The Vagina Bible – by Dr. Jen Gunter
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The vagina is mysterious to most men, and honestly, also to a lot of women. School education on this is minimal, if even extant, and as an adult, everyone’s expected to “just know” stuff. However, here in reality, that isn’t how knowledge works.
To remedy this, gynecologist Dr. Jen Gunter takes 432 pages to give us the low-down and the ins-and-outs of this remarkable organ that affects, and is affected by, a lot of the rest of our health.
(On which note, if you think you already know it, ask yourself: could you write 432 pages about it? If not, you’ll probably still learn some things from this book)
Stylistically, this book is more of a textbook in presentation, but the writing is still very much easy-reading. The focus is mostly on anatomy and physiology, though she does give due attention to relevant healthcare options; what’s good, what’s bad, and what’s just plain unnecessary. In such cases, she always has plenty of science to hand; it’s never just “one woman’s opinion”.
If the book has a downside, it’s that (based on other reviews) it seems to upset some readers with unwelcome truths, but that’s more in the vein of “she’s right, of course, but I didn’t like reading it”.
Bottom line: if you have a vagina, or spend any amount of time in close proximity to one, then this is a great book for you.
Click here to check out The Vagina Bible, and upgrade your knowledge!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
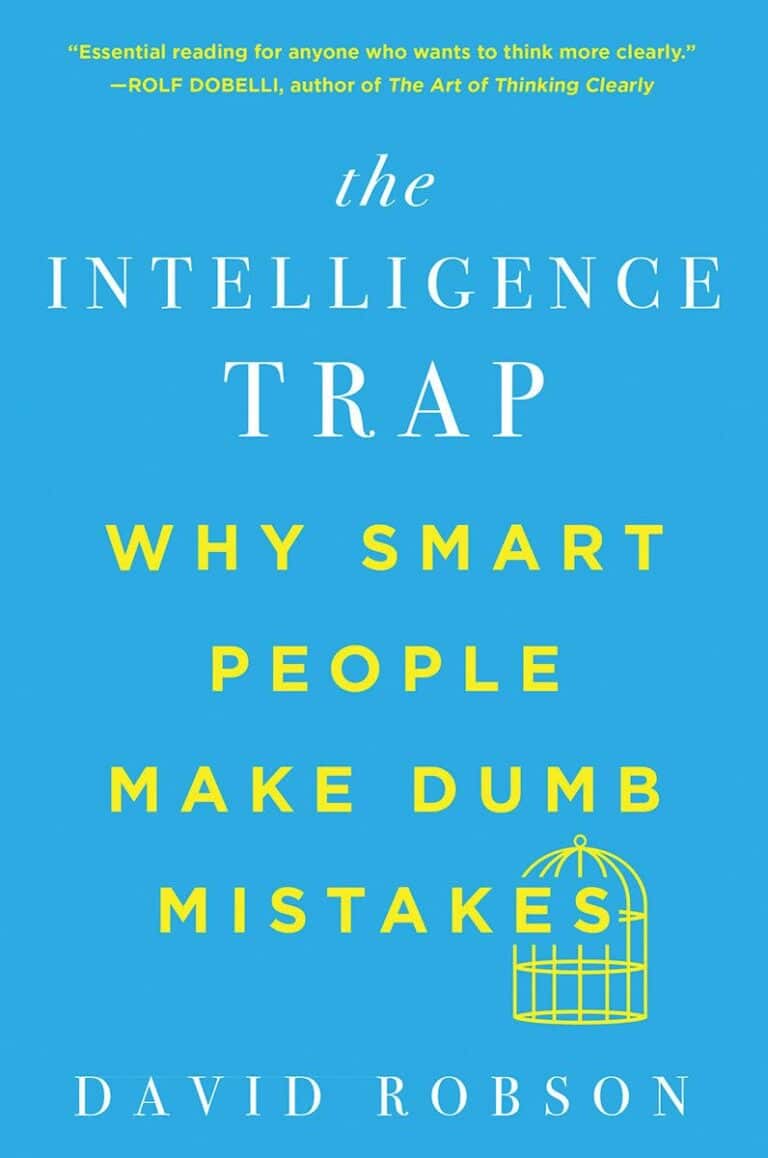
Managing Major Chronic Diseases – by Alexis Dupree
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our author, Alexis Dupree, is herself in her 70s, and writing with more than three decades of experience of surviving multiple chronic diseases (in her case, Multiple Sclerosis, and then a dozen comorbidities that came with such).
She is not a doctor or a scientist, but for more than 30 years she’s been actively working to accumulate knowledge not just on her own conditions, but on the whole medical system, and what it means to be a “forever patient” without giving up hope.
She talks lived-experience “life management” strategies for living with chronic disease, and she talks—again from lived experience—about navigating the complexities of medical care; not on a legalistic “State regulations say…” level, because that kind of thing changes by the minute, but on a human level.
Perhaps most practically: how to advocate strongly for yourself while still treating medical professionals with the respect and frankly compassion that they deserve while doing their best in turn.
But also: how to change your attitude to that of a survivor, and yet also redefine your dreams. How to make a new game plan of life—while working to make life easier for yourself. How to deal, psychologically, with the likelihood that not only will you probably not get better, but also, you will probably get worse, while still never, ever, giving up.
After all, many things are easily treatable today that mere decades ago were death sentences, and science is progressing all the time. We just have to stay alive, and in as good a condition as we reasonably can, to benefit from those advances!
Bottom line: if you have a chronic disease, or if a loved one does, then this is an immensely valuable book to read.
Click here to check out Managing Major Chronic Diseases, and make life easier!
Share This Post
-
‘Sleep tourism’ promises the trip of your dreams. Beyond the hype plus 5 tips for a holiday at home
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Imagine arriving at your hotel after a long flight and being greeted by your own personal sleep butler. They present you with a pillow menu and invite you to a sleep meditation session later that day.
You unpack in a room kitted with an AI-powered smart bed, blackout shades, blue light-blocking glasses and weighted blankets.
Holidays are traditionally for activities or sightseeing – eating Parisian pastry under the Eiffel tower, ice skating at New York City’s Rockefeller Centre, lying by the pool in Bali or sipping limoncello in Sicily. But “sleep tourism” offers vacations for the sole purpose of getting good sleep.
The emerging trend extends out of the global wellness tourism industry – reportedly worth more than US$800 billion globally (A$1.2 trillion) and expected to boom.
Luxurious sleep retreats and sleep suites at hotels are popping up all over the world for tourists to get some much-needed rest, relaxation and recovery. But do you really need to leave home for some shuteye?
RossHelen/Shutterstock Not getting enough
The rise of sleep tourism may be a sign of just how chronically sleep deprived we all are.
In Australia more than one-third of adults are not achieving the recommended 7–9 hours of sleep per night, and the estimated cost of this inadequate sleep is A$45 billion each year.
Inadequate sleep is linked to long-term health problems including poor mental health, heart disease, metabolic disease and deaths from any cause.
Can a fancy hotel give you a better sleep?
Many of the sleep services available in the sleep tourism industry aim to optimise the bedroom for sleep. This is a core component of sleep hygiene – a series of healthy sleep practices that facilitate good sleep including sleeping in a comfortable bedroom with a good mattress and pillow, sleeping in a quiet environment and relaxing before bed.
The more people follow sleep hygiene practices, the better their sleep quality and quantity.
When we are staying in a hotel we are also likely away from any stressors we encounter in everyday life (such as work pressure or caring responsibilities). And we’re away from potential nighttime disruptions to sleep we might experience at home (the construction work next door, restless pets, unsettled children). So regardless of the sleep features hotels offer, it is likely we will experience improved sleep when we are away.
Being away from home also means being away from domestic disruptions. Makistock/Shutterstock What the science says about catching up on sleep
In the short-term, we can catch up on sleep. This can happen, for example, after a short night of sleep when our brain accumulates “sleep pressure”. This term describes how strong the biological drive for sleep is. More sleep pressure makes it easier to sleep the next night and to sleep for longer.
But while a longer sleep the next night can relieve the sleep pressure, it does not reverse the effects of the short sleep on our brain and body. Every night’s sleep is important for our body to recover and for our brain to process the events of that day. Spending a holiday “catching up” on sleep could help you feel more rested, but it is not a substitute for prioritising regular healthy sleep at home.
All good things, including holidays, must come to an end. Unfortunately the perks of sleep tourism may end too.
Our bodies do not like variability in the time of day that we sleep. The most common example of this is called “social jet lag”, where weekday sleep (getting up early to get to work or school) is vastly different to weekend sleep (late nights and sleep ins). This can result in a sleepy, grouchy start to the week on Monday. Sleep tourism may be similar, if you do not come back home with the intention to prioritise sleep.
So we should be mindful that as well as sleeping well on holiday, it is important to optimise conditions at home to get consistent, adequate sleep every night.
Good sleep hygiene doesn’t require a passport. Maridav/Shutterstock 5 tips for having a sleep holiday at home
An AI-powered mattress and a sleep butler at home might be the dream. But these features are not the only way we can optimise our sleep environment and give ourselves the best chance to get a good night’s sleep. Here are five ideas to start the night right:
1. avoid bright artificial light in the evening (such as bright overhead lights, phones, laptops)
2. make your bed as comfortable as possible with fresh pillows and a supportive mattress
3. use black-out window coverings and maintain a cool room temperature for the ideal sleeping environment
4. establish an evening wind-down routine, such as a warm shower and reading a book before bed or even a “sleepy girl mocktail”
5. use consistency as the key to a good sleep routine. Aim for a similar bedtime and wake time – even on weekends.
Charlotte Gupta, Senior postdoctoral research fellow, Appleton Institute, HealthWise research group, CQUniversity Australia and Dean J. Miller, Adjunct Research Fellow, Appleton Institute of Behavioural Science, CQUniversity Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Using the”Task Zero” approach
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Jonathan Frakes Asks You Things” Voice:
- Do you ever find yourself in a room and wonder what you’re doing there?
- Or set about a to-do list, but get quickly distracted by side-quests?
- Finally get through to a person in a call center, they ask how they can help, and your mind goes blank?
- Go to the supermarket and come out with six things, none of which were the one you came for?
This is a “working memory” thing and you’re not alone. There’s a trick that can help keep you on track more often than not:
Don’t try to overburden your working memory. It is very limited (this goes for everyone to a greater or lesser degree). Instead, hold only two tasks at once:
- Task zero (what you are doing right now)
- Task one (your next task)
When you’ve completed task zero, task one becomes the new task zero, and you can populate a new task one from your to-do list.
This way, you will always know what you’re doing right now, and what you’re doing next, and your focus will be so intent on task zero, that you will not get sidetracked by task seventeen!
Happy focusing
Share This Post
Related Posts
-
What Does Kaempferol Do, Anyway?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝In the this or that article, you said kampeferol was a famously good flavonol on a par with quercetin, does it do the same thing or does it do something different, and is it worth supplementing?❞
So, this will be in reference to a This-or-That from last week:
Cantaloupe vs Cucumber – Which is Healthier?
Let’s break down your question into parts:
- Is it comparable to quercetin?
- Does it have special properties of its own?
- Is it worth supplementing?
Is it comparable to quercetin?
They are both flavonols, and potent ones at that. Similarities include that they’re found in many of the same plants, and that (like most if not all polyphenols) they have antioxidant and anti-inflammatory benefits, which in turn usually translate to anti-aging and anticancer benefits too.
You can read more about quercetin here: Fight Inflammation & Protect Your Brain, With Quercetin
You can read more about polyphenols in general here: 21 Most Beneficial Polyphenols & What Foods Have Them ← quercetin and kaempferol are #1 and #2 on this list, respectively
Does it have special properties of its own?
Yes it does!
❝Epidemiological studies have shown an inverse relationship between kaempferol intake and cancer.
Kaempferol may help by augmenting the body’s antioxidant defense against free radicals, which promote the development of cancer.
At the molecular level, kaempferol has been reported to modulate a number of key elements in cellular signal transduction pathways linked to apoptosis, angiogenesis, inflammation, and metastasis.
Significantly, kaempferol inhibits cancer cell growth and angiognesis and induces cancer cell apoptosis, but on the other hand, kaempferol appears to preserve normal cell viability, in some cases exerting a protective effect.❞
Read in full: A review of the dietary flavonoid, kaempferol on human health and cancer chemoprevention
It is also particularly good for the gut:
❝Most recently, an increasing number of studies have demonstrated the significance of kaempferol in the regulation of intestinal function and the mitigation of intestinal inflammation❞
Read in full: A Critical Review of Kaempferol in Intestinal Health and Diseases
This also means it is particularly efficacious against food allergies:
❝we screened food ingredients with the expectation of finding dietary compounds that exert beneficial effects on intestinal immune tolerance and identified kaempferol, a flavonoid, as the compound that most effectively increased Aldh1a2 mRNA levels❞
(that’s good)
That one’s a bit scientifically denser than we usually try to find when citing sources here, so here’s a pop-science article about the same thing, which explains in more words than we have room to here:
Flavonoid kaempferol could offer natural relief for food allergies ← much lighter reading, but still very informative
Kaempferol (like quercetin, granted) is also a potent neuroprotective agent, not least of all because its anti-inflammatory powers extend to reducing neuroinflammation (not everything does, because not everything we ingest can pass the blood-brain barrier to affect what goes on in the brain):
…and more:
❝it may be used to treat numerous acute and chronic inflammation-induced diseases, including intervertebral disc degeneration and colitis, as well as post-menopausal bone loss and acute lung injury. In addition, it has beneficial effects against cancer, liver injury, obesity and diabetes, inhibits vascular endothelial inflammation, protects the cranial nerve and heart function, and may be used for treating fibroproliferative disorders, including hypertrophic scar.❞
Read in full: Recent progress regarding kaempferol for the treatment of various diseases
Is it worth supplementing?
If you eat a lot of leafy greens, cruciferous vegetables, and/or citrus fruits, and/or drink tea (true teas from tea plants, not miscellaneous herbal infusions), then you probably get a good dose of kaempferol already.
However, if you want to supplement, hawthorn berry is not a bad one to go with, like this example product on Amazon 😎
We wrote about this before, here: Hawthorn For The Heart (& More)
As for teas, if you’re wondering about the merits of black, white, green or red, check out:
Black, White, Green, Red: Which Kind Of Tea Is Best For The Health, According To Science? ← this covers many factors
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cherries vs Blueberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cherries to blueberries, we picked the blueberries.
Why?
It was close! And blueberries only won by virtue of taking an average value for cherries; we could have (if you’ll pardon the phrase) cherry-picked tart cherries for extra benefits that’d put them ahead of blueberries. That’s how close it is.
In terms of macros, they are almost identical, so nothing to set them apart there.
In the category of vitamins, they are mostly comparable except that blueberries have a lot more vitamin K, and cherries have a lot more vitamin A. Since vitamin K is the vitamin that’s scarcer in general, we’ll call blueberries’ vitamin K content a win.
Blueberries do also have about 6x more vitamin E, with a cup of blueberries containing about 10% of the daily requirement (and cherries containing almost none). Another small win for blueberries.
When it comes to minerals, they are mostly comparable; the largest point of difference is that blueberries contain more manganese while cherries contain more copper; nothing to decide between them here.
We’re down to counting amino acids and antioxidants now, so blueberries have a lot more cystine and tyrosine. They also have slightly more of amino acids that they both only have trace amounts of. And as for antioxidants? Blueberries contain notably more quercetin.
So, blueberries win the day—but if we had specified tart cherries rather than taking an average, they could have come out on top. Enjoy both!
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ozempic Helps People Walk Further
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s often a catch-22 when it comes to exercise: it’s important for good health, and/but people with ill health usually cannot exercise much.
A recent (published today, at time of writing, the 29th of March 2025, never let it be said we don’t bring you the very most up-to-date health science!) study by Dr. Neda Rasouli et al. has shown there is a possible way through that catch-22, depending on the nature of the illness.
This study followed 792 people across 112 outpatient clinical trial sites in 20 countries in North America, Asia, and Europe, with type 2 diabetes and peripheral artery disease.
What they found
Patients taking semaglutide (specifically, 1mg Ozempic) enjoyed a 21% median increase in walking distance, as well as some bonus benefits, namely:
- Weight reduction: the semaglutide group saw a greater reduction in body weight (–4.1 kg; P < 0 .0001)
- HbA1c levels: semaglutide lowered HbA1c by 1 percentage point (P < 0.0001)
- Blood pressure: systolic blood pressure decreased by 3.2 mmHg (P = 0.0042)
You may be wondering what that “P =” means: it’s the probability of this occurring by random chance, on a scale from zero (impossible outcome) to 1 (unavoidable outcome).
For example:
“We hypothesized that singing the happy birthday song before tossing a coin would result in it landing on heads. We sang the happy birthday song and tossed the coin; it landed on heads (P = 0.5)”
In science, generally speaking anything with a probability of under 0.05 (expressed as: “P < 0.05”) is considered a statistically significant result.
All this to say, the cited figures of, for example, P < 0.0001, are very significant indeed.
On which note, that 21% median increase in walking distance? P < 0.0004.
As for side effects? Serious adverse events related to the drug occurred in 1% of the semaglutide group vs 2% in the placebo group. So, that seems quite safe indeed.
You can find the paper itself here:
Want to learn more?
Check out:
- The Doctor Who Wants Us To Exercise Less, & Move More
- Walking… Better.
- 5 Ways To Naturally Boost The “Ozempic Effect”
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: