The first pig kidney has been transplanted into a living person. But we’re still a long way from solving organ shortages
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a world first, we heard last week that US surgeons had transplanted a kidney from a gene-edited pig into a living human. News reports said the procedure was a breakthrough in xenotransplantation – when an organ, cells or tissues are transplanted from one species to another. https://www.youtube.com/embed/cisOFfBPZk0?wmode=transparent&start=0 The world’s first transplant of a gene-edited pig kidney into a live human was announced last week.
Champions of xenotransplantation regard it as the solution to organ shortages across the world. In December 2023, 1,445 people in Australia were on the waiting list for donor kidneys. In the United States, more than 89,000 are waiting for kidneys.
One biotech CEO says gene-edited pigs promise “an unlimited supply of transplantable organs”.
Not, everyone, though, is convinced transplanting animal organs into humans is really the answer to organ shortages, or even if it’s right to use organs from other animals this way.
There are two critical barriers to the procedure’s success: organ rejection and the transmission of animal viruses to recipients.
But in the past decade, a new platform and technique known as CRISPR/Cas9 – often shortened to CRISPR – has promised to mitigate these issues.
What is CRISPR?
CRISPR gene editing takes advantage of a system already found in nature. CRISPR’s “genetic scissors” evolved in bacteria and other microbes to help them fend off viruses. Their cellular machinery allows them to integrate and ultimately destroy viral DNA by cutting it.
In 2012, two teams of scientists discovered how to harness this bacterial immune system. This is made up of repeating arrays of DNA and associated proteins, known as “Cas” (CRISPR-associated) proteins.
When they used a particular Cas protein (Cas9) with a “guide RNA” made up of a singular molecule, they found they could program the CRISPR/Cas9 complex to break and repair DNA at precise locations as they desired. The system could even “knock in” new genes at the repair site.
In 2020, the two scientists leading these teams were awarded a Nobel prize for their work.
In the case of the latest xenotransplantation, CRISPR technology was used to edit 69 genes in the donor pig to inactivate viral genes, “humanise” the pig with human genes, and knock out harmful pig genes. https://www.youtube.com/embed/UKbrwPL3wXE?wmode=transparent&start=0 How does CRISPR work?
A busy time for gene-edited xenotransplantation
While CRISPR editing has brought new hope to the possibility of xenotransplantation, even recent trials show great caution is still warranted.
In 2022 and 2023, two patients with terminal heart diseases, who were ineligible for traditional heart transplants, were granted regulatory permission to receive a gene-edited pig heart. These pig hearts had ten genome edits to make them more suitable for transplanting into humans. However, both patients died within several weeks of the procedures.
Earlier this month, we heard a team of surgeons in China transplanted a gene-edited pig liver into a clinically dead man (with family consent). The liver functioned well up until the ten-day limit of the trial.
How is this latest example different?
The gene-edited pig kidney was transplanted into a relatively young, living, legally competent and consenting adult.
The total number of gene edits edits made to the donor pig is very high. The researchers report making 69 edits to inactivate viral genes, “humanise” the pig with human genes, and to knockout harmful pig genes.
Clearly, the race to transform these organs into viable products for transplantation is ramping up.
From biotech dream to clinical reality
Only a few months ago, CRISPR gene editing made its debut in mainstream medicine.
In November, drug regulators in the United Kingdom and US approved the world’s first CRISPR-based genome-editing therapy for human use – a treatment for life-threatening forms of sickle-cell disease.
The treatment, known as Casgevy, uses CRISPR/Cas-9 to edit the patient’s own blood (bone-marrow) stem cells. By disrupting the unhealthy gene that gives red blood cells their “sickle” shape, the aim is to produce red blood cells with a healthy spherical shape.
Although the treatment uses the patient’s own cells, the same underlying principle applies to recent clinical xenotransplants: unsuitable cellular materials may be edited to make them therapeutically beneficial in the patient.

We’ll be talking more about gene-editing
Medicine and gene technology regulators are increasingly asked to approve new experimental trials using gene editing and CRISPR.
However, neither xenotransplantation nor the therapeutic applications of this technology lead to changes to the genome that can be inherited.
For this to occur, CRISPR edits would need to be applied to the cells at the earliest stages of their life, such as to early-stage embryonic cells in vitro (in the lab).
In Australia, intentionally creating heritable alterations to the human genome is a criminal offence carrying 15 years’ imprisonment.
No jurisdiction in the world has laws that expressly permits heritable human genome editing. However, some countries lack specific regulations about the procedure.
Is this the future?
Even without creating inheritable gene changes, however, xenotransplantation using CRISPR is in its infancy.
For all the promise of the headlines, there is not yet one example of a stable xenotransplantation in a living human lasting beyond seven months.
While authorisation for this recent US transplant has been granted under the so-called “compassionate use” exemption, conventional clinical trials of pig-human xenotransplantation have yet to commence.
But the prospect of such trials would likely require significant improvements in current outcomes to gain regulatory approval in the US or elsewhere.
By the same token, regulatory approval of any “off-the-shelf” xenotransplantation organs, including gene-edited kidneys, would seem some way off.
Christopher Rudge, Law lecturer, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Sea Salt vs MSG – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sea salt to MSG, we picked the MSG.
Why?
Surprise! Or maybe not? The results of the poll for this one should be interesting, and will help us know whether we need to keep mentioning in every second recipe that MSG is a healthier alternative to salt.
First of all, two things:
- Don’t be fooled by their respective names, and/or with such, an appeal to naturalism. For example, hydroxybenzoic acids are a major group of beneficial phenolic compounds, whereas hemlock is a wildflower that grows in this writer’s garden and will kill you if you eat it. Actually hydroxybenzoic acids also grow here (on the apple tree), but that’s not the point. The point is: worry less about names, and more about evidence!
- Don’t be fooled by the packaging. A lot of products go for “greenwashing” of one kind or another. You’re not eating the packaging (hopefully), so don’t be swayed by a graphic designer’s implementation of a marketing team’s aesthetic choices.
If naturalism is for some reason very important to you though, do bear in mind that glutamates occur generously in many common foodstuffs (tomatoes are a fine, healthy example) and eating tomato in the presence of salt will have the same biochemical effect as eating MSG, because it’s the same chemicals.
Since there are bad rumors about MSG’s safety, especially in the US where there is often a strong distrust of anything associated with China (actually MSG was first isolated in Japan, more than 100 years ago, by Japanese biochemist Dr. Kikunae Ikeda, but that gets drowned out by the “Chinese Restaurant Syndrome” fear in the US), know that this has resulted in MSG being one of the most-studied food additives in the last 40 years or so, with many teams of scientists trying to determine its risks and not finding any (aside from the same that could be said of any substance; anything in sufficient excess will kill you, including water or oxygen).
Well, that’s all been about safety, but what makes it healthier than sea salt?
Simply, it has about ⅓ of the sodium content, that’s all. So, if you are laboring all day in a field under the hot summer sun, then probably the sea salt will be healthier, to replenish more of the sodium you lost through sweat. But for most people most of the time, having less sodium rather than more is the healthier option.
Want to learn more?
You might like to read:
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
- MSG vs. Salt: Sodium Comparison ← here be chemistry
- More Salt, Not Less? ← No
- Pink Himalayan Salt: Health Facts
Take care!
Share This Post
-
Sleeping on Your Back after 50; Yay or Nay?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sleeping Differently After 50
Sleeping is one of those things that, at any age, can be hard to master. Some of our most popular articles have been on getting better sleep, and effective sleep aids, and we’ve had a range of specific sleep-related questions, like whether air purifiers actually improve your sleep.
But perhaps there’s an underlying truth hidden in our opening sentence…is sleeping consistently difficult because the way we sleep should change according to our age?
Inspired by Brad and Mike’s video below (which was published to their 5 million+ subscribers!), there are 4 main elements to consider when sleeping on your back after you’ve hit the 50-year mark:
- Degenerative Disk Disease: As you age, your spine may start to show signs of wear and tear, which directly affects comfort while lying on your back.
- Sleep Apnea and Snoring: Sleep Apnea and snoring become more of an issue with age, and sleeping on your back can exacerbate these problems; when you sleep on your back, the soft tissues in your throat, as well as your tongue, “fall back” and partly obstruct your the airway.
- Spinal Stenosis: Spinal Stenosis–the often-age-related narrowing of your spinal canal–can put pressure on the nerves that travel through the spine, which equally makes back-sleeping harder.
- GERD: The all-too-familiar gastroesophageal reflux disease can be more problematic when lying flat on your back, as doing so can allow easy access for stomach acid to move upwards.
Alternatives to Back Sleeping
Referencing the Mayo Clinic’s Sleep Facility’s director, Dr. Virend Somers, today’s video suggests a simple solution: sleeping on your side. The video goes into a bit more detail but, as you know, here at 10almonds we like to cut to the chase.
Modifications for Back Sleeping
If you’re a lifelong back-sleeping and cannot bear the idea of changing to your side, or your stomach, then there are a few modifications that you can make to ease any pain and discomfort.
Most solutions revolve around either leg wedges or pillow adjustments. For instance, if you’re suffering from back pain, try propping your knees up. Or if GERD is your worst enemy, a wedge pillow could help keep that acid down.
As can be expected, the video dives into more detail:
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Share This Post
-
Blood, urine and other bodily fluids: how your leftover pathology samples can be used for medical research
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A doctor’s visit often ends with you leaving with a pathology request form in hand. The request form soon has you filling a sample pot, having blood drawn, or perhaps even a tissue biopsy taken.
After that, your sample goes to a clinical pathology lab to be analysed, in whichever manner the doctor requested. All this is done with the goal of getting to the bottom of the health issue you’re experiencing.
But after all the tests are done, what happens with the leftover sample? In most cases, leftover samples go in the waste bin, destined for incineration. Sometimes though, they may be used again for other purposes, including research.
Kaboompics.com/Pexels Who can use my leftover samples?
The samples we’re talking about here cover the range of samples clinical labs receive in the normal course of their testing work. These include blood and its various components (including plasma and serum), urine, faeces, joint and spinal fluids, swabs (such as from the nose or a wound), and tissue samples from biopsies, among others.
Clinical pathology labs often use leftover samples to practise or check their testing methods and help ensure test accuracy. This type of use is a vital part of the quality assurance processes labs need to perform, and is not considered research.
Leftover samples can also be used by researchers from a range of agencies such as universities, research institutes or private companies.
They may use leftover samples for research activities such as trying out new ideas or conducting small-scale studies (more on this later). Companies that develop new or improved medical diagnostic tests can also use leftover samples to assess the efficacy of their test, generating data needed for regulatory approval.
What about informed consent?
If you’ve ever participated in a medical research project such as a clinical trial, you may be familiar with the concept of informed consent. In this process, you have the opportunity to learn about the study and what your participation involves, before you decide whether or not to participate.
So you may be surprised to learn using leftover samples for research purposes without your consent is permitted in most parts of Australia, and elsewhere. However, it’s only allowed under certain conditions.
In Australia, the National Health and Medical Research Council (NHMRC) offers guidance around the use of leftover pathology samples.
One of the conditions for using leftover samples without consent for research is that they were received and retained by an accredited pathology service. This helps ensure the samples were collected safely and properly, for a legitimate clinical reason, and that no additional burdens or risk of harm to the person who provided the sample will be created with their further use.
Another condition is anonymity: the leftover samples must be deidentified, and not easily able to be reidentified. This means they can only be used in research if the identity of the donor is not needed.
Leftover pathology samples are sometimes used in medical research. hedgehog94/Shutterstock The decision to allow a particular research project to use leftover pathology samples is made by an independent human research ethics committee which includes consumers and independent experts. The committee evaluates the project and weighs up the risks and potential benefits before permitting an exemption to the need for informed consent.
Similar frameworks exist in the United States, the United Kingdom, India and elsewhere.
What research might be done on my leftover samples?
You might wonder how useful leftover samples are, particularly when they’re not linked to a person and their medical history. But these samples can still be a valuable resource, particularly for early-stage “discovery” research.
Research using leftover samples has helped our understanding of antibiotic resistance in a bacterium that causes stomach ulcers, Helicobacter pylori. It has helped us understand how malaria parasites, Plasmodium falciparum, damage red blood cells.
Leftover samples are also helping researchers identify better, less invasive ways to detect chronic diseases such as pulmonary fibrosis. And they’re allowing scientists to assess the prevalence of a variant in haemoglobin that can interfere with widely used diagnostic blood tests.
All of this can be done without your permission. The kinds of tests researchers do on leftover samples will not harm the person they were taken from in any way. However, using what would otherwise be discarded allows researchers to test a new method or treatment and avoid burdening people with providing fresh samples specifically for the research.
When considering questions of ethics, it could be argued not using these samples to derive maximum benefit is in fact unethical, because their potential is wasted. Using leftover samples also minimises the cost of preliminary studies, which are often funded by taxpayers.
The use of leftover pathology samples in research has been subject to some debate. Andrey_Popov/Shutterstock Inconsistencies in policy
Despite NHMRC guidance, certain states and territories have their own legislation and guidelines which differ in important ways. For instance, in New South Wales, only pathology services may use leftover specimens for certain types of internal work. In all other cases consent must be obtained.
Ethical standards and their application in research are not static, and they evolve over time. As medical research continues to advance, so too will the frameworks that govern the use of leftover samples. Nonetheless, developing a nationally consistent approach on this issue would be ideal.
Striking a balance between ensuring ethical integrity and fostering scientific discovery is essential. With ongoing dialogue and oversight, leftover pathology samples will continue to play a crucial role in driving innovation and advances in health care, while respecting the privacy and rights of individuals.
Christine Carson, Senior Research Fellow, School of Medicine, The University of Western Australia and Nikolajs Zeps, Professor, School of Public Health and Preventive Medicine, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
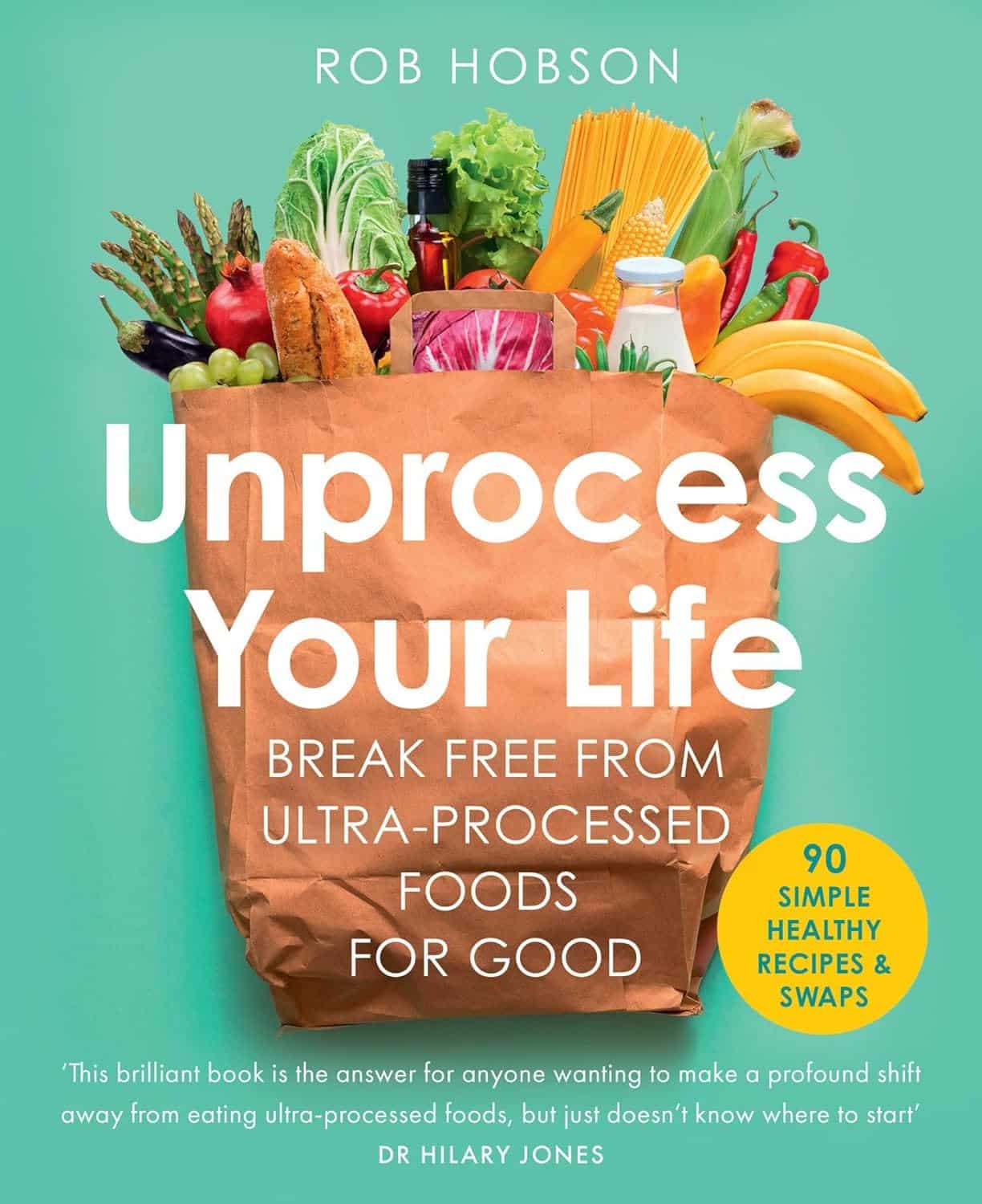
Unprocess Your Life – by Rob Hobson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Rob Hobson is not a doctor, but he is a nutritionist with half the alphabet after his name (BSc, PGDip, MSc, AFN, SENR) and decades of experience in the field.
The book covers, in jargon-free fashion, the science of ultra-processed foods, and why for example that pack of frozen chicken nuggets are bad but a pack of tofu (which obviously also took some processing, because it didn’t grow on the plant like that) isn’t.
This kind of explanation puts to rest a lot of the “does this count?” queries that a reader might have when giving the shopping list a once-over.
He also covers practical considerations such as kitchen equipment that’s worth investing in if you don’t already have it, and an “unprocessed pantry” shopping list.
The recipes (yes, there are recipes, nearly a hundred of them) are not plant-based by default, but there is a section of vegan and vegetarian recipes. Given that the theme of the book is replacing ultra-processed foods, it doesn’t mean a life of abstemiousness—there are recipes for all manner of things from hot sauce to cakes. Just, healthier unprocessed ones! There are classically healthy recipes too, of course.
Bottom line: if you’ve been wishing for a while that you could get rid of those processed products that are just so convenient that you haven’t got around to replacing them with healthier options, this book can indeed help you do just that.
Click here to check out Unprocess Your Life, and unprocess your life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Bored of Lunch – by Nathan Anthony
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cooking with a slow cooker is famously easy, but often we settle down on a few recipes and then don’t vary. This book brings a healthy dose of inspiration and variety.
The recipes themselves range from comfort food to fancy entertaining, pasta dishes to risottos, and even what the author categorizes as “fakeaways” (a play on the British English “takeaway”, cf. AmE “takeout”), so indulgent nights in have never been healthier!
For each recipe, you’ll see a nice simple clear layout of all you’d expect (ingredients, method, etc) plus calorie count, so that you can have a rough idea of how much food each meal is.
In terms of dietary restrictions you may have, there’s quite a variety here so it’ll be easy to find things for all needs, and in addition to that, optional substitutions are mostly quite straightforward too.
Bottom line: if you have a slow cooker but have been cooking only the same three things in it for the past ten years, this is the book to liven things up, while staying healthy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healthy Homemade Flatbreads
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our recipes sometimes call for the use of flatbreads, or suggest serving with flatbreads. But we want you to be able to have healthy homemade ones! So here’s a very quick and easy recipe. You’ll probably need to order some of the ingredients in, but it’s worth it, and then if you keep a stock of the ingredients, you can whip these up in minutes anytime you want them.
You will need
- 1 cup garbanzo bean flour, plus more for dusting
- 1 cup quinoa flour
- 2 tbsp ground/milled flaxseed
- 1 tbsp baking powder
- 1 tbsp extra virgin olive oil, plus more for the pan
- ½ tsp MSG, or 1 tsp low-sodium salt, with MSG being the healthier and preferable option
- ½ tsp onion powder
- ½ tsp garlic powder
- ½ tsp dried cumin
- ½ tsp dried thyme
Method
(we suggest you read everything at least once before doing anything)
1) Mix the flaxseed with ⅓ cup of water and set aside for at least 5 minutes.
2) Combine the rest of the ingredients in a big bowl, plus the flax mixtures we just made, and an extra ½ cup of water. Knead this into a dough, adding a touch more water if it becomes necessary, but be sparing with it.
3) Divide the dough into 6 equal portions, shaping each into a ball. Dust a clean surface with the extra garbanzo bean flour, and roll each dough ball into in a thin 6″ circle.
4) Heat a skillet and add some olive oil for frying; when hot enough, place a dough disk in the pan and cook for a few minutes on each side until golden brown. Repeat with the other 5.
5) Serve! If you’re looking for a perfect accompaniment to these, try our Hero Homemade Hummus
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: