The Two-Second Advantage – by Vivek Ranadive and Kevin Maney
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The titular “two-second advantage” can in some cases be literal (imagine you got a two-second head-start in a boxing match!), in other cases can refer to being just a little ahead of things in a way that can confer a great advantage, often cumulatively—as anyone who’s played Monopoly can certainly attest.
Vivek Ranadivé and Kevin Maney give us lots of examples from business, sports, politics, economics, and more, in a way that seeks to cultivate a habit of asking the right questions in order to anticipate the future and not just be ahead of the competition—some areas of life don’t have competition for most people, like health, for example—but to generally have things “in hand”.
When it comes to personal finances, health, personal projects, and the like, those tiny initial advantages that lead to incremental further improvements, can be the difference between continually (and frantically) playing catch-up, or making the jump past breaking even to going from strength to strength.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Squat Variations for Painful Knees (No More Pain!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Having bad knees can be a bit of a catch-22; you want to squat to make them stronger, but you can’t do that because your knees are not good. But, there are ways to do it!
Dr. Alyssa Kuhn, a doctor of physical therapy, advises:
Gently does it
Ten ways to choose from:
- Pool Squats: performed in a pool for joint-friendly support. Can use both hands, one hand, or no support. Focus on sitting back and standing up, aiming for 10–20 reps.
- Supported Squats: use a sink, rings, or handles for support. Stand a distance away and sit back while keeping your knees behind your heels. Perform 10–20 reps for 2–3 sets.
- Chair Loop Squats: use a resistance band around your knees while sitting on a chair. Press your knees outward as you stand and sit to strengthen hip and knee stability. Do 8–12 reps for 2–3 sets.
- Heel Elevated Squats: place your heels on dumbbells to shift emphasis to thighs and reduce knee strain. Ideal for stiff ankles or back tightness. Perform 10–15 reps for 2–3 sets.
- Sumo Squats: a wide stance squat, good for hip strength and reducing knee stress. Adjust your foot positioning for comfort. Perform 15–20 reps for 2–3 sets.
- Chair Squats: hold a weight close to your chest while sitting and standing from a chair. Can use kettlebells or dumbbells. Do 8–10 reps for 2–3 sets.
- Band Squats: use a resistance band secured behind your knees to provide support and encourage proper squat mechanics. Perform 5–12 reps for 2–3 sets.
- Modified Single Leg Squat: sit-to-stand using one leg with the other as a kickstand. Adjust your foot position for difficulty. Perform 8–12 reps per side for 2–3 sets.
- Weighted Squats: add weight using dumbbells or a barbell. Maintain an upright torso. Adjust the weight and reps based on difficulty, and do 5–10 reps for 2–4 sets.
- Split Squat: a stationary lunge, keeping your feet in place and lowering straight down. Focus on your front leg while keeping balance. Can add weight if you want. Perform 5–12 reps per side based on difficulty.
For more on each of these plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
Seeds: The Good, The Bad, And The Not-Really-Seeds!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Doctors are great at saving lives like mine. I’m a two time survivor of colon cancer and have recently been diagnosed with Chron’s disease at 62. No one is the health system can or is prepared to tell me an appropriate diet to follow or what to avoid. Can you?❞
Congratulations on the survivorship!
As to Crohn’s, that’s indeed quite a pain, isn’t it? In some ways, a good diet for Crohn’s is the same as a good diet for most other people, with one major exception: fiber
…and unfortunately, that changes everything, in terms of a whole-foods majority plant-based diet.
What stays the same:
- You still ideally want to eat a lot of plants
- You definitely want to avoid meat and dairy in general
- Eating fish is still usually* fine, same with eggs
- Get plenty of water
What needs to change:
- Consider swapping grains for potatoes or pasta (at least: avoid grains)
- Peel vegetables that are peelable; discard the peel or use it to make stock
- Consider steaming fruit and veg for easier digestion
- Skip spicy foods (moderate spices, like ginger, turmeric, and black pepper, are usually fine in moderation)
Much of this latter list is opposite to the advice for people without Crohn’s Disease.
*A good practice, by the way, is to keep a food journal. There are apps that you can get for free, or you can do it the old-fashioned way on paper if prefer.
But the important part is: make a note not just of what you ate, but also of how you felt afterwards. That way, you can start to get a picture of patterns, and what’s working (or not) for you, and build up a more personalized set of guidelines than anyone else could give to you.
We hope the above pointers at least help you get going on the right foot, though!
❝Why do baked goods and deep fried foods all of a sudden become intolerable? I used to b able to ingest bakery foods and fried foods. Lately I developed an extreme allergy to Kiwi… what else should I “fear”❞
About the baked goods and the deep-fried foods, it’s hard to say without more information! It could be something in the ingredients or the method, and the intolerance could be any number of symptoms that we don’t know. Certainly, pastries and deep-fried foods are not generally substantial parts of a healthy diet, of course!
Kiwi, on the other hand, we can answer… Or rather, we can direct you to today’s “What’s happening in the health world” section below, as there is news on that front!
We turn the tables and ask you a question!
We’ll then talk about this tomorrow:
Share This Post
-
The Exercises That Can Fix Sinus Problems (And More)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Who nose what benefits you will gain today?
This is James Nestor, a science journalist and author. He’s written for many publications, including Scientific American, and written a number of books, most notably Breath: The New Science Of A Lost Art.
Today we’ll be looking at what he has to share about what has gone wrong with our breathing, what problems this causes, and how to fix it.
What has gone wrong?
When it comes to breathing, we humans are the pugs of the primate world. In a way, we have the opposite problem to the squashed-faced dogs, though. But, how and why?
When our ancestors learned first tenderize food, and later to cook it, this had two big effects:
- We could now get much more nutrition for much less hunting/gathering
- We now did not need to chew our food nearly so much
Getting much more nutrition for much less hunting/gathering is what allowed us to grow our brains so large—as a species, we have a singularly large brain-to-body size ratio.
Not needing to chew our food nearly so much, meanwhile, had even more effects… And these effects have become only more pronounced in recent decades with the rise of processed food making our food softer and softer.
It changed the shape of our jaw and cheekbones, just as the size of our brains taking up more space in our skull moved our breathing apparatus around. As a result, our nasal cavities are anatomically ridiculous, our sinuses are a crime against nature (not least of all because they drain backwards and get easily clogged), and our windpipes are very easily blocked and damaged due to the unique placement of our larynx; we’re the only species that has it there. It allowed us to develop speech, but at the cost of choking much more easily.
What problems does this cause?
Our (normal, to us) species-wide breathing problems have resulted in behavioral adaptations such as partial (or in some people’s cases, total or near-total) mouth-breathing. This in turn exacerbates the problems with our jaws and cheekbones, which in turn exacerbates the problems with our sinuses and nasal cavities in general.
Results include such very human-centric conditions as sleep apnea, as well as a tendency towards asthma, allergies, and autoimmune diseases. Improper breathing also brings about a rather sluggish metabolism for how many calories we consume.
How are we supposed to fix all that?!
First, close your mouth if you haven’t already, and breathe through your nose.
In and out.
Both are important, and unless you are engaging in peak exercise, both should be through your nose. If you’re not used to this, it may feel odd at first, but practice, and build up your breathing ability.
Six seconds in and six seconds out is a very good pace.
If you’re sitting doing a breathing exercise, also good is four seconds in, four seconds hold, four seconds out, four seconds hold, repeat.
But those frequent holds aren’t practical in general life, so: six seconds in, six seconds out.
Through your nose only.
This has benefits immediately, but there are other more long-term benefits from doing not just that, but also what has been called (by Nestor, amongst many others), “Mewing”, per the orthodontist, Dr. John Mew, who pioneered it.
How (and why) to “mew”:
Place your tongue against the roof of your mouth. It should be flat against the palate; you’re not touching it with the tip here; you’re creating a flat seal.
Note: if you were mouth-breathing, you will now be unable to breathe. So, important to make sure you can breathe adequately through your nose first.
This does two things:
- It obliges nose-breathing rather than mouth-breathing
- It creates a change in how the muscles of your face interact with the bones of your face
In a battle between muscle and bone, muscle will always win.
Aim to keep your tongue there as much as possible; make it your new best habit. If you’re not eating, talking, or otherwise using your tongue to do something, it should be flat against the roof of your mouth.
You don’t have to exert pressure; this isn’t an exercise regime. Think of it more as a postural exercise, just, inside your mouth.
Quick note: read the above line again, because it’s important. Doing it too hard could cause the opposite problems, and you don’t want that. You cannot rush this by doing it harder; it takes time and gentleness.
Why would we want to do that?
The result, over time, will tend to be much healthier breathing, better sinus health, freer airways, reduced or eliminated sleep apnea, and, as a bonus, what is generally considered a more attractive face in terms of bone structure. We’re talking more defined cheekbones, straighter teeth, and a better mouth position.
Want to learn more?
This is the “Mewing” technique that Nestor encourages us to try:
Share This Post
Related Posts
-
Basic Baked Tofu
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the main criticisms of tofu is that it is tasteless. Well, so is flour, but you’re not supposed to eat it plain, and the same goes for tofu. It’s a blank canvas that you get to decide what to do with—not to mention, it’s a canvas that’s very high in protein, and is a complete protein too, containing all essential amino acids. Anyway, here’s a starter recipe that elevates tofu from “nutrition” to “nutritious tasty snack”!
We were going to do a fancier recipe today, but considered that it might be judicious to cover this basic element first, that can be incorporated into a larger recipe later, a bit like we have done with recipes such as our Tasty Versatile Rice, and Plant-Based Healthy Cream Cheese (amongst others).
You will need
- 1 block of extra-firm tofu; these are quite standardized in size; it should be about 12oz; don’t worry if it’s a little more or less.
- 2 tbsp arrowroot powder (or potato starch if you don’t have arrowroot)
- 1½ tbsp extra virgin olive oil
- 1 tbsp nutritional yeast
- 1 tsp black pepper
- ½ tsp MSG or 1 tsp low-sodium salt
- Optional: ½ tsp garlic powder
- Optional: ½ tsp ground turmeric
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 425ºF / 220ºC.
2) Press the tofu for about 15 minutes (to remove excess moisture), using a tofu press if you have one. If you don’t, then here is an example product on Amazon, or alternatively, you can go with the time-honored tradition of cutting the tofu lengthways into slabs, and wrapping it in a lint-free kitchen towel or muslin cloth, and pressing it with heavy books. We don’t recommend pressing for more than about 15 minutes, as you are going to bake the tofu so you don’t want it too dry going in.
3) Cut the tofu into cubes. Size is up to you, but half-inch cubes are very respectable.
4) Combine the tofu cubes in a big bowl with the oil and seasonings, including the nutritional yeast but not the arrowroot powder or potato starch yet. You will need to toss them gently (very gently; they are fragile!) to combine.
5) Add the arrowroot powder or potato starch, and again toss gently to combine. We do this last, because it would stop the other things from sticking properly if we did it earlier.
6) Arrange the tofu on a baking tray lined with baking paper, in a single layer so that the cubes don’t touch. Bake for 15 minutes, turn them over, and bake for a further 15 minutes on the other side. They should now be golden and crisp, but if they’re not, just give them a little more time.
7) Serve as a snack, or set aside for whatever else you’re going to do with them in a larger more complex recipe.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Tofu vs Seitan – Which is Healthier?
- Plant vs Animal Protein: Head to Head
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
We looked at 700 plant-based foods to see how healthy they really are. Here’s what we found
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’re thinking about buying plant-based foods, a trip to the supermarket can leave you bewildered.
There are plant-based burgers, sausages and mince. The fridges are loaded with non-dairy milk, cheese and yoghurt. Then there are the tins of beans and packets of tofu.
But how much is actually healthy?
Our nutritional audit of more than 700 plant-based foods for sale in Australian supermarkets has just been published. We found some products are so high in salt or saturated fat, we’d struggle to call them “healthy”.
We took (several) trips to the supermarket
In 2022, we visited two of each of four major supermarket retailers across Melbourne to collect information on the available range of plant-based alternatives to meat and dairy products.
We took pictures of the products and their nutrition labels.
We then analysed the nutrition information on the packaging of more than 700 of these products. This included 236 meat substitutes, 169 legumes and pulses, 50 baked beans, 157 dairy milk substitutes, 52 cheese substitutes and 40 non-dairy yoghurts.
Plant-based meats were surprisingly salty
We found a wide range of plant-based meats for sale. So, it’s not surprising we found large variations in their nutrition content.
Sodium, found in added salt and which contributes to high blood pressure, was our greatest concern.
The sodium content varied from 1 milligram per 100 grams in products such as tofu, to 2,000mg per 100g in items such as plant-based mince products.
This means we could eat our entire daily recommended sodium intake in just one bowl of plant-based mince.
An audit of 66 plant-based meat products in Australian supermarkets conducted in 2014 found sodium ranged from 316mg in legume-based products to 640mg in tofu products, per 100g. In a 2019 audit of 137 products, the range was up to 1,200mg per 100g.
In other words, the results of our audit seems to show a consistent trend of plant-based meats getting saltier.
Looking for plant-based meat? Check the label for the sodium content.
Michael Vi/Shutterstock
What about plant-based milks?
Some 70% of the plant-based milks we audited were fortified with calcium, a nutrient important for bone health.
This is good news as a 2019-2020 audit of 115 plant-based milks from Melbourne and Sydney found only 43% of plant-based milks were fortified with calcium.
Of the fortified milks in our audit, almost three-quarters (73%) contained the recommended amount of calcium – at least 100mg per 100mL.
We also looked at the saturated fat content of plant-based milks.
Coconut-based milks had on average up to six times higher saturated fat content than almond, oat or soy milks.
Previous audits also found coconut-based milks were much higher in saturated fat than all other categories of milks.
Some plant-based milks were healthier than others.
TY Lim/Shutterstock
A first look at cheese and yoghurt alternatives
Our audit is the first study to identify the range of cheese and yoghurt alternatives available in Australian supermarkets.
Calcium was only labelled on a third of plant-based yoghurts, and only 20% of supermarket options met the recommended 100mg of calcium per 100g.
For plant-based cheeses, most (92%) were not fortified with calcium. Their sodium content varied from 390mg to 1,400mg per 100g, and saturated fat ranged from 0g to 28g per 100g.
So, what should we consider when shopping?
As a general principle, try to choose whole plant foods, such as unprocessed legumes, beans or tofu. These foods are packed with vitamins and minerals. They’re also high in dietary fibre, which is good for your gut health and keeps you fuller for longer.
If opting for a processed plant-based food, here are five tips for choosing a healthier option.
1. Watch the sodium
Plant-based meat alternatives can be high in sodium, so look for products that have around 150-250mg sodium per 100g.
2. Pick canned beans and legumes
Canned chickpeas, lentils and beans can be healthy and low-cost additions to many meals. Where you can, choose canned varieties with no added salt, especially when buying baked beans.
3. Add herbs and spices to your tofu
Tofu can be a great alternative to meat. Check the label and pick the option with the highest calcium content. We found flavoured tofu was higher in salt and sugar content than minimally processed tofu. So it’s best to pick an unflavoured option and add your own flavours with spices and herbs.
4. Check the calcium
When choosing a non-dairy alternative to milk, such as those made from soy, oat, or rice, check it is fortified with calcium. A good alternative to traditional dairy will have at least 100mg of calcium per 100g.
5. Watch for saturated fat
If looking for a lower saturated fat option, almond, soy, rice and oat varieties of milk and yoghurt alternatives have much lower saturated fat content than coconut options. Pick those with less than 3g per 100g.
Laura Marchese, PhD Student at the Institute for Physical Activity and Nutrition, Deakin University and Katherine Livingstone, NHMRC Emerging Leadership Fellow and Senior Research Fellow at the Institute for Physical Activity and Nutrition, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
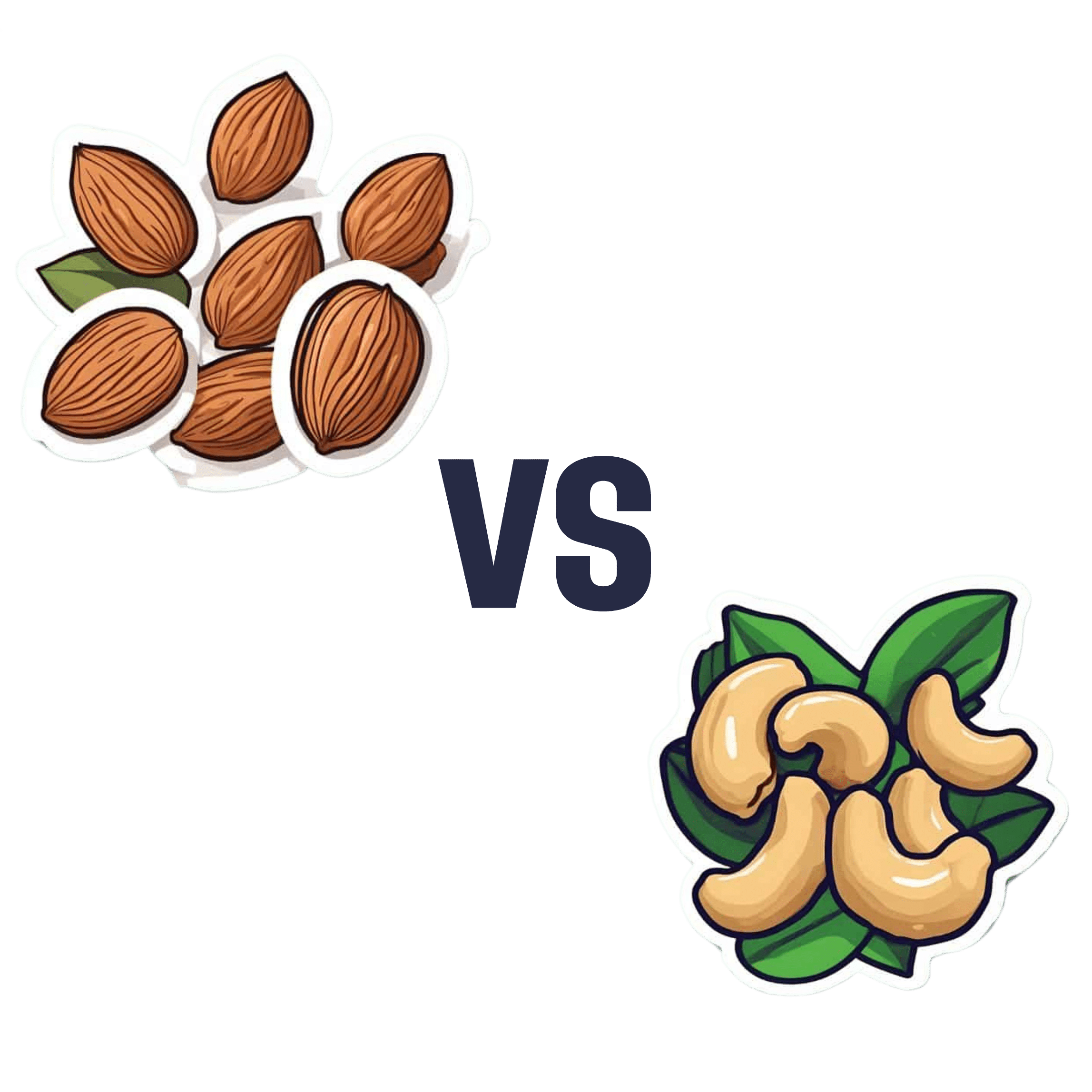
Almonds vs Cashews – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing almonds to cashews, we picked the almonds.
Why?
Both are great! But here’s why we picked the almonds:
In terms of macros, almonds have a little more protein and more than 4x the fiber. Given how critical fiber is to good health, and how most people in industrialized countries in general (and N. America in particular) aren’t getting enough, we consider this a major win for almonds.
Things are closer to even for vitamins, but almonds have a slight edge. Almonds are higher in vitamins A, B2, B3, B9, and especially 27x higher in vitamin E, while cashews are higher in vitamins B1, B5, B6, C & K. So, a moderate win for almonds.
In the category of minerals, cashews do a bit better on average. Cashews have moderately more copper, iron, phosphorus, selenium, and zinc, while almonds boast 6x more calcium, and slightly more manganese and potassium. We say this one’s a slight win for cashews.
Adding the categories up, however, makes it clear that almonds win the day.
However, of course, enjoy both! Diversity is healthy. Just, if you’re going to choose between them, we recommend almonds.
Want to learn more?
You might like to read:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Almonds vs Walnuts – Which is Healthier?
- Pistachios vs Cashews – Which is Healthier?
- Why You Should Diversify Your Nuts!
- What Matters Most For Your Heart?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: