The Intelligence Trap – by David Robson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’re including this one under the umbrella of “general wellness”, because it happens that a lot of very intelligent people make stunningly unfortunate choices sometimes, for reasons that may baffle others.
The author outlines for us the various reasons that this happens, and how. From the famous trope of “specialized intelligence in one area”, to the tendency of people who are better at acquiring knowledge and understanding to also be better at acquiring biases along the way, to the hubris of “I am intelligent and therefore right as a matter of principle” thinking, and many other reasons.
Perhaps the greatest value of the book is the focus on how we can avoid these traps, narrow our bias blind spots, and play to our strengths while paying full attention to our weaknesses.
The style is very readable, despite having a lot of complex ideas discussed along the way. This is entirely to be expected of this author, an award-winning science writer.
Bottom line: if you’d like to better understand the array of traps that disproportionately catch out the most intelligent people (and how to spot such), then this is a great book for you.
Click here to check out The Intelligence Trap, and be more wary!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The 6 Dimensions Of Sleep (And Why They Matter)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Good Is Your Sleep, Really?
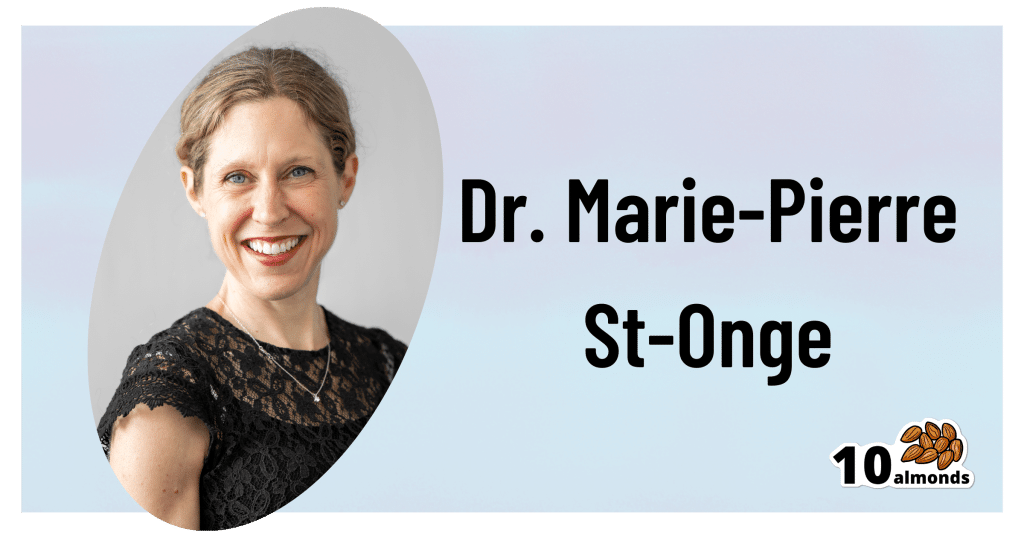
This is Dr. Marie-Pierre St-Onge, Director of Columbia University’s Center of Excellence for Sleep and Circadian Research.
The focus of Dr. St-Onge’s research is the study of the impact of lifestyle, especially sleep and diet, on cardio-metabolic risk factors.
She conducts clinical research combining her expertise on sleep, nutrition, and energy regulation.
What kind of things do her studies look at?
Her work focuses on questions about…
- The role of circadian rhythms (including sleep duration and timing)
- Meal timing and eating patterns
…and their impact on cardio-metabolic risk.
What does she want us to know?
First things first, when not to worry:
❝Getting a bad night’s sleep once in a while isn’t anything to worry about. That’s what we would describe as transient insomnia. Chronic insomnia occurs when you spend three months or more without regular sleep, and that is when I would start to be concerned.❞
But… as prevention is (as ever) better than cure, she also advises that we do pay attention to our sleep! And, as for how to do that…
The Six Dimensions of Sleep
One useful definition of overall sleep health is the RU-Sated framework, which assesses six key dimensions of sleep that have been consistently associated with better health outcomes. These are:
- regularity
- satisfaction with sleep
- alertness during waking hours
- timing of sleep
- efficiency of sleep
- duration of sleep
You’ll notice that some of these things you can only really know if you use a sleep-monitoring app. She does recommend the use of those, and so do we!
We reviewed and compared some of the most popular sleep-monitoring apps! You can check them out here: Time For Some Pillow Talk
You also might like…
We’re not all the same with regard to when is the best time for us to sleep, so:
Use This Sleep Cycle Calculator To Figure Out the Optimal Time for You To Go to Bed and Wake Up
AROUND THE WEB
What’s happening in the health world…
- Aspirin may make your breathing worse
- Taking naps for more than 30 minutes may raise your metabolic disease risk
- How to ease back into exercise after surgery
- Study provides evidence that breathing exercises may reduce your Alzheimer’s risk
- No one in movies knows how to swallow a pill
More to come tomorrow!
Share This Post
-
How Not To Get Sick: A Cookbook – by Dr. Benjamin Bikman and Diana Keuilian
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Bikman’s excellent “Why We Get Sick”, and if you haven’t read that yet, we recommend doing so.
Nevertheless, you don’t need to have read it to benefit from this one, which is about cooking with those learnings (from the other book) in mind.
Before getting to the recipes, we get a section recapping what we learned previously, as well as adding some more general lifestyle advices beyond the kitchen. The science is also expanded a bit, to include such things as the two-way relationship between insulin and aging, as well as the interplay with other metrics of health, including blood lipids, for example.
The authors then provide a plan, in the three stages: reverse (insulin resistance), prevent (insulin resistance), maintain (insulin sensitivity).
The recipes themselves, of which there are 70, are of course tailored to do the above three things; they’re also quite diverse, albeit if you are vegetarian or vegan, you should know in advance that most of these recipes are not.
Bottom line: if the above doesn’t apply to you, and you would like to improve your insulin sensitivity, this book can indeed help.
Share This Post
-
If I’m diagnosed with one cancer, am I likely to get another?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Receiving a cancer diagnosis is life-changing and can cause a range of concerns about ongoing health.
Fear of cancer returning is one of the top health concerns. And managing this fear is an important part of cancer treatment.
But how likely is it to get cancer for a second time?
Why can cancer return?
While initial cancer treatment may seem successful, sometimes a few cancer cells remain dormant. Over time, these cancer cells can grow again and may start to cause symptoms.
This is known as cancer recurrence: when a cancer returns after a period of remission. This period could be days, months or even years. The new cancer is the same type as the original cancer, but can sometimes grow in a new location through a process called metastasis.
Actor Hugh Jackman has gone public about his multiple diagnoses of basal cell carcinoma (a type of skin cancer) over the past decade.
The exact reason why cancer returns differs depending on the cancer type and the treatment received. Research is ongoing to identify genes associated with cancers returning. This may eventually allow doctors to tailor treatments for high-risk people.
What are the chances of cancer returning?
The risk of cancer returning differs between cancers, and between sub-types of the same cancer.
New screening and treatment options have seen reductions in recurrence rates for many types of cancer. For example, between 2004 and 2019, the risk of colon cancer recurring dropped by 31-68%. It is important to remember that only someone’s treatment team can assess an individual’s personal risk of cancer returning.
For most types of cancer, the highest risk of cancer returning is within the first three years after entering remission. This is because any leftover cancer cells not killed by treatment are likely to start growing again sooner rather than later. Three years after entering remission, recurrence rates for most cancers decrease, meaning that every day that passes lowers the risk of the cancer returning.
Every day that passes also increases the numbers of new discoveries, and cancer drugs being developed.
What about second, unrelated cancers?
Earlier this year, we learned Sarah Ferguson, Duchess of York, had been diagnosed with malignant melanoma (a type of skin cancer) shortly after being treated for breast cancer.
Although details have not been confirmed, this is likely a new cancer that isn’t a recurrence or metastasis of the first one.
Australian research from Queensland and Tasmania shows adults who have had cancer have around a 6-36% higher risk of developing a second primary cancer compared to the risk of cancer in the general population.
Who’s at risk of another, unrelated cancer?
With improvements in cancer diagnosis and treatment, people diagnosed with cancer are living longer than ever. This means they need to consider their long-term health, including their risk of developing another unrelated cancer.
Reasons for such cancers include different types of cancers sharing the same kind of lifestyle, environmental and genetic risk factors.
The increased risk is also likely partly due to the effects that some cancer treatments and imaging procedures have on the body. However, this increased risk is relatively small when compared with the (sometimes lifesaving) benefits of these treatment and procedures.
While a 6-36% greater chance of getting a second, unrelated cancer may seem large, only around 10-12% of participants developed a second cancer in the Australian studies we mentioned. Both had a median follow-up time of around five years.
Similarly, in a large US study only about one in 12 adult cancer patients developed a second type of cancer in the follow-up period (an average of seven years).
The kind of first cancer you had also affects your risk of a second, unrelated cancer, as well as the type of second cancer you are at risk of. For example, in the two Australian studies we mentioned, the risk of a second cancer was greater for people with an initial diagnosis of head and neck cancer, or a haematological (blood) cancer.
People diagnosed with cancer as a child, adolescent or young adult also have a greater risk of a second, unrelated cancer.
What can I do to lower my risk?
Regular follow-up examinations can give peace of mind, and ensure any subsequent cancer is caught early, when there’s the best chance of successful treatment.
Maintenance therapy may be used to reduce the risk of some types of cancer returning. However, despite ongoing research, there are no specific treatments against cancer recurrence or developing a second, unrelated cancer.
But there are things you can do to help lower your general risk of cancer – not smoking, being physically active, eating well, maintaining a healthy body weight, limiting alcohol intake and being sun safe. These all reduce the chance of cancer returning and getting a second cancer.
Sarah Diepstraten, Senior Research Officer, Blood Cells and Blood Cancer Division, Walter and Eliza Hall Institute and Terry Boyle, Senior Lecturer in Cancer Epidemiology, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Blackberries vs Blueberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing blackberries to blueberries, we picked the blackberries.
Why?
They’re both great! But the humble blackberry stands out (and is an example of “foods that are darker are often more nutrient-dense”).
In terms of macronutrients, they’re quite similar, being both berry fruits that are mostly water, but blackberries do have 2x the fiber (and for what it’s worth, 2x the protein, though this is a small number obviously), while blueberries have 2x the carbohydrates. An easy win for blackberries.
When it comes to vitamins, blackberries have notably more of vitamin A, B3, B5, B9, C, and E, as well as choline, while blueberries have a little more of vitamins B1, B2, and B6. A fair win for blackberries.
In the category of minerals, blackberries have a lot more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. Blueberries are not higher in any minerals. Another easy win for blackberries.
Blueberries are famous for their antioxidants, but blackberries actually equal them. The polyphenolic content varies from one fruit to another, but they are both loaded with an abundance (thousands) of antioxidants, especially anthocyanins. Blackberries and blueberries tie in this category.
Adding up the sections makes for an easy, easy win for blackberries—but diversity is always best, so enjoy both!
Want to learn more?
You might like to read:
- Cherries vs Blueberries – Which is Healthier?
- Strawberries vs Cherries – Which is Healthier?
- Strawberries vs Raspberries – Which is Healthier?
- Goji Berries vs Blueberries – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Breadfruit vs Custard Apple – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing breadfruit to custard apple, we picked the breadfruit.
Why?
Today in “fruits pretending to be less healthy things than they are”, both are great, but one of these fruits just edges out the other in all categories. This is quite simple today:
In terms of macros, being fruits they’re both fairly high in carbs and fiber, however the carbs are close to equal and breadfruit has nearly 2x the fiber.
This also means that breadfruit has the lower glycemic index, but they’re both medium-low GI foods with a low insulin index.
When it comes to vitamins, breadfruit has more of vitamins B1, B3, B5, and C, while custard apple has more of vitamins A, B2, and B6. So, a 4:3 win for breadfruit.
In the category of minerals, breadfruit has more copper, magnesium, phosphorus, potassium, and zinc, while custard apple has more calcium and iron.
In short, enjoy both, but if you’re going just for one, breadfruit is the healthiest.
Want to learn more?
You might like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Figs vs Banana – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing figs to banana, we picked the banana.
Why?
Both of these fruits have a reputation for being carb-heavy (though their glycemic index is low in both cases because of the fiber), and they both have approximately the same macros across the board. So a tie on macros.
When it comes to vitamins, figs have more of vitamins A, B1, E, and K, while banana has more of vitamins B2, B3, B5, B6, B9, C, and choline. So, a win for banana there.
In the category of minerals, figs have more calcium and iron, while banana has more copper, magnesium, manganese, phosphorus, potassium, and selenium. Another win for banana.
Adding up the section makes for a win for bananas, but by all means, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: