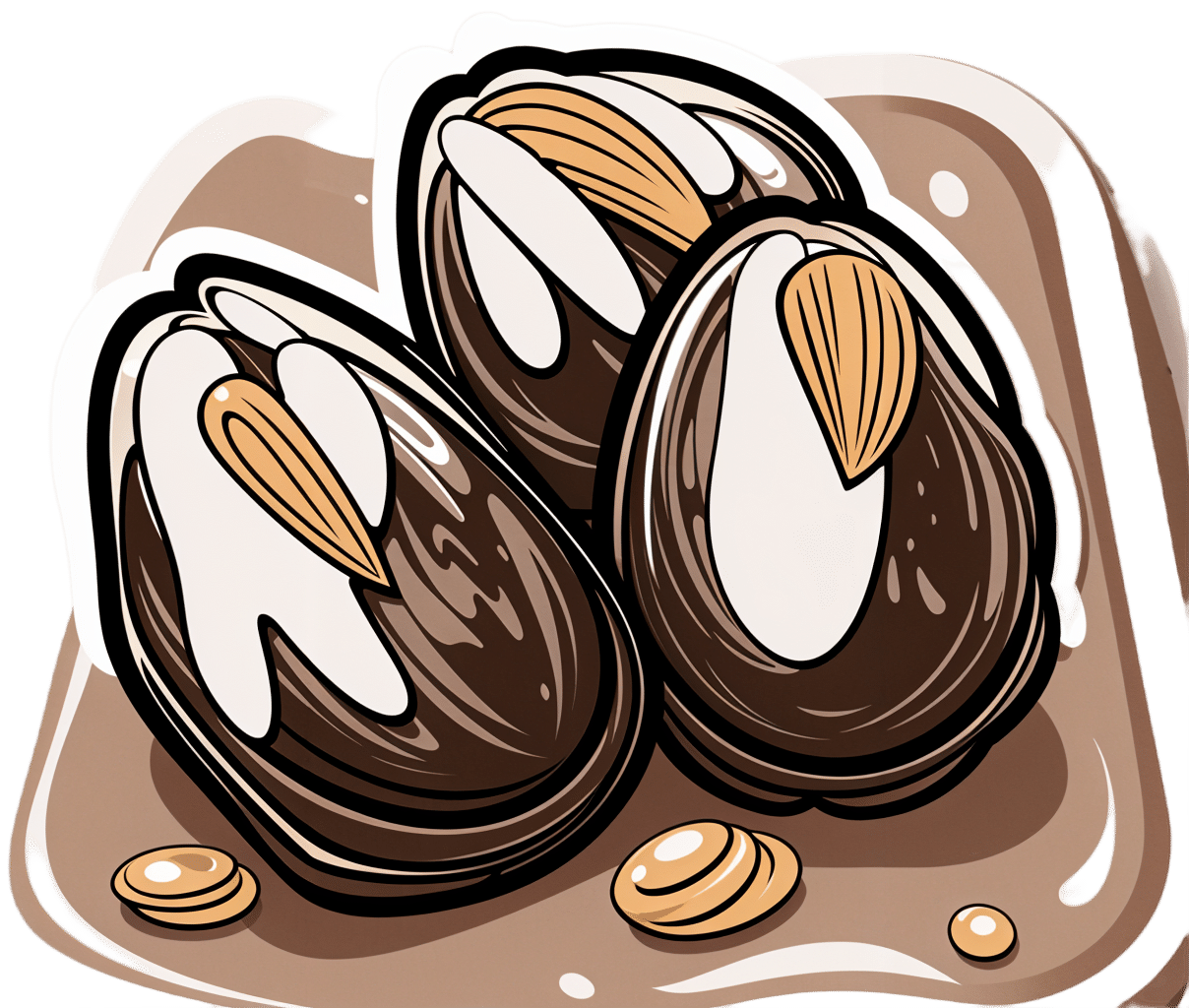
Tiramisu Crunch Bites
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s coffee, it’s creamy, it’s nutty, it’s chocolatey, what’s not to love? It has all the well-loved flavors of tiramisu, but this recipe is a simple one, and it’s essentially stuffed dates in a way you’ve never had them before. They’re delectable, decadent, and decidedly good for your health. These things are little nutrient-bombs that’ll keep you reaching for more.
You will need
- Coffee (we will discuss this)
- 150g (5.5oz) mascarpone (if vegan or lactose-intolerant, can be substituted with vegan varieties, or at a pinch, pressed silken tofu)
- 500g (1lb) dates (Medjool are ideal)
- Twice as many almonds as you have dates
- 50g (2oz) dark chocolate (the darkest, bitterest, you can find)
- Edible flower petals if you can source them (some shops sell dried rose petals for this purpose)
Method
(we suggest you read everything at least once before doing anything)
1) Take the mascarpone and whisk (or blend) it with the coffee. What kind of coffee, you ask? Many will use instant coffee (1tbsp granules mixed with enough boiling water to dissolve it), and that is actually healthiest (counterintuitive but true) but if you care for flavor over health, and have the means to make espresso, make it ristretto (so, stop it halfway through filling up an espresso cup), let it cool, and use that. Absolute bonus for flavor (not for health): if you have the means to make Turkish coffee, use an equivalent amount of that (again, cooled).
You will now have coffee-flavoured mascarpone. It’s great for your gut and full of antioxidant polyphenols. Set it aside for the moment.
2) Take the dark chocolate and melt it. Please don’t microwave it or try to do it in a pan directly over the hob; instead, you will need to use a Bain-Marie. If you don’t have one made-for-purpose, you can place a metal or heatproof glass bowl in a saucepan, with something to stop it from touching the floor of the pan. Then boil water in the pan (without letting the water get into the bowl), and melt the chocolate in the bowl—this will allow you to melt it evenly without burning the chocolate.
You will now have melted dark chocolate. It has its own set of polyphenols, and is great for everything from the brain to the gut microbiome.
3) Cut the dates lengthways on one side and remove the stone. Stuff them carefully with the coffee-flavored mascarpone (you can use a teaspoon, or use a piping kit if you have one). Add a couple of almonds to each one. Place them all on a big plate, and drizzle the melted chocolate over them. Add the petals if you have them.
The dates and almonds deliver extra vitamins and minerals in abundance (not to mention, lots of fiber), and also are an amazing combination even just by themselves. With the mascarpone and chocolate added, this winning on new levels. We’re not done yet, though…
4) Chill them in the fridge for about 30 minutes.
Serve!

Learn more
For those interested in some of the science of what we have going on today:
- Make The Heart-Healthiest Coffee ← this is about cafestol content and why instant is heart-healthiest (alas)
- The Bitter Truth About Coffee (Or Is It) ← this is about the health benefits (and some risks, but mostly benefits) of coffee
- Why You Should Diversify Your Nuts ← almonds are a top-tier choice, but other nuts are good too! This recipe could work well with hazelnuts, for example (we wouldn’t call it “tiramisu crunch bites” in that case, though, since the flavor profile would change)
- Which Sugars Are Healthier, And Which Are Just The Same? ← for any worrying “aren’t dates sugary, though?”
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Body on Fire – by Dr. Monica Aggarwal and Dr. Jyothi Rao
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are times when you do really need a doctor, not a dietician. But there are also times when a doctor will prescribe something for the symptom, leaving the underlying issue untouched. If only there were a way to have the best of both worlds!
That’s where Drs. Rao and Aggarwal come in. They’re both medical doctors… with a keen interest in nutrition and healthy lifestyle changes to make us less sick such that we have less need to go to the doctor at all.
Best of all, they understand—while some things are true for everyone—there’s not a one-size-fits all diet or exercise regime or even sleep setup.
So instead, they take us hand-in-hand (chapter by chapter!) through the various parts of our life (including our diet) that might need tweaking. Each of these changes, if taken up, promise a net improvement that becomes synergistic with the other changes. There’s a degree of biofeedback involved, and listening to your body, to be sure of what’s really best for you, not what merely should be best for you on paper.
The writing style is accessible while science-heavy. They don’t assume prior knowledge, and/but they sure deliver a lot. The book is more text than images, but there are plenty of medical diagrams, explanations, charts, and the like. You will feed like a medical student! And it’s very much worth studying.
Bottom line: highly recommendable even if you don’t have inflammation issues, and worth its weight in gold if you do.
Share This Post
-
Can kimchi really help you lose weight? Hold your pickle. The evidence isn’t looking great
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fermented foods have become popular in recent years, partly due to their perceived health benefits.
For instance, there is some evidence eating or drinking fermented foods can improve blood glucose control in people with diabetes. They can lower blood lipid (fats) levels and blood pressure in people with diabetes or obesity. Fermented foods can also improve diarrhoea symptoms.
But can they help you lose weight, as a recent study suggests? Let’s look at the evidence.
Remind me, what are fermented foods?
Fermented foods are ones prepared when microbes (bacteria and/or yeast) ferment (or digest) food components to form new foods. Examples include yoghurt, cheese, kefir, kombucha, wine, beer, sauerkraut and kimchi.
As a result of fermentation, the food becomes acidic, extending its shelf life (food-spoilage microbes are less likely to grow under these conditions). This makes fermentation one of the earliest forms of food processing.
Fermentation also leads to new nutrients being made. Beneficial microbes (probiotics) digest nutrients and components in the food to produce new bioactive components (postbiotics). These postbiotics are thought to contribute to the health benefits of the fermented foods, alongside the health benefits of the bacteria themselves.
What does the evidence say?
A study published last week has provided some preliminary evidence eating kimchi – the popular Korean fermented food – is associated with a lower risk of obesity in some instances. But there were mixed results.
The South Korean study involved 115,726 men and women aged 40-69 who reported how much kimchi they’d eaten over the previous year. The study was funded by the World Institute of Kimchi, which specialises in researching the country’s national dish.
Eating one to three servings of any type of kimchi a day was associated with a lower risk of obesity in men.
Men who ate more than three serves a day of cabbage kimchi (baechu) were less likely to have obesity and abdominal obesity (excess fat deposits around their middle). And women who ate two to three serves a day of baechu were less likely to have obesity and abdominal obesity.
Eating more radish kimchi (kkakdugi) was associated with less abdominal obesity in both men and women.
However, people who ate five or more serves of any type of kimchi weighed more, had a larger waist sizes and were more likely to be obese.
The study had limitations. The authors acknowledged the questionnaire they used may make it difficult to say exactly how much kimchi people actually ate.
The study also relied on people to report past eating habits. This may make it hard for them to accurately recall what they ate.
This study design can also only tell us if something is linked (kimchi and obesity), not if one thing causes another (if kimchi causes weight loss). So it is important to look at experimental studies where researchers make changes to people’s diets then look at the results.
How about evidence from experimental trials?
There have been several experimental studies looking at how much weight people lose after eating various types of fermented foods. Other studies looked at markers or measures of appetite, but not weight loss.
One study showed the stomach of men who drank 1.4 litres of fermented milk during a meal took longer to empty (compared to those who drank the same quantity of whole milk). This is related to feeling fuller for longer, potentially having less appetite for more food.
Another study showed drinking 200 millilitres of kefir (a small glass) reduced participants’ appetite after the meal, but only when the meal contained quickly-digested foods likely to make blood glucose levels rise rapidly. This study did not measure changes in weight.
Kefir, a fermented milk drink, reduced people’s appetite.
Ildi Papp/ShutterstockAnother study looked at Indonesian young women with obesity. Eating tempeh (a fermented soybean product) led to changes in an appetite hormone. But this did not impact their appetite or whether they felt full. Weight was not measured in this study.
A study in South Korea asked people to eat about 70g a day of chungkookjang (fermented soybean). There were improvements in some measures of obesity, including percentage body fat, lean body mass, waist-to-hip ratio and waist circumference in women. However there were no changes in weight for men or women.
A systematic review of all studies that looked at the impact of fermented foods on satiety (feeling full) showed no effect.
What should I do?
The evidence so far is very weak to support or recommend fermented foods for weight loss. These experimental studies have been short in length, and many did not report weight changes.
To date, most of the studies have used different fermented foods, so it is difficult to generalise across them all.
Nevertheless, fermented foods are still useful as part of a healthy, varied and balanced diet, particularly if you enjoy them. They are rich in healthy bacteria, and nutrients.
Are there downsides?
Some fermented foods, such as kimchi and sauerkraut, have added salt. The latest kimchi study said the average amount of kimchi South Koreans eat provides about 490mg of salt a day. For an Australian, this would represent about 50% of the suggested dietary target for optimal health.
Eating too much salt increases your risk of high blood pressure, heart disease and stroke.
Evangeline Mantzioris, Program Director of Nutrition and Food Sciences, Accredited Practising Dietitian, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Keep Inflammation At Bay
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How to Prevent (or Reduce) Inflammation
You asked us to do a main feature on inflammation, so here we go!
Before we start, it’s worth noting an important difference between acute and chronic inflammation:
- Acute inflammation is generally when the body detects some invader, and goes to war against it. This (except in cases such as allergic responses) is usually helpful.
- Chronic inflammation is generally when the body does a civil war. This is almost never helpful.
We’ll be tackling the latter, which frees up your body’s resources to do better at the former.
First, the obvious…
These five things are as important for this as they are for most things:
- Get a good diet—the Mediterranean diet is once again a top-scorer
- Exercise—move and stretch your body; don’t overdo it, but do what you reasonably can, or the inflammation will get worse.
- Reduce (or ideally eliminate) alcohol consumption. When in pain, it’s easy to turn to the bottle, and say “isn’t this one of red wine’s benefits?” (it isn’t, functionally*). Alcohol will cause your inflammation to flare up like little else.
- Don’t smoke—it’s bad for everything, and that goes for inflammation too.
- Get good sleep. Obviously this can be difficult with chronic pain, but do take your sleep seriously. For example, invest in a good mattress, nice bedding, a good bedtime routine, etc.
*Resveratrol (which is a polyphenol, by the way), famously found in red wine, does have anti-inflammatory properties. However, to get enough resveratrol to be of benefit would require drinking far more wine than will be good for your inflammation or, indeed, the rest of you. So if you’d like resveratrol benefits, consider taking it as a supplement. Superficially it doesn’t seem as much fun as drinking red wine, but we assure you that the results will be much more fun than the inflammation flare-up after drinking.
About the Mediterranean Diet for this…
There are many causes of chronic inflammation, but here are some studies done with some of the most common ones:
- Beneficial effect of Mediterranean diet in systemic lupus erythematosus patients
- How the Mediterranean diet and some of its components modulate inflammatory pathways in arthritis
- The effects of the Mediterranean diet on biomarkers of vascular wall inflammation and plaque vulnerability in subjects with high risk for cardiovascular disease
- Adherence to Mediterranean diet and 10-year incidence of diabetes: correlations with inflammatory and oxidative stress biomarkers*
*Type 1 diabetes is a congenital autoimmune disorder, as the pancreas goes to war with itself. Type 2 diabetes is different, being a) acquired and b) primarily about insulin resistance, and/but this is related to chronic inflammation regardless. It is also possible to have T1D and go on to develop insulin resistance, and that’s very bad, and/but beyond the scope of today’s newsletter, in which we are focusing on the inflammation aspects.
Some specific foods to eat or avoid…
Eat these:
- Leafy greens
- Cruciferous vegetables
- Tomatoes
- Fruits in general (berries in particular)
- Healthy fats, e.g. olives and olive oil
- Almonds and other nuts
- Dark chocolate (choose high cocoa, low sugar)
Avoid these:
- Processed meats (absolute worst offenders are hot dogs, followed by sausages in general)
- Red meats
- Sugar (includes most fruit juices, but not most actual fruits—the difference with actual fruits is they still contain plenty of fiber, and in many cases, antioxidants/polyphenols that reduce inflammation)
- Dairy products (unless fermented, in which case it seems to be at worst neutral, sometimes even a benefit, in moderation)
- White flour (and white flour products, e.g. white bread, white pasta, etc)
- Processed vegetable oils
See also: 9 Best Drinks To Reduce Inflammation, Says Science
Supplements?
Some supplements that have been found to reduce inflammation include:
(links are to studies showing their efficacy)
Consider Intermittent Fasting
Remember when we talked about the difference between acute and chronic inflammation? It’s fair to wonder “if I reduce my inflammatory response, will I be weakening my immune system?”, and the answer is: generally, no.
Often, as with the above supplements and dietary considerations, reducing inflammation actually results in a better immune response when it’s actually needed! This is because your immune system works better when it hasn’t been working in overdrive constantly.
Here’s another good example: intermittent fasting reduces the number of circulating monocytes (a way of measuring inflammation) in healthy humans—but doesn‘t compromise antimicrobial (e.g. against bacteria and viruses) immune response.
See for yourself: Dietary Intake Regulates the Circulating Inflammatory Monocyte Pool ← the study is about the anti-inflammatory effects of fasting
Share This Post
Related Posts
-
80-Year-Olds Share Their Biggest Regrets
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Notwithstanding the title, some of these people are a little younger than 80, but this adds to the interest a little as we see the different regrets / learned wisdoms at different stages of later life!
If we could turn back the time…
There are dozens of life regrets / wishes / retroactive advices shared in this video; here are some highlights:
- “My regret was I had a dysfunctional family and I wish I would have learned not to take responsibility.”
- “In my 30s, when I started drinking very heavily, I wish I hadn’t done that because it escalated to drug abuse.”
- “When my parents were old ages, I was working very hard… I didn’t have time to take care of them, not even spend the time with them. That’s my biggest regret.”
- “Live life to the fullest because none of us have any assurance on how old we’re going to be when we’re going to die.”
- “If I could do it over, I would have called home more and realized what my brother was going through.”
- “Spent a lot of years being concerned about what other people thought of me.”
- “You got to be careful what you say to your children because it means a lot.”
For the rest, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Managing Your Mortality Without Regrets
- How To Avoid Carer Burnout (Without Dropping Care)
- Managing Sibling Relationships In Adult Life
- Family Estrangment & How To Fix It
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What you need to know about H5N1 bird flu
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
On May 30, the Centers for Disease Control and Prevention reported that a Michigan dairy worker tested positive for H5N1 bird flu. It was the fourth person to test positive for H5N1 in the United States, following another recent case in Michigan, an April case in Texas, and an initial case in Colorado in 2022.
H5N1 bird flu has been spreading among bird species in the U.S. since 2021, killing millions of wild birds and poultry. In late March 2024, H5N1 bird flu was found in cows for the first time, causing an outbreak in dairy cows across several states.
U.S. public health officials and researchers are particularly concerned about this outbreak because the virus has infected cows and other mammals and has spread from a cow to a human for the first time.
This bird flu strain has shown to not only make wild mammals, including marine mammals and bears, very sick but to also cause high rates of death among species, says Jane Sykes, professor of small animal medicine at the University of California, Davis, School of Veterinary Medicine.
“And now that it has been found in cattle, [it] raises particular concern for spread to all the animal species, including people,” adds Sykes.
Even though the risk for human infection is low and there has never been human-to-human transmission of H5N1, there are several actions you can take to stay protected. Read on to learn more about H5N1 bird flu and the current outbreak.
What is H5N1?
H5N1 is a type of influenza virus that most commonly affects birds, causing them severe respiratory illness and death.
The H5N1 strain first emerged in China in the 1990s, and it has continued to spread around the world since then. In 1997, the virus spread from animals to humans in Hong Kong for the first time, infecting 18 people, six of whom died.
Since 2020, the H5N1 strain has caused “an unprecedented number of deaths in wild birds and poultry in many countries,” according to the World Health Organization.
Even though bird flu is rare in humans, an H5N1 infection can cause mild to severe illness and can be fatal in some cases. It can cause eye infection, upper respiratory symptoms, and pneumonia.
What do we know about the 2024 human cases of H5N1 in the U.S.?
The Michigan worker who tested positive for H5N1 in late May is a dairy worker who was exposed to infected livestock. They were the first to experience respiratory symptoms—including a cough without a fever—during the current outbreak. They were given an antiviral and the CDC says their symptoms are resolving.
The Michigan farm worker who tested positive earlier in May only experienced eye-related symptoms and has already recovered. And the dairy worker who tested positive for the virus in Texas in April only experienced eye redness as well, was treated with an antiviral medication for the flu, and is recovering.
Is H5N1 bird flu in the milk we consume?
The Food and Drug Administration has found traces of H5N1 bird flu virus in raw or unpasteurized milk. However, pasteurized milk is safe to drink.
Pasteurization, the process of heating milk to high temperatures to kill harmful bacteria (which the majority of commercially sold milk goes through), deactivates the virus. In 20 percent of pasteurized milk samples, the FDA found small, inactive (not live nor infectious) traces of the virus, but these fragments do not make pasteurized milk dangerous.
In a recent Infectious Diseases Society of America briefing, Dr. Maximo Brito, a professor at the University of Illinois College of Medicine, said that it’s important for people to avoid “drinking unpasteurized or raw milk [because] there are other diseases, not only influenza, that could be transmitted by drinking unpasteurized milk.”
What can I do to prevent bird flu?
While the risk of H5N1 infection in humans is low, people with exposure to infected animals (like farmworkers) are most at risk. But there are several actions you can take to stay protected.
One of the most important things, according to Sykes, is taking the usual precautions we’ve taken with COVID-19 and other respiratory viruses, including frequent handwashing, especially before eating.
“Handwashing and mask-wearing [are important], just as we learned from the pandemic,” Sykes adds. “And it’s not wearing a mask at all times, but thinking about high-risk situations, like when you’re indoors in a crowded environment, where transmission of respiratory viruses is much more likely to occur.”
There are other steps you can take to prevent H5N1, according to the CDC:
- Avoid direct contact with sick or dead animals, including wild birds and poultry.
- Don’t touch surfaces that may have been contaminated with animal poop, saliva, or mucus.
- Cook poultry and eggs to an internal temperature of 165 degrees Fahrenheit to kill any bacteria or virus, including H5N1. Generally, avoid eating undercooked food.
- Avoid consuming unpasteurized or raw milk or products like cheeses made with raw milk.
- Avoid eating uncooked or undercooked food.
- Poultry and livestock farmers and workers and bird flock owners should wear masks and other personal protective equipment “when in direct or close physical contact with sick birds, livestock, or other animals; carcasses; feces; litter; raw milk; or surfaces and water that might be contaminated with animal excretions from potentially or confirmed infected birds, livestock, or other animals.” (The CDC has more recommendations for this population here.)
Is there a vaccine for H5N1?
The CDC said there are two candidate H5N1 vaccines ready to be made and distributed in case the virus starts to spread from person to person, and the country is now moving forward with plans to produce millions of vaccine doses.
The FDA has approved several bird flu vaccines since 2007. The U.S. has flu vaccines in stockpile through the National Pre-Pandemic Influenza Vaccine Stockpile program, which allows for quick response as strains of the flu virus evolve.
Could this outbreak become a pandemic?
Scientists and researchers are concerned about the possibility of H5N1 spreading among people and causing a pandemic. “Right now, the risk is low, but as time goes on, the potential for mutation to cause widespread human infection increases,” says Sykes.
“I think this virus jumping into cows has shown the urgency to keep tracking [H5N1] a lot more closely now,” Peter Halfmann, research associate professor at the University of Wisconsin-Madison’s Influenza Research Institute tells PGN. “We have our eyes on surveillance now. … We’re keeping a much closer eye, so it’s not going to take us by surprise.”
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Body: A Guide for Occupants – by Bill Bryson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Better known for his writings on geography and history, here Bryson puts his mind to anatomy and physiology. How well does he do?
Very well, actually—thanks no doubt to the oversight of the veritable flock of consulting scientists mentioned in the acknowledgements. To this reviewer’s knowledge, no mistakes made it through into publication.
That said, Bryson’s love of history does shine through, and in this case, the book is as much a telling of medical history, as it is of the human body. That’s a feature not a bug, though, as not only is it fascinating in and of itself, but also, it’d be difficult to fully understand where we’re at in science, without understanding how we got here.
The style of the book is easy-reading narrative prose, but packed with lots of quirky facts, captivating anecdotes, and thought-provoking statistics. For example:
- The least effective way to spread germs is kissing. It proved ineffective among volunteers (in what sounds like a fun study) who had been successfully infected with the cold virus. Sneezes and coughs weren’t much better. The only really reliable way to transfer cold germs was physically by touch.
- The United States has 4% of the world’s population but consumes 80% of its opiates.
- Allowing a fever to run its course (within limits) could be the wisest thing. An increase of only a degree or so in body temperature slows the replication rate of viruses by a factor of 200.
Still, these kinds of things are woven together so well, that it doesn’t feel at all like reading a trivia list!
Bottom line: if you’d like to know a lot more about anatomy and physiology, but prefer a very casual style rather than sitting down with a stack of textbooks, this book is a great option.
Click here to check out The Body, and learn more about yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: