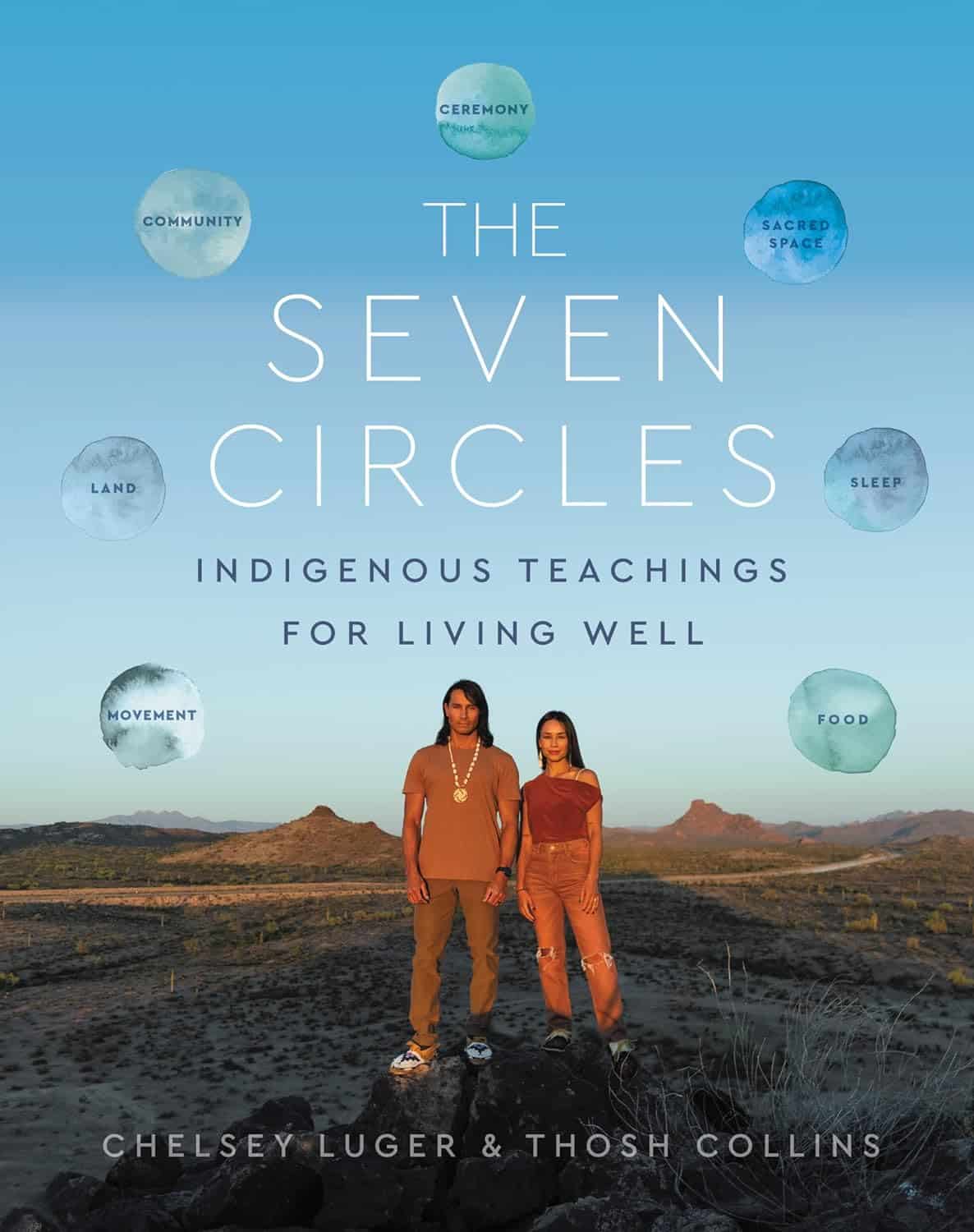
The Seven Circles – by Chelsey Luger & Thosh Collins
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At first glance, this can seem like an unscientific book—you won’t find links to studies in this one, for sure! However, if we take a look at the seven circles in question, they are:
- Food
- Movement
- Sleep
- Ceremony
- Sacred Space
- Land
- Community
Regular 10almonds readers may notice that these seven items contain five of the things strongly associated with the “supercentenarian Blue Zones”. (If you are wondering why Native American reservations are not Blue Zones, the answer there lies less in health science and more in history and sociology, and what things have been done to a given people).
The authors—who are Native American, yes—present in one place a wealth of knowledge and know-how. Not even just from their own knowledge and their own respective tribes, but gathered from other tribes too.
Perhaps the strongest value of this book to the reader is in the explanation of noting the size of each of those circles, how they connect with each other, and providing a whole well-explained system for how we can grow each of them in harmony with each other.
Or to say the same thing in sciencey terms: how to mindfully improve integrated lifestyle factors synergistically for greater efficacy and improved health-adjusted quality-of-life years.
Bottom line: if you’re not averse to something that mostly doesn’t use sciencey terms of have citations to peer-reviewed studies peppered through the text, then this book has wisdom that’s a) older than the pyramids of Giza, yet also b) highly consistent with our current best science of Blue Zone healthy longevity.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Regrow Receding Gums
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the problems with the human form is that our teeth evolved to last us for the whole of our life, with plenty of room to spare before our eventual death at the ripe old age of about 35 on average. Dr. Ellie Phillips advises those of us who might be a bit older than that, on how we can avoid becoming “too long in the tooth”—in other words, how to keep our gums, and thus our teeth, in place and healthy.
Getting to the root of the problem
The single biggest cause of gum recession is an acidic environment in the mouth, which harms teeth and gums alike. This acidic environment is produced not merely by consuming acid foods or drinks, but also (and much more often, and more problematically) by sugary foods and drinks, which are not necessarily themselves acidic, but they feed bacteria that release acids as a by-product of their metabolism. If we consume an acidic food or drink, it’s there for a moment, but if we then salivate and/or take a drink of water, it’s pretty much gone in a few seconds. But those bacteria when we feed them sugar? They are there to stay unless we do something more about them than just drink some water.
Other contributing factors to gum recession include teeth grinding, and (ironically) certain oral care products, especially many artificial teeth whiteners.
In case you were wondering: no, brushing will not* generally cause or even worsen gum recession, but flossing can exacerbate it if it’s already underway.
*unless, of course, you are using one of the whiteners we mentioned above
What to do about it: Dr. Phillips recommends:
- use a moderately firm toothbrush to massage gums and promote blood flow
- avoid acidic oral products and homemade remedies even if they’re not acidic but can be caustic, such as baking soda
- rebuild your gums’ and teeth’s protective biofilm (yes, there are “good bacteria” that are supposed to be there) with proper brushing
- avoid cleanings that are more intensive than brushing—skip flossing until your gums have recovered, too
- adjust your diet to avoid acids and (especially) sugars
10almonds note: she also recommends the use of xylitol to promote a healthy oral environment; we don’t recommend that, as while it may be great for the teeth, studies have found it to be bad for the heart.
For more on all of her advices and a bit more of the science of it, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Toothpastes & Mouthwashes: Which Help And Which Harm?
- Flossing Without Flossing?
- Less Common Oral Hygiene Options ← including the miswak “chewing stick”, which even outperformed toothbrushes in clinical trials, by biochemically altering the composition of the saliva while gently cleaning like a toothbrush.
- Fluoride Toothpaste vs Non-Fluoride Toothpaste – Which is Healthier?
- Non-Alcohol Mouthwash vs Alcohol Mouthwash – Which is Healthier?
- Xylitol vs Erythritol – Which is Healthier?
Take care!
Share This Post
-
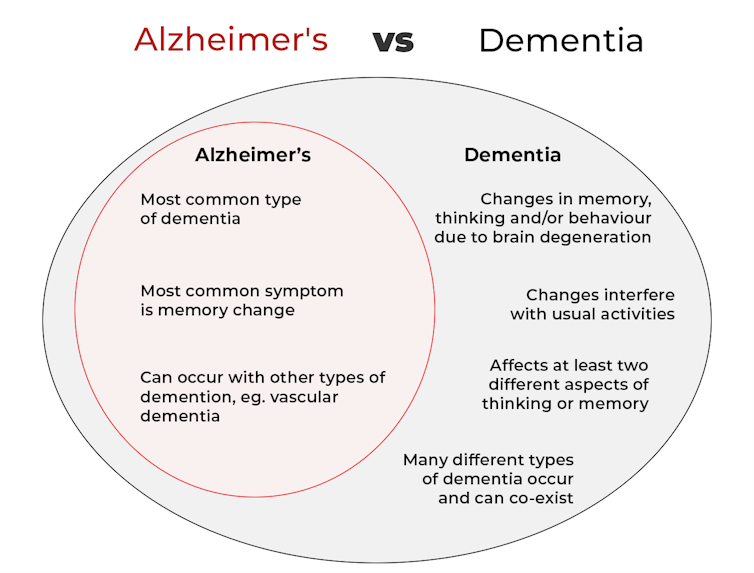
What’s the difference between Alzheimer’s and dementia?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
Changes in thinking and memory as we age can occur for a variety of reasons. These changes are not always cause for concern. But when they begin to disrupt daily life, it could indicate the first signs of dementia.
Another term that can crop up when we’re talking about dementia is Alzheimer’s disease, or Alzheimer’s for short.
So what’s the difference?
Lightspring/Shutterstock What is dementia?
Dementia is an umbrella term used to describe a range of syndromes that result in changes in memory, thinking and/or behaviour due to degeneration in the brain.
To meet the criteria for dementia these changes must be sufficiently pronounced to interfere with usual activities and are present in at least two different aspects of thinking or memory.
For example, someone might have trouble remembering to pay bills and become lost in previously familiar areas.
It’s less-well known that dementia can also occur in children. This is due to progressive brain damage associated with more than 100 rare genetic disorders. This can result in similar cognitive changes as we see in adults.
So what’s Alzheimer’s then?
Alzheimer’s is the most common type of dementia, accounting for about 60-80% of cases.
So it’s not surprising many people use the terms dementia and Alzheimer’s interchangeably.
Changes in memory are the most common sign of Alzheimer’s and it’s what the public most often associates with it. For instance, someone with Alzheimer’s may have trouble recalling recent events or keeping track of what day or month it is.
People with dementia may have trouble keeping track of dates. Daisy Daisy/Shutterstock We still don’t know exactly what causes Alzheimer’s. However, we do know it is associated with a build-up in the brain of two types of protein called amyloid-β and tau.
While we all have some amyloid-β, when too much builds up in the brain it clumps together, forming plaques in the spaces between cells. These plaques cause damage (inflammation) to surrounding brain cells and leads to disruption in tau. Tau forms part of the structure of brain cells but in Alzheimer’s tau proteins become “tangled”. This is toxic to the cells, causing them to die. A feedback loop is then thought to occur, triggering production of more amyloid-β and more abnormal tau, perpetuating damage to brain cells.
Alzheimer’s can also occur with other forms of dementia, such as vascular dementia. This combination is the most common example of a mixed dementia.
Vascular dementia
The second most common type of dementia is vascular dementia. This results from disrupted blood flow to the brain.
Because the changes in blood flow can occur throughout the brain, signs of vascular dementia can be more varied than the memory changes typically seen in Alzheimer’s.
For example, vascular dementia may present as general confusion, slowed thinking, or difficulty organising thoughts and actions.
Your risk of vascular dementia is greater if you have heart disease or high blood pressure.
Frontotemporal dementia
Some people may not realise that dementia can also affect behaviour and/or language. We see this in different forms of frontotemporal dementia.
The behavioural variant of frontotemporal dementia is the second most common form (after Alzheimer’s disease) of younger onset dementia (dementia in people under 65).
People living with this may have difficulties in interpreting and appropriately responding to social situations. For example, they may make uncharacteristically rude or offensive comments or invade people’s personal space.
Semantic dementia is also a type of frontotemporal dementia and results in difficulty with understanding the meaning of words and naming everyday objects.
Dementia with Lewy bodies
Dementia with Lewy bodies results from dysregulation of a different type of protein known as α-synuclein. We often see this in people with Parkinson’s disease.
So people with this type of dementia may have altered movement, such as a stooped posture, shuffling walk, and changes in handwriting. Other symptoms include changes in alertness, visual hallucinations and significant disruption to sleep.
Do I have dementia and if so, which type?
If you or someone close to you is concerned, the first thing to do is to speak to your GP. They will likely ask you some questions about your medical history and what changes you have noticed.
Sometimes it might not be clear if you have dementia when you first speak to your doctor. They may suggest you watch for changes or they may refer you to a specialist for further tests.
There is no single test to clearly show if you have dementia, or the type of dementia. A diagnosis comes after multiple tests, including brain scans, tests of memory and thinking, and consideration of how these changes impact your daily life.
Not knowing what is happening can be a challenging time so it is important to speak to someone about how you are feeling or to reach out to support services.
Dementia is diverse
As well as the different forms of dementia, everyone experiences dementia in different ways. For example, the speed dementia progresses varies a lot from person to person. Some people will continue to live well with dementia for some time while others may decline more quickly.
There is still significant stigma surrounding dementia. So by learning more about the various types of dementia and understanding differences in how dementia progresses we can all do our part to create a more dementia-friendly community.
The National Dementia Helpline (1800 100 500) provides information and support for people living with dementia and their carers. To learn more about dementia, you can take this free online course.
Nikki-Anne Wilson, Postdoctoral Research Fellow, Neuroscience Research Australia (NeuRA), UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Diet Tips for Crohn’s Disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Doctors are great at saving lives like mine. I’m a two time survivor of colon cancer and have recently been diagnosed with Chron’s disease at 62. No one is the health system can or is prepared to tell me an appropriate diet to follow or what to avoid. Can you?❞
Congratulations on the survivorship!
As to Crohn’s, that’s indeed quite a pain, isn’t it? In some ways, a good diet for Crohn’s is the same as a good diet for most other people, with one major exception: fiber
…and unfortunately, that changes everything, in terms of a whole-foods majority plant-based diet.
What stays the same:
- You still ideally want to eat a lot of plants
- You definitely want to avoid meat and dairy in general
- Eating fish is still usually* fine, same with eggs
- Get plenty of water
What needs to change:
- Consider swapping grains for potatoes or pasta (at least: avoid grains)
- Peel vegetables that are peelable; discard the peel or use it to make stock
- Consider steaming fruit and veg for easier digestion
- Skip spicy foods (moderate spices, like ginger, turmeric, and black pepper, are usually fine in moderation)
Much of this latter list is opposite to the advice for people without Crohn’s Disease.
*A good practice, by the way, is to keep a food journal. There are apps that you can get for free, or you can do it the old-fashioned way on paper if prefer.
But the important part is: make a note not just of what you ate, but also of how you felt afterwards. That way, you can start to get a picture of patterns, and what’s working (or not) for you, and build up a more personalized set of guidelines than anyone else could give to you.
We hope the above pointers at least help you get going on the right foot, though!
Share This Post
Related Posts
-
Anchovies vs Sardines – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing anchovies to sardines, we picked the sardines.
Why?
In terms of macros, sardines have slightly more protein and more than 2x the fat, but the fat profile is healthier than that of anchovies, meaning that the amount of saturated fat is the same, and sardines have more poly- and monounsaturated fats. Breaking it down further, sardines also have more omega-3. Unless you are for whatever reason especially keen to keep your total fat* intake down, sardines win here.
*or calories, which in this case come almost entirely from the fat, and sardines are consequently nearly 2x higher in calories.
When it comes to vitamins, sardines further distinguish themselves; anchovies have more of vitamins B2 and B3, while sardines have more of vitamins A, B1, B6, B12, B9, E, and K—in some cases, by quite large margins (especially the B12 and K, being 14x more and 26x more, respectively). A clear win for sardines.
Minerals are closer to even; anchovies have more copper, iron, and zinc, while sardines have more calcium, manganese, phosphorus, and selenium. That’s already a slight win for sardines, before we take into account that sardines’ margins of difference are also much greater than anchovies’.
In short, enjoy either in moderation if you are so inclined, but sardines win on overall nutritional density.
Want to learn more?
You might like to read:
Farmed Fish vs Wild Caught: More Important Than You Might Think
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The 7 Known Risk Factors For Dementia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A recent UK-based survey found that…
- while nearly half of adults say dementia is the disease they fear most,
- only a third of those thought you could do anything to avoid it, and
- just 1% could name the 7 known risk factors.
Quick test
Can you name the 7 known risk factors?
Please take a moment to actually try (this kind of mental stimulation is good in any case), and count them out on your fingers (or write them down), and then…
Answer (no peeking if you haven’t listed them yet)
The 7 known risk factors are:
*drumroll please*
- Smoking
- High blood pressure
- Diabetes
- Obesity
- Depression
- Lack of mental stimulation
- Lack of physical activity
How many did you get? If you got them all, well done. If not, then well, now you know, so that’s good.
Did you come here from our “Future-Proof Your Brain” article? If so, you can get back to it here ← and if you didn’t, you should check it out anyway; it’s worth it😉
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
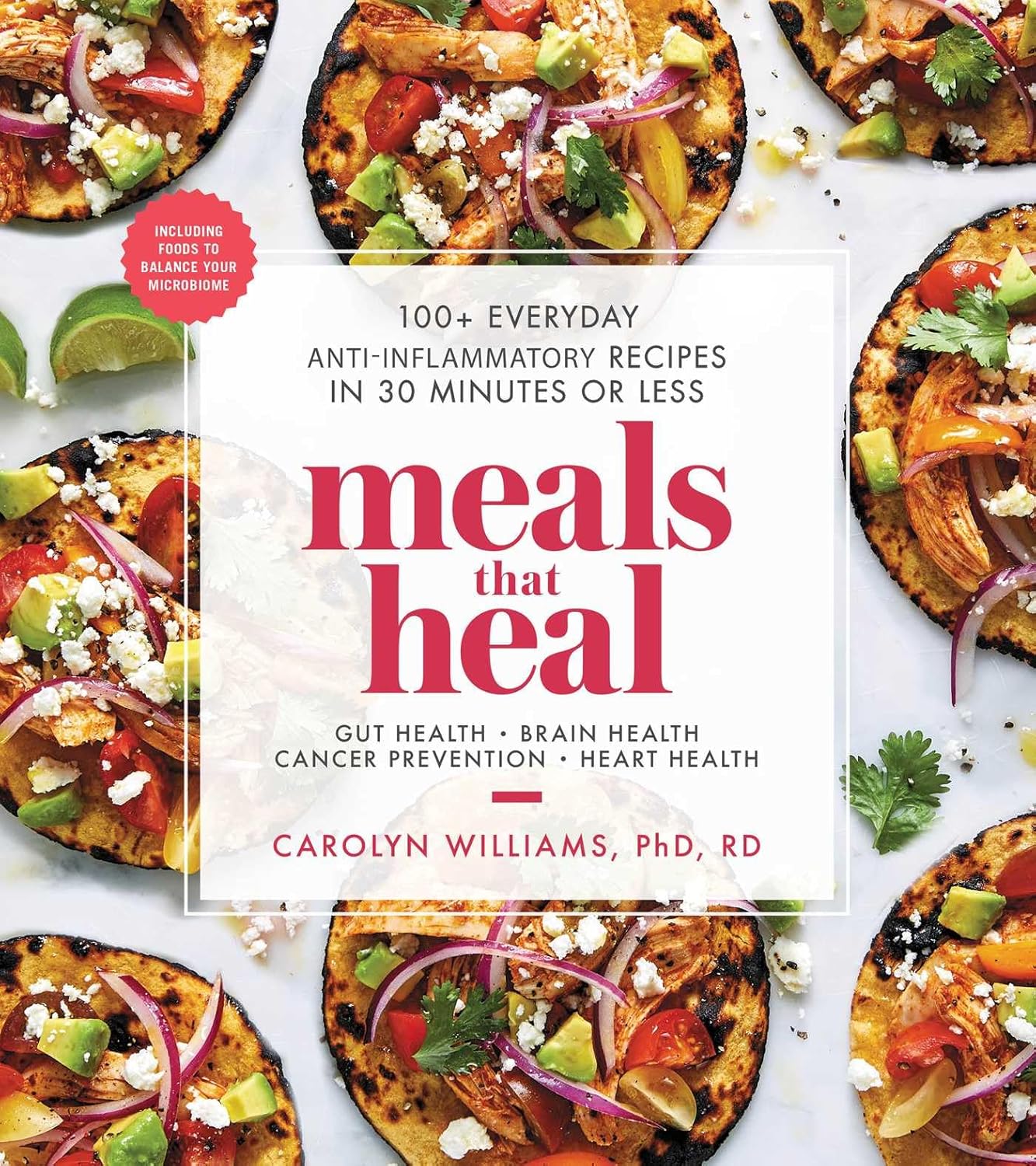
Meals That Heal – by Dr. Carolyn Williams
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Inflammation is implicated as a contributory or casual factor in almost all chronic diseases (and still exacerbates the ones in which it’s not directly implicated causally), so if there’s one area of health to focus on with one’s diet, then reducing inflammation is a top candidate.
This book sets about doing exactly that.
You may be wondering whether, per the book’s subtitle, they can really all be done in 30 minutes or under. The answer is: no, not unless you have a team of sous-chefs to do all the prep work for you, and line up everything mise-en-place style for when you start the clock. If you do have that team of sous-chefs working for you, then you can probably do most of them in under 30 minutes. If you don’t have that team, then budget about an hour in total, sometimes less, sometimes more, depending on the recipe.
The recipes themselves are mostly Mediterranean-inspired, though you might want to do a few swaps where the author has oddly recommended using seed oils instead of olive oil, or plant milk in place of where she has used dairy milk in a couple of “recipes” for smoothies. You might also want to be a little more generous with the seasonings, if you’re anything like this reviewer.
Bottom line: if you’re looking for an anti-inflammatory starter cookbook, you could do worse than this. You could probably do better, too, such as starting with The Inflammation Spectrum – by Dr. Will Cole.
Alternatively, click here if you want to check out Meals That Heal, and dive straight in!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: