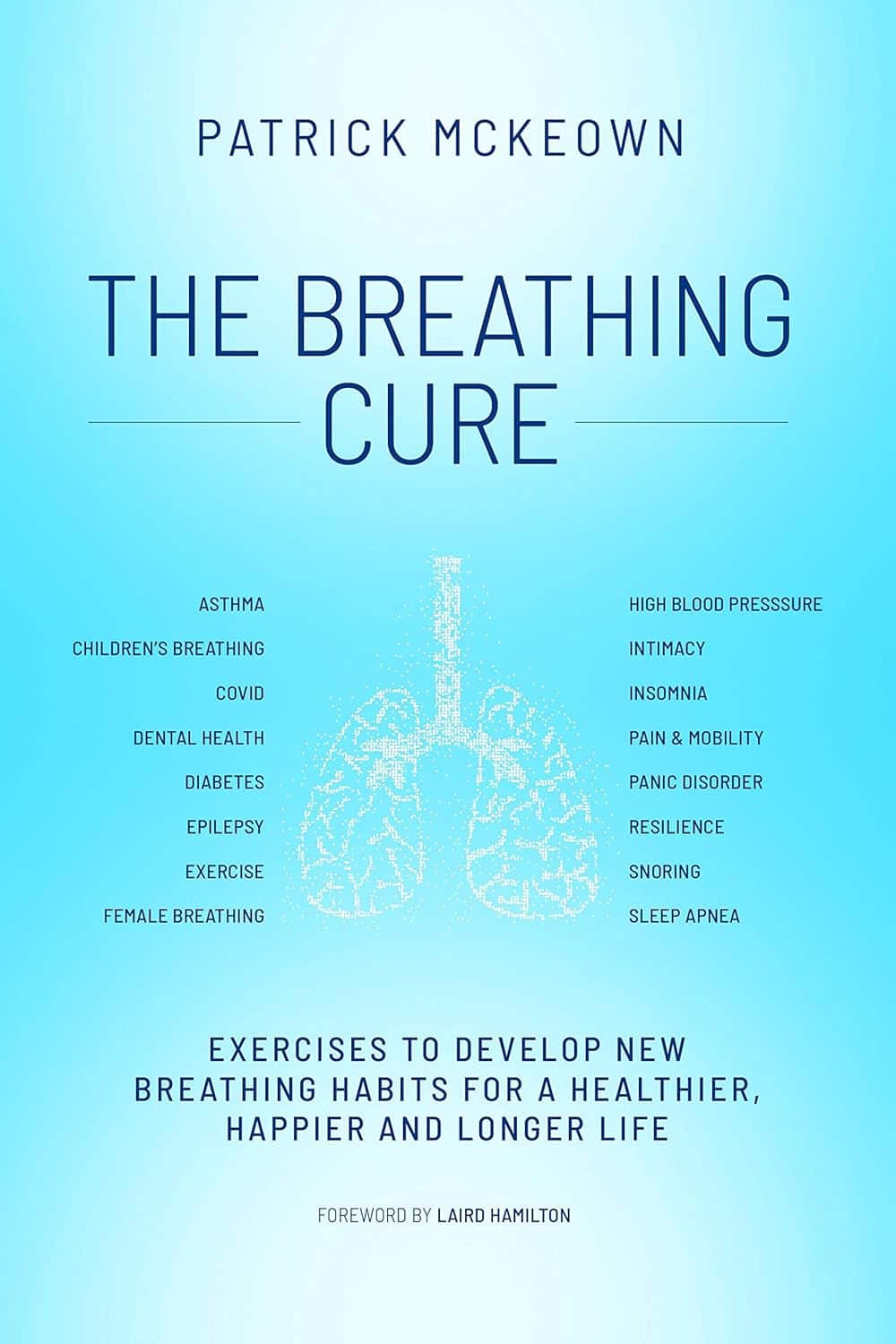
The Breathing Cure – by Patrick McKeown
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed this author’s “The Oxygen Advantage”, which as you might guess from the title, was also about breathing. So, what’s different here?
While The Oxygen Advantage was mostly about improving good health with optimized breathing, and with an emphasis on sports too, The Breathing Cure is more about the two-way relationship between ill health and disordered breathing (and how to fix it).
Many kinds of illnesses can affect our breathing, and our breathing can affect many types of illness; McKeown covers a lot of these, including the obvious things like respiratory diseases (including COVID and Long COVID, as well as non-infectious respiratory conditions like asthma), but also things like diabetes and heart disease, as well as peri-disease things like chronic pain, and demi-disease things like periods and menopause.
In each case (and more), he examines what things make matters better or worse, and how to improve them.
While the style itself is just as pop-science as The Oxygen Advantage, this time it relies less on anecdote (though there are plenty of anecdotes too), and leans more heavily on a generous chapter-by-chapter scientific bibliography, with plenty of citations to back up claims.
Bottom line: if you’d like to breathe better, this book can help in very many ways.
Click here to check out The Breathing Cure, and breathe easy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Widen the Window – by Dr. Elizabeth Stanley
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, about the title… That “window” that the author bids us “widen” is not a flowery metaphor, but rather, is referring to the window of exhibited resilience to stress/trauma; the “window” in question looks like an “inverted U” bell-curve on the graph.
In other words: Dr. Stanley’s main premise here is that we respond best to moderate stress (i.e: in that window, the area under the curve!), but if there is too little or too much, we don’t do so well. The key, she argues, is widening that middle part (expanding the area under the curve) in which we perform optimally. That way, we can still function in a motivated fashion without extrinsic threats, and we also don’t collapse under the weight of overwhelm, either.
The main strength of this book, however, lies in its practical exercises to accomplish that—and more.
“And more”, because the subtitle also promised recovery from trauma, and the author delivers in that regard too. In this case, it’s about widening that same window, but this time to allow one’s parasympathetic nervous system to recognize that the traumatic event is behind us, and no longer a threat; we are safe now.
Bottom line: if you would like to respond better to stress, and/or recover from trauma, this book is a very good tool.
Share This Post
-
The Power of When – by Dr. Michael Breus
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There’s a lot more to one’s circadian rhythm than just when one wakes and sleeps. This book goes into that quite deeply!
For example, those items in the subtitle? You could do them all at the same time, but it probably wouldn’t be optimal (although honestly, that does sound like quite a good life!). Rather, there are distinct times of day that we’re going to be better at certain things, and there are distinct times of day when certain things are going to be better for us.
Of course, some items are not so simple as a one-size fits all, so Dr. Breus outlines for us how to figure out our own chronotype (within four main schemas), and how to make that work for us as well as possible.
They style is easy-reading pop-science, with frequent summaries, bullet-points, quizzes, and so forth, making it easy to understand, learn, and apply.
Bottom line: if you feel like your sleep could use a do-over, then this book can help you get it into order—and the rest of your daily activities too!
Click here to check out The Power of When, and optimize your health!
Share This Post
-
Superfood-Stuffed Squash
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This stuffed squash recipe is packed with so many nutrient-dense ingredients, yet it feels delightfully decadent—a great recipe to have up your sleeve ready for fall.
You will need
- 1 large or two medium butternut squashes, halved lengthways and seeds removed (keep them; they are full of nutrients! You can sprout them, or dry them to use them at your leisure), along with some of the flesh from the central part above where the seeds are, so that there is room for stuffing
- 2 cups low-sodium vegetable stock
- 1 cup wild rice, rinsed
- 1 medium onion, finely chopped
- ½ cup walnuts, roughly chopped
- ½ cup dried
cranberriesgoji berries ← why goji berries? They have even more healthful properties than cranberries, and cranberries are hard to buy without so much added sugar that the ingredients list looks like “cranberries (51%), sugar (39%), vegetable oil (10%)”, whereas when buying goji berries, the ingredients list says “goji berries”, and they do the same culinary job. - ¼ cup pine nuts
- ½ bulb garlic, minced
- 1 tbsp dried thyme or 2 tsp fresh thyme, destalked
- 1 tbsp dried rosemary or 2 tsp fresh rosemary, destalked
- 1 generous handful fresh parsley, chopped
- 1 tbsp chia seeds
- 1 tbsp nutritional yeast
- 1 tbsp black pepper, coarse ground
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil, for brushing and frying
- Aged balsamic vinegar, to serve (failing this, make a balsamic vinegar reduction and use that; it should have a thicker texture but still taste acidic and not too sweet; the thickness should come from the higher concentration of grape must and its natural sugars; no need to add sugar)
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400°F / 200°C.
2) Brush the cut sides of the squash with olive oil; sprinkle with a pinch of MSG/salt and a little black pepper (grind it directly over the squash if you are using a grinder; hold the grinder high though so that it distributes evenly—waiters in restaurants aren’t just being dramatic when they do that with pepper or Parmesan or such)
3) Arrange them cut-sides-down on a baking tray lined with baking paper, and roast for at least 30 minutes or until tender.
4) While that is roasting, add the chia seeds to the wild rice, and cook them in the low-sodium vegetable stock, using a rice cooker if available. It should take about the same length of time, but if the rice is done first, set it aside, and if the squash is done first, turn the oven down low to keep it warm.
5) Heat some oil in a sauté pan (not a skillet without high sides; we’re going to need space in a bit), and fry the chopped onion until translucent and soft. We could say “about 5 minutes” but honestly it depends on your pan as well as the heat and other factors.
6) Add the seasonings (herbs, garlic, black pepper, MSG/salt, nooch), and cook for a further 2 minutes, stirring thoroughly to distribute evenly.
7) Add the rice, berries, and nuts, cooking for a further 2 minutes, stirring constantly, ensuring everything is heated evenly.
8) Remove the squash halves from the oven, turn them over, and spoon the mixture we just made into them, filling generously.
9) Drizzle a lashing of the aged balsamic vinegar (or balsamic vinegar reduction), to serve.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Brown Rice vs Wild Rice – Which is Healthier?
- Why You Should Diversify Your Nuts!
- Goji Berries: Which Benefits Do They Really Have?
- Chia: The Tiniest Seeds With The Most Value
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- 10 Ways To Balance Blood Sugars
Take care!
Share This Post
Related Posts
-
If You’re Poor, Fertility Treatment Can Be Out of Reach
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mary Delgado’s first pregnancy went according to plan, but when she tried to get pregnant again seven years later, nothing happened. After 10 months, Delgado, now 34, and her partner, Joaquin Rodriguez, went to see an OB-GYN. Tests showed she had endometriosis, which was interfering with conception. Delgado’s only option, the doctor said, was in vitro fertilization.
“When she told me that, she broke me inside,” Delgado said, “because I knew it was so expensive.”
Delgado, who lives in New York City, is enrolled in Medicaid, the federal-state health program for low-income and disabled people. The roughly $20,000 price tag for a round of IVF would be a financial stretch for lots of people, but for someone on Medicaid — for which the maximum annual income for a two-person household in New York is just over $26,000 — the treatment can be unattainable.
Expansions of work-based insurance plans to cover fertility treatments, including free egg freezing and unlimited IVF cycles, are often touted by large companies as a boon for their employees. But people with lower incomes, often minorities, are more likely to be covered by Medicaid or skimpier commercial plans with no such coverage. That raises the question of whether medical assistance to create a family is only for the well-to-do or people with generous benefit packages.
“In American health care, they don’t want the poor people to reproduce,” Delgado said. She was caring full-time for their son, who was born with a rare genetic disorder that required several surgeries before he was 5. Her partner, who works for a company that maintains the city’s yellow cabs, has an individual plan through the state insurance marketplace, but it does not include fertility coverage.
Some medical experts whose patients have faced these issues say they can understand why people in Delgado’s situation think the system is stacked against them.
“It feels a little like that,” said Elizabeth Ginsburg, a professor of obstetrics and gynecology at Harvard Medical School who is president-elect of the American Society for Reproductive Medicine, a research and advocacy group.
Whether or not it’s intended, many say the inequity reflects poorly on the U.S.
“This is really sort of standing out as a sore thumb in a nation that would like to claim that it cares for the less fortunate and it seeks to do anything it can for them,” said Eli Adashi, a professor of medical science at Brown University and former president of the Society for Reproductive Endocrinologists.
Yet efforts to add coverage for fertility care to Medicaid face a lot of pushback, Ginsburg said.
Over the years, Barbara Collura, president and CEO of the advocacy group Resolve: The National Infertility Association, has heard many explanations for why it doesn’t make sense to cover fertility treatment for Medicaid recipients. Legislators have asked, “If they can’t pay for fertility treatment, do they have any idea how much it costs to raise a child?” she said.
“So right there, as a country we’re making judgments about who gets to have children,” Collura said.
The legacy of the eugenics movement of the early 20th century, when states passed laws that permitted poor, nonwhite, and disabled people to be sterilized against their will, lingers as well.
“As a reproductive justice person, I believe it’s a human right to have a child, and it’s a larger ethical issue to provide support,” said Regina Davis Moss, president and CEO of In Our Own Voice: National Black Women’s Reproductive Justice Agenda, an advocacy group.
But such coverage decisions — especially when the health care safety net is involved — sometimes require difficult choices, because resources are limited.
Even if state Medicaid programs wanted to cover fertility treatment, for instance, they would have to weigh the benefit against investing in other types of care, including maternity care, said Kate McEvoy, executive director of the National Association of Medicaid Directors. “There is a recognition about the primacy and urgency of maternity care,” she said.
Medicaid pays for about 40% of births in the United States. And since 2022, 46 states and the District of Columbia have elected to extend Medicaid postpartum coverage to 12 months, up from 60 days.
Fertility problems are relatively common, affecting roughly 10% of women and men of childbearing age, according to the National Institute of Child Health and Human Development.
Traditionally, a couple is considered infertile if they’ve been trying to get pregnant unsuccessfully for 12 months. Last year, the ASRM broadened the definition of infertility to incorporate would-be parents beyond heterosexual couples, including people who can’t get pregnant for medical, sexual, or other reasons, as well as those who need medical interventions such as donor eggs or sperm to get pregnant.
The World Health Organization defined infertility as a disease of the reproductive system characterized by failing to get pregnant after a year of unprotected intercourse. It terms the high cost of fertility treatment a major equity issue and has called for better policies and public financing to improve access.
No matter how the condition is defined, private health plans often decline to cover fertility treatments because they don’t consider them “medically necessary.” Twenty states and Washington, D.C., have laws requiring health plans to provide some fertility coverage, but those laws vary greatly and apply only to companies whose plans are regulated by the state.
In recent years, many companies have begun offering fertility treatment in a bid to recruit and retain top-notch talent. In 2023, 45% of companies with 500 or more workers covered IVF and/or drug therapy, according to the benefits consultant Mercer.
But that doesn’t help people on Medicaid. Only two states’ Medicaid programs provide any fertility treatment: New York covers some oral ovulation-enhancing medications, and Illinois covers costs for fertility preservation, to freeze the eggs or sperm of people who need medical treatment that will likely make them infertile, such as for cancer. Several other states also are considering adding fertility preservation services.
In Delgado’s case, Medicaid covered the tests to diagnose her endometriosis, but nothing more. She was searching the internet for fertility treatment options when she came upon a clinic group called CNY Fertility that seemed significantly less expensive than other clinics, and also offered in-house financing. Based in Syracuse, New York, the company has a handful of clinics in upstate New York cities and four other U.S. locations.
Though Delgado and her partner had to travel more than 300 miles round trip to Albany for the procedures, the savings made it worthwhile. They were able do an entire IVF cycle, including medications, egg retrieval, genetic testing, and transferring the egg to her uterus, for $14,000. To pay for it, they took $7,000 of the cash they’d been saving to buy a home and financed the other half through the fertility clinic.
She got pregnant on the first try, and their daughter, Emiliana, is now almost a year old.
Delgado doesn’t resent people with more resources or better insurance coverage, but she wishes the system were more equitable.
“I have a medical problem,” she said. “It’s not like I did IVF because I wanted to choose the gender.”
One reason CNY is less expensive than other clinics is simply that the privately owned company chooses to charge less, said William Kiltz, its vice president of marketing and business development. Since the company’s beginning in 1997, it has become a large practice with a large volume of IVF cycles, which helps keep prices low.
At this point, more than half its clients come from out of state, and many earn significantly less than a typical patient at another clinic. Twenty percent earn less than $50,000, and “we treat a good number who are on Medicaid,” Kiltz said.
Now that their son, Joaquin, is settled in a good school, Delgado has started working for an agency that provides home health services. After putting in 30 hours a week for 90 days, she’ll be eligible for health insurance.
One of the benefits: fertility coverage.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Mimosa For Healing Your Body & Mind
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Today we’re looking at mimosa (no relation to the cocktail!), which is a name given to several related plant species that belong to the same genus or general clade, look similar, and have similar properties and behavior.
As a point of interest that’s not useful: mimosa is one of those plants whereby if you touch it, it’ll retract its leaves and shrink away from you. The leaves also droop at nighttime (perfectly healthily; they’re not wilting or anything; this too is just plant movement), and spring back up in the daytime.
So that’s what we mean when we say “and behavior” 😉
Antidepressant & anxiolytic
Mimosa bark and leaves have long been used in Traditional Chinese Medicine, as well as (albeit different species) in the North-East of Brazil, and (again, sometimes different species) in Mexico.
Animal studies, in vivo studies, and clinical practice in humans, have found this to be effective, for example:
❝[Mimosa pudica extract] has anti-anxiety, anti-depressant and memory enhancing activities that are mediated through multiple mechanisms❞
Source: Effects of Mimosa pudica L. leaves extract on anxiety, depression and memory
Research is ongoing with regard to how, exactly, mimosa does what it does. Here’s a paper about another species mimosa:
(notwithstanding the genus name, it’s still part of the mimosa clade)
Anti-inflammatory & analgesic
In this case, mimosa has traditionally been used as a topical tincture (for skin damage of many kinds, ranging from cuts and abrasions to burns to autoimmune conditions and more), so what does the science say about that?
❝In summary, the present study provided evidence that the [mimosa extract], its fractions and the isolated compound sakuranetin showed significant anti-inflammatory and antinociceptive activities❞
Wound healing
About those various skin damages, here’s another application, and a study showing that it doesn’t just make it feel better, it actually helps it to heal, too:
❝Therapeutic effectiveness occurred in all patients of the extract group; after the 8th treatment week, ulcer size was reduced by 92% as mean value in this group, whereas therapeutic effectiveness was observed only in one patient of the control group (chi(2), p=0.0001). No side effects were observed in any patient in either group.❞
Very compelling stats!
Read more: Therapeutic effectiveness of a Mimosa tenuiflora cortex extract in venous leg ulceration treatment
Is it safe?
Yes, for most people, with some caveats:
- this one comes with a clear “don’t take if pregnant or breastfeeding” warning, as for unknown reasons it has caused a high incidence of fetal abnormalities or fetal death in animal studies.
- while the stem bark (the kind used in most mimosa supplements and most readily found online) has negligible psychoactivity, as do many species of mimosa in general, the root of M. tenuiflora has psychedelic effects similar to ayahuasca if taken orally, for example as a decoction, if in the presence of a monoamine oxidase inhibitor (MAOI), as otherwise MAO would metabolize the psychoactive component in the gut before it can enter the bloodstream.
That’s several “ifs”, meaning that the chances of unwanted psychedelic effects are slim if you’re paying attention, but as ever, do check with your doctor/pharmacist to be sure.
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Five Advance Warnings of Multiple Sclerosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Five Advance Warnings of Multiple Sclerosis
First things first, a quick check-in with regard to how much you know about multiple sclerosis (MS):
- Do you know what causes it?
- Do you know how it happens?
- Do you know how it can be fixed?
If your answer to the above questions is “no”, then take solace in the fact that modern science doesn’t know either.
What we do know is that it’s an autoimmune condition, and that it results in the degradation of myelin, the “insulator” of nerves, in the central nervous system.
- How exactly this is brought about remains unclear, though there are several leading hypotheses including autoimmune attack of myelin itself, or disruption to the production of myelin.
- Treatments look to reduce/mitigate inflammation, and/or treat other symptoms (which are many and various) on an as-needed basis.
If you’re wondering about the prognosis after diagnosis, the scientific consensus on that is also “we don’t know”:
Read: Personalized medicine in multiple sclerosis: hope or reality?
this paper, like every other one we considered putting in that spot, concludes with basically begging for research to be done to identify biomarkers in a useful fashion that could help classify many distinct forms of MS, rather than the current “you have MS, but who knows what that will mean for you personally because it’s so varied” approach.
The Five Advance Warning Signs
Something we do know! First, we’ll quote directly the researchers’ conclusion:
❝We identified 5 health conditions associated with subsequent MS diagnosis, which may be considered not only prodromal but also early-stage symptoms.
However, these health conditions overlap with prodrome of two other autoimmune diseases, hence they lack specificity to MS.❞
So, these things are a warning, five alarm bells, but not necessarily diagnostic criteria.
Without further ado, the five things are:
- depression
- sexual disorders
- constipation
- cystitis
- urinary tract infections
❝This association was sufficiently robust at the statistical level for us to state that these are early clinical warning signs, probably related to damage to the nervous system, in patients who will later be diagnosed with multiple sclerosis.
The overrepresentation of these symptoms persisted and even increased over the five years after diagnosis.❞
Read the paper for yourself:
Hot off the press! Published only yesterday!
Want to know more about MS?
Here’s a very comprehensive guide:
National clinical guideline for diagnosis and management of multiple sclerosis
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: