily Servings of Beans?
- Cashew Nuts vs Coconut – Which is Healthier?
- What Matters Most For Your Heart?
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we hit 5/5 again today!
Take care!
Share This Post
-
Make Your Vegetables Work Better Nutritionally
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most people know that boiling vegetables to death is generally not best for them, but raw isn’t always best either, and if we want to not sabotage our food, then there’s more to bear in mind than “just steam them, then”.
So, what should we keep in mind?
Water solubility
Many nutrients are water-soluble, including vitamin C, vitamin B-complex (as in, the collection of B-vitamins), and flavonoids, as well as many other polyphenols.
This means that if you cook your vegetables (which includes beans, lentils, etc) in water, a lot of the nutrients will go into the water, and be lost if you then drain that.
There are, thus, options;
- Steaming, yes
- Use just enough water to slow-cook or pressure-cook things that are suitable for slow-cooking, or pressure-cooking such as those beans and lentils. That way, when it’s done, there’s no excess water to drain, and all the nutrients are still in situ.
- Use as much water as you like, but then keep the excess water to make a soup, sauce, or broth.
- Use a cooking method other than water, where appropriate. For example, roasting peppers is a much better idea than roasting dried pulses.
- Consume raw, where appropriate.
Fat solubility
Many nutrients are fat-soluble, including vitamins A, D, E, and K, as well as a lot of carotenoids (including heavy-hitters lycopene and β-carotene) and many other polyphenols.
We’re now going to offer almost the opposite advice to that we had about water solubility. This is because unless they are dried, vegetables already contain water, whereas many contain only trace amounts of fat. Consequently, the advice this time is to add fat.
There are options:
- Cook with a modest amount of your favorite healthy cooking oil (our general go-to is extra-virgin olive oil, but avocado oil is great especially for higher temperature cooking, and an argument can be made for coconut oil sometimes)
- Remember that this goes for roasting, too. Brush those vegetables with a touch of olive oil, and not only will they be delicious, they’ll be more nutritious, too.
- Drizzle some the the above, if you’re serving things raw and it’s appropriate. This goes also for things like salads, so dress them!
- Enjoy your vegetables alongside healthy fatty foods such as nuts and seeds (or fatty animal products, if you eat those; fatty fish is a fine option here, in moderation, as are eggs, or fermented dairy products).
For a deeper understanding: Can Saturated Fats Be Healthy?
Do not, however, deep-fry your foods unless it’s really necessary and then only for an occasional indulgence that you simply accept will be unhealthy. Not only is deep-frying terrible for the health in a host of ways (ranging from an excess of oil in the resultant food, to acrylamide, to creating Advanced Glycation End-products*), but also those fat-soluble nutrients? Guess where they’ll go. And unlike with the excess vegetable-cooking water that you can turn into soup or whatever, we obviously can’t recommend doing that with deep-fryer oil.
*see also: Are You Eating AGEs?
Temperature sensitivity
Many nutrients are sensitive to temperature, including vitamin C (breaks down when exposed to high temperatures) and carotenoids (are released when exposed to higher temperatures). Another special case is ergothioneine, “the longevity vitamin” that’s not a vitamin, found in mushrooms, which is also much more bioavailable when cooked.
So, if you’re eating something for vitamin C, then raw is best if that’s a reasonable option.
And if it’s not a reasonable option? Well, then you can either a) just cope with the fact it’s going to have less vitamin C in it, or b) cook it as gently and briefly as reasonably possible.
On the other hand, if you’re eating something for carotenoids (especially including lycopene and β-carotene), or ergothioneine, then cooked is best.
Additionally, if your food is high in oxalates (such as spinach), and you don’t want it to be (for example because you have kidney problems, which oxalates can exacerbate, or would like to get more calcium out of the spinach and into your body, which which oxalic acid would inhibit), then cooked is best, as it breaks down the oxalates.
Same goes for phytates, another “anti-nutrient” found in some whole grains (such as rice and wheat); cooking breaks it down, therefore cooked is best.
This latter is not, however, applicable in the case of brown rice protein powder, for those who enjoy that—because phytates aren’t found in the part of the rice that’s extracted to make that.
And as for brown rice itself? Does contain phytates… Which can be reduced by soaking and heating, preferably both, to the point that the nutritional value is better than it would have been had there not been phytic acid present in the first place; in other words: cooked is best.
You may be wondering: “who is eating rice raw?” and the answer is: people using rice flour.
See: Brown Rice Protein: Strengths & Weaknesses
Want to know more?
Here’s a great rundown from Dr. Rosalind Gibson, Dr. Leah Perlas, and Dr. Christine Hotz:
Improving the bioavailability of nutrients in plant foods at the household level
Enjoy!
Share This Post
-
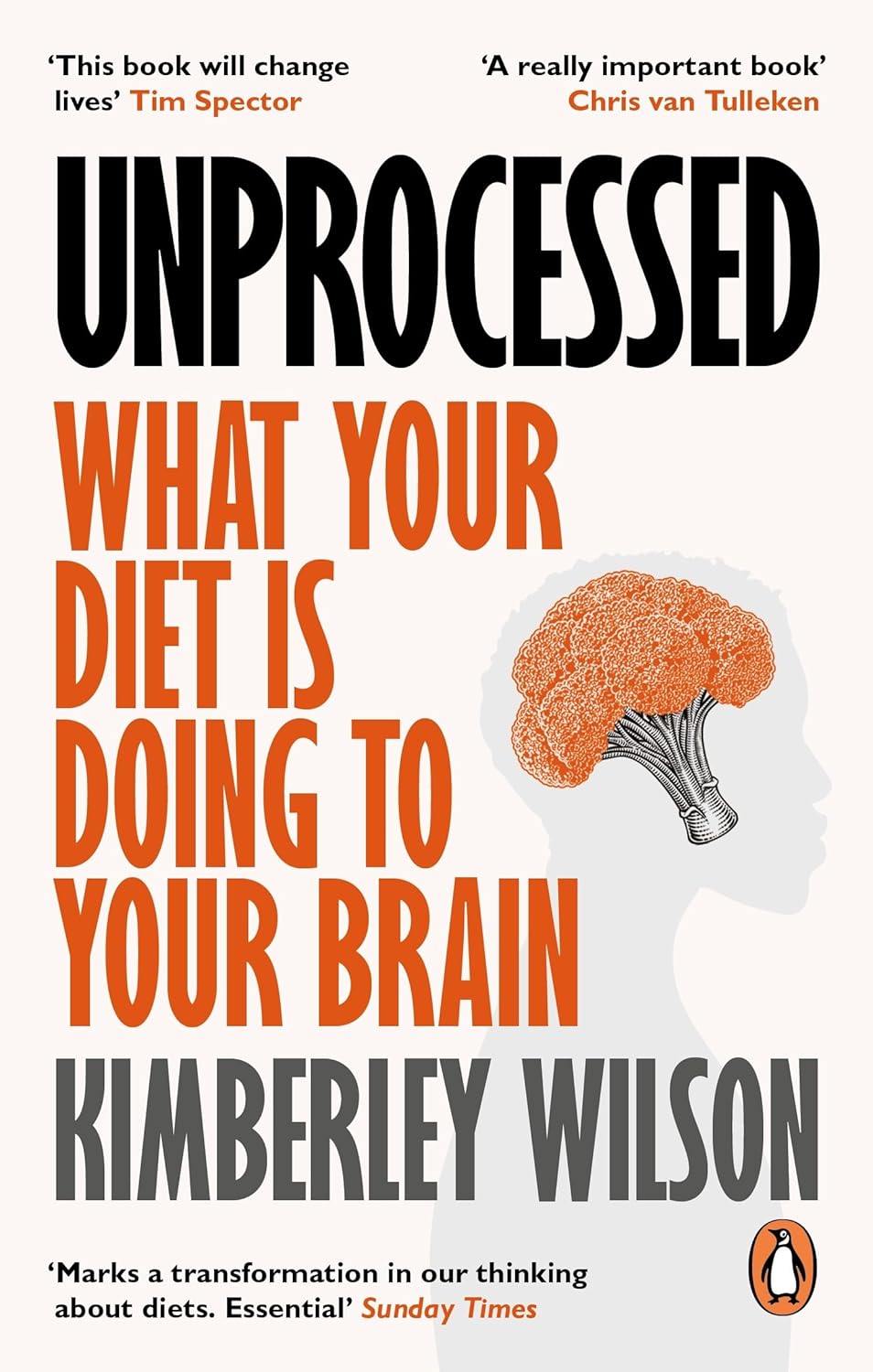
Unprocessed – by Kimberly Wilson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this is not: hundreds of pages to say “eat less processed food”. That is, of course, also advisable (and indeed, is advised in the book too), but there’s a lot more going on here too.
Though not a doctor, the author is a psychologist who brings a lot of data to the table, especially when it comes to the neurophysiology at hand, what forgotten micronutrients many people are lacking, and what trends in society worsen these deficiencies in the population at large.
If you only care about the broadest of take-away advice, it is: eat a diet that’s mostly minimally processed plants and some oily fish, watch out for certain deficiencies in particular, and increase dietary intake of them where necessary (with taking supplements as a respectable next-best remedy).
On which note, a point of criticism is that there’s some incorrect information about veganism and brain health; she mentions that DHA is only found in fish (in fact, fish get it from algae, which has it, and is the basis of many vegan omega-3 supplements), and the B12 is found only in animals (also found in yeast, which is not an animal, as well as various bacteria in soil, and farm animals get their B12 from supplements these days anyway, so it is arguable that we could keep things simpler by just cutting out the middlecow).
However, the strength of this book really is in the delivery of understanding about why certain things matter. If you’re told “such-and-such is good for the brain”, you’ll up your intake for 1–60 days, depending on whether you bought a supermarket item or ordered a batch of supplements. And then you’ll forget, until 6–12 months later, and you’ll do it again. On the other hand, if you understand how something is good or bad for the brain, what it does (for good or ill) on a cellular level, the chemistry and neurophysiology at hand, you’ll make new habits for life.
The style is middle-range pop-science; by this we mean there are tables of data and some long words that are difficult to pronounce, but also it’s not just hard science throughout—there’s (as one might expect from an author who is a psychologist) a lot about the psychology and sociology of why many people make poor dietary decisions, and the things governments often do (or omit doing) that affect this adversely—and how we can avoid those traps as individuals (unless we be incarcerated or such).
As an aside, the author is British, so governmental examples are mostly UK-based, but it doesn’t take a lot to mentally measure that against what the governments of, for example, the US or Canada do the same or differently.
Bottom line: there’s a lot of great information about brain health here; the strongest parts are whether the author stays within her field (psychology encompasses such diverse topics as neurophysiology and aspects of sociology, but not microbiology, for example). If you want to learn about the physiology of brain health and enjoy quite a sociopolitical ride along the way, this one’s a good one for that.
Click here to check out Unprocessed, and make the best choices for you!
Share This Post
Related Posts
-
How To Boost Your Memory Immediately (Without Supplements)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Boost Your Memory (Without Supplements)
While we do recommend having a good diet and taking advantage of various supplements that have been found to help memory, that only gets so much mileage. With that in mind…
First, how good is your memory? Take This 2-Minute Online Test
Now, that was a test of short term memory, which tends to be the most impactful in our everyday life.
It’s the difference between “I remember the address of the house where I grew up” (long-term memory) and “what did I come to this room to do?” (short-term memory / working memory)
First tip:
When you want to remember something, take a moment to notice the details. You can’t have a madeleine moment years later if you wolfed down the madeleines so urgently they barely touched the sides.
This goes for more than just food, of course. And when facing the prospect of age-related memory loss in particular, people tend to be afraid not of forgetting their PIN code, but their cherished memories of loved ones. So… Cherish them, now! You’ll struggle to cherish them later if you don’t cherish them now. Notice the little details as though you were a painter looking at a scene for painting. Involve more senses than just sight, too!
If it’s important, relive it. Relive it now, relive it tomorrow. Rehearsal is important to memory, and each time you relive a memory, the deeper it gets written into your long-term memory until it becomes indelible to all but literal brain damage.
Second tip:
Tell the story of it to someone else. Or imagine telling it to someone else! (You brain can’t tell the difference)
And you know how it goes… Once you’ve told a story a few times, you’ll never forget it later. Isn’t your life a story worth telling?
Many people approach memory like they’re studying for a test. Don’t. Approach it like you’re preparing to tell a story, or give a performance. We are storytelling creatures at heart, whether or not we realize it.
What do you do when you find yourself in a room and wonder why you went there? (We’ve all been there!) You might look around for clues, but if that doesn’t immediately serve, your fallback will be retracing your steps. Literally, physically, if needs be, but at least mentally. The story of how you got there is easier to remember than the smallest bit of pure information.
What about when there’s no real story to tell, but we still need to remember something?
Make up a story. Did you ever play the game “My granny went to market” as a child?
If not, it’s a collaborative memory game in which players take turns adding items to a list, “My granny went to market and bought eggs”, My granny went to market and bought eggs and milk”, “my granny went to market and bought eggs and milk and flour” (is she making a cake?), “my granny went to market and bought eggs and milk and flour and shoe polish” (what image came to mind? Use that) “my granny went to market and bought eggs and milk and flour and shoe polish and tea” (continue building the story in your head), and so on.
When we actually go shopping, if we don’t have a written list we may rely on the simple story of “what I’m going to cook for dinner” and walking ourselves through that story to ensure we get the things we need.
This is because our memory thrives (and depends!) on connections. Literal synapse connections in the brain, and conceptual contextual connections in your mind. The more connections, the better the memory.
Now imagine a story: “I went to Stonehenge, but in the background was a twin-peaked mountain blue. I packed a red suitcase, placing a conch shell inside it, when suddenly I heard a trombone, and…” Ring any bells? These are example items from the memory test earlier, though of course you may have seen different things in a different order.
So next time you want to remember things, don’t study as though for a test. Prepare to tell a story!
Try going through the test again, but this time, ignore their instructions because we’re going to use the test differently than intended (we’re rebels like that). Don’t rush, and don’t worry about the score this time (or even whether or not you saw a given image previously), but instead, build a story as you go. We’re willing to bet that after it, you can probably recite most of the images you saw in their correct order with fair confidence.
Here’s the link again: Take The Same Test, But This Time Make It Story-Worthy!
Again, ignore what it says about your score this time, because we weren’t doing that this time around. Instead, list the things you saw.
What you were just able to list was the result of you doing story-telling with random zero-context images while under time pressure.
Imagine what you can do with actual meaningful memories of your ongoing life, people you meet, conversations you have!
Just… Take the time to smell the roses, then rehearse the story you’ll tell about them. That memory will swiftly become as strong as any memory can be, and quickly get worked into your long-term memory for the rest of your days.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cool As A Cucumber
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cucumber Extract Beats Glucosamine & Chondroitin… At 1/135th Of The Dose?!
Do you take glucosamine & chondroitin supplements for your bone-and-joint health?
Or perhaps, like many, you take them intermittently because they mean taking several large tablets a day. Or maybe you don’t take them at all because they generally contain ingredients derived from shellfish?
Cucumber extract has your back! (and your knees, and your hips, and…)
It’s plant-derived (being from botanical cucumbers, not sea cucumbers, the aquatic animal!) and requires only 1/135th of the dosage to produce twice the benefits!
Distilling the study to its absolute bare bones for your convenience:
- Cucumber extract (10mg) was pitted against glucosamine & chondroitin (1350mg)
- Cucumber extract performed around 50% better than G&C after 30 days
- Cucumber extract performed more than 200% better than G&C after 180 days
In conclusion, this study indicates that, in very lay terms:
Cucumber extract blows glucosamine & chondroitin out of the water as a treatment and preventative for joint pain
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Overcome Front-Of-Hip Pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Alyssa Kuhn, physiotherapist, demonstrates how:
One, two, three…
One kind of pain affects a lot of related things: hip pain has an impact on everything that’s connected to the pelvis, which is basically the rest of the body, but especially the spine itself. For this reason, it’s critical to keep it in as good condition as possible.
Two primary causes of hip stiffness and pain:
- Anterior pelvic tilt due to posture, weight distribution, or pain. This tightens the front muscles and weakens the back muscles.
- Prolonged sitting, which tightens the hip muscles due to inactivity.
Three exercises are recommended by Dr. Kuhn to relieve pain and stiffness:
- Bridge exercise:
- Lie on a firm surface with your knees bent.
- Push through your feet, engage your hamstrings, and flatten your lower back.
- Hold for 3–5 seconds, relax, and repeat (10–20 reps).
- Wall exercise with arms:
- Stand with your lower back against the wall, feet a step away.
- Tilt your hips backwards, keeping your lower back in contact with the wall.
- Alternate lifting one arm at a time while maintaining back contact with the wall (10–20 reps).
- Wall exercise with legs:
- Same stance as the previous exercise but wider now.
- Lift one heel at a time while keeping your hips stable and your back against the wall.
- Practice for 30–60 seconds, maintaining good form.
As ever, consistency is key for long-term relief. Dr. Kuhn recommends doing these regularly, especially before any expected periods of prolonged sitting (e.g. at desk, or driving, etc). And of course, do try to reduce, or at least break up, those sitting marathons if you can.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: