The AFib Cure – by Dr. John Day & Dr. Jared Bunch
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The authors—cardiologists and AFib specialists—make the case that if you have atrial fibrillation, you do in fact have more options than “take these pills and suffer”.
To be clear: they’re not anti-medication per se and they also acknowledge that for some people the meds may still have their place (safety first, and all), but they do fall on the side of “it would be nice to not have to, if possible, so let’s see what we can do”.
Rather, they recommend lifestyle adjustments (no surprises there), and certain biomarker optimizations (this is where it gets more in-depth), which have a good record of reducing symptoms to the point of remission and freedom from medications.
The book is first a primer on the topic of AFib, and then a how-to manual of fixing the problems that you now understand, by biomarker monitoring, lifestyle optimization, and if those things don’t work, ablative therapy which they argue is safer, easier, and more successful than you might think.
The style is clear and easy to understand, with frequent scholarly citations throughout. On the downside, the tone can sometimes be a little on the pushy side for this reviewer’s tastes, but if one overlooks that, it doesn’t detract from the useful content.
Bottom line: if you or a loved one have AFib and would like more treatment/management options than have hitherto been presented, this book will give you that.
Click here to check out The AFib Cure, and look after your heart!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tribulus Terrestris For Testosterone?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
(Clinical) Trials and Tribul-ations
In the category of supplements that have enjoyed use as aphrodisiacs, Tribulus terrestris (also called caltrop, goat’s head, gokshura, or puncture vine) has a long history, having seen wide use in both Traditional Chinese Medicine and in Ayurveda.
It’s been used for other purposes too, and has been considered a “general wellness” plant.
So, what does the science say?
Good news: very conclusive evidence!
Bad news: the conclusion is not favorable…
Scientists are known for their careful use of clinical language, and it’s very rare for a study/review to claim something as proven (scientists leave journalists to do that part), and in this case, when it comes to Tribulus’s usefulness as a testosterone-enhancing libido-boosting supplement…
❝analysis of empirical evidence from a comprehensive review of available literature proved this hypothesis wrong❞
Strong words! You can read it in full here; they do make some concessions along the way (e.g. mentioning unclear or contradictory findings, suggesting that it may have some effect, but by an as-yet unknown mechanism if it does—although some potential effect on nitric oxide levels has been hypothesized, which is reasonable if so, as NO does feature in arousal-signalling), but the general conclusion is “no, this doesn’t have androgen-enhancing properties”:
Pro-sexual and androgen enhancing effects of Tribulus terrestris L.: Fact or Fiction
That’s a review though, what about taking a look at a representative RCT? Here we go:
❝Tribulus terrestris was not more effective than placebo on improving symptoms of erectile dysfunction or serum total testosterone❞
As a performance-enhancer in sport
We’ll be brief here: it doesn’t seem to work and it may not be safe:
Insights into Supplements with Tribulus Terrestris used by Athletes
From sport, into general wellness?
Finally, a study that finds it may be useful for something!
❝Overall, participants supplemented with TT displayed significant improvements in lipid profile. Inflammatory and hematological biomarkers showed moderate beneficial effects with no significant changes on renal biomarkers. No positive effects were observed on the immune system response. Additionally, no TT-induced toxicity was reported.
In conclusion, there was no clear evidence of the beneficial effects of TT supplementation on muscle damage markers and hormonal behavior.❞
About those lipids…
Animal studies have shown that it may not only improve lipid profiles, but also may partially repair the endothelial dysfunction resulting from hyperlipidemia:
Want to try some?
In the unlikely event that today’s research review has inspired you with an urge to try Tribulus terrestris, here’s an example product on Amazon
If on the other hand you’d like to actually increase testosterone levels, then we suggest:
Topping Up Testosterone? ← a previous main feature did earlier this year
Take care!
Share This Post
-
Hate salad or veggies? Just keep eating them. Here’s how our tastebuds adapt to what we eat
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Do you hate salad? It’s OK if you do, there are plenty of foods in the world, and lots of different ways to prepare them.
But given almost all of us don’t eat enough vegetables, even though most of us (81%) know eating more vegetables is a simple way to improve our health, you might want to try.
If this idea makes you miserable, fear not, with time and a little effort you can make friends with salad.
Why don’t I like salads?
It’s an unfortunate quirk of evolution that vegetables are so good for us but they aren’t all immediately tasty to all of us. We have evolved to enjoy the sweet or umami (savoury) taste of higher energy foods, because starvation is a more immediate risk than long-term health.
Vegetables aren’t particularly high energy but they are jam-packed with dietary fibre, vitamins and minerals, and health-promoting compounds called bioactives.
Those bioactives are part of the reason vegetables taste bitter. Plant bioactives, also called phytonutrients, are made by plants to protect themselves against environmental stress and predators. The very things that make plant foods bitter, are the things that make them good for us.
Unfortunately, bitter taste evolved to protect us from poisons, and possibly from over-eating one single plant food. So in a way, plant foods can taste like poison.
For some of us, this bitter sensing is particularly acute, and for others it isn’t so bad. This is partly due to our genes. Humans have at least 25 different receptors that detect bitterness, and we each have our own genetic combinations. So some people really, really taste some bitter compounds while others can barely detect them.
This means we don’t all have the same starting point when it comes to interacting with salads and veggies. So be patient with yourself. But the steps toward learning to like salads and veggies are the same regardless of your starting point.
It takes time
We can train our tastes because our genes and our receptors aren’t the end of the story. Repeat exposures to bitter foods can help us adapt over time. Repeat exposures help our brain learn that bitter vegetables aren’t posions.
And as we change what we eat, the enzymes and other proteins in our saliva change too. This changes how different compounds in food are broken down and detected by our taste buds. How exactly this works isn’t clear, but it’s similar to other behavioural cognitive training.
Add masking ingredients
The good news is we can use lots of great strategies to mask the bitterness of vegetables, and this positively reinforces our taste training.
Salt and fat can reduce the perception of bitterness, so adding seasoning and dressing can help make salads taste better instantly. You are probably thinking, “but don’t we need to reduce our salt and fat intake?” – yes, but you will get more nutritional bang-for-buck by reducing those in discretionary foods like cakes, biscuits, chips and desserts, not by trying to avoid them with your vegetables.
Adding heat with chillies or pepper can also help by acting as a decoy to the bitterness. Adding fruits to salads adds sweetness and juiciness, this can help improve the overall flavour and texture balance, increasing enjoyment.
Pairing foods you are learning to like with foods you already like can also help.
The options for salads are almost endless, if you don’t like the standard garden salad you were raised on, that’s OK, keep experimenting.
Experimenting with texture (for example chopping vegetables smaller or chunkier) can also help in finding your salad loves.
Challenge your biases
Challenging your biases can also help the salad situation. A phenomenon called the “unhealthy-tasty intuition” makes us assume tasty foods aren’t good for us, and that healthy foods will taste bad. Shaking that assumption off can help you enjoy your vegetables more.
When researchers labelled vegetables with taste-focused labels, priming subjects for an enjoyable taste, they were more likely to enjoy them compared to when they were told how healthy they were.
The bottom line
Vegetables are good for us, but we need to be patient and kind with ourselves when we start trying to eat more.
Try working with biology and brain, and not against them.
And hold back from judging yourself or other people if they don’t like the salads you do. We are all on a different point of our taste-training journey.
Emma Beckett, Senior Lecturer (Food Science and Human Nutrition), School of Environmental and Life Sciences, University of Newcastle
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Protein vs Sarcopenia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Protein vs Sarcopenia
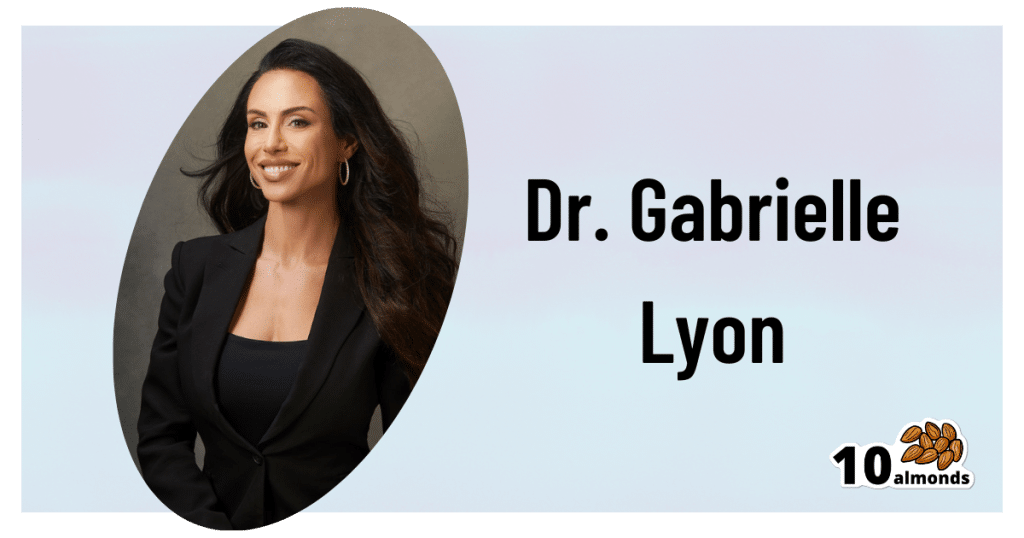
This is Dr. Gabrielle Lyon. A medical doctor, she’s board-certified in family medicine, and has also engaged in research and clinical practice in the fields of geriatrics and nutritional sciences.
A quick note…
We’re going to be talking a bit about protein metabolism today, and it’s worth noting that Dr. Lyon personally is vehemently against vegetarianism/veganism, and considers red meat to be healthy.
Scientific consensus on the other hand, holds that vegetarianism and veganism are fine for most people if pursued in an informed and mindful fashion, that white meat and fish are also fine for most people, and red meat is simply not.
If you’d like a recap on the science of any of that:
- Protein: How Much Do We Need, Really?
- Plant vs Animal Protein: Diversity is Key
- Do We Need Animal Products to be Healthy?
Nevertheless, if we look at the science that she provides, the advice is sound when applied to protein in general and without an undue focus on red meat.
How much protein is enough?
In our article linked above, we gave 1–2g/kg/day
Dr. Lyons gives the more specific 1.6g/kg/day for adults older than 40 (this is where sarcopenia often begins!) and laments that many sources offer 0.8g/kg.
To be clear, that “per kilogram” means per kilogram of your bodyweight. For Americans, this means dividing lbs by 2.2 to get the kg figure.
Why so much protein?
Protein is needed to rebuild not just our muscles, but also our bones, joint tissues, and various other parts of us:
We Are Such Stuff As Fish Are Made Of
Additionally, our muscles themselves are important for far more than just moving us (and other things) around.
As Dr. Lyon explains: sarcopenia, the (usually age-related) loss of muscle mass, does more than just make us frail; it also messes up our metabolism, which in turn messes up… Everything else, really. Because everything depends on that.
This is because our muscles themselves use a lot of our energy, and/but also store energy as glycogen, so having less of them means:
- getting a slower metabolism
- the energy that can’t be stored in muscle tissue gets stored somewhere else (like the liver, and/or visceral fat)
So, while for example the correlation between maintaining strong muscles and avoiding non-alcoholic fatty liver disease may not be immediately obvious, it is clear when one follows the metabolic trail to its inevitable conclusion.
Same goes for avoiding diabetes, heart disease, and suchlike, though those things are a little more intuitive.
How can we get so much protein?
It can seem daunting at first to get so much protein if you’re not used to it, especially as protein is an appetite suppressant, so you’ll feel full sooner.
It can especially seem daunting to get so much protein if you’re trying to avoid too many carbs, and here’s where Dr. Lyon’s anti-vegetarianism does have a point: it’s harder to get lean protein without meat/fish.
That said, “harder” does not mean “impossible” and even she acknowledges that lentils are great for this.
If you’re not vegetarian or vegan, collagen supplementation is a good way to make up any shortfall, by the way.
And for everyone, there are protein supplements available if we want them (usually based on whey protein or soy protein)
Anything else we need to do?
Yes! Eating protein means nothing if you don’t do any resistance work to build and maintain muscle. This can take various forms, and Dr. Lyon recommends lifting weights and/or doing bodyweight resistance training (calisthenics, Pilates, etc).
Here are some previous articles of ours, consistent with the above:
- Resistance Is Useful! (Especially As We Get Older)
- Overdone It? How To Speed Up Recovery After Exercise
- How To Do HIIT (Without Wrecking Your Body)
- Exercises To Do (And Ones To Avoid) If You Have Osteoporosis
Take care!
Share This Post
Related Posts
-
Don’t Do *This* If You’re Over 50 (And Want Better Sleep)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Michael Breus, sleep specialist, explains:
Don’t make these mistakes
Dr. Breus recommends avoiding…
- Misusing magnesium: magnesium is a helpful sleep aid but must be carefully monitored. Recommended doses are 250mg for women and 300–350 mg for men, with slight adjustments for hot climates or active lifestyles. Overdosing can cause stomach issues, diarrhea, and dehydration, disrupting sleep. He recommends starting with magnesium glycinate for fewer stomach issues, and later mix with magnesium citrate. Always check supplements to avoid excessive magnesium intake.
- Misusing melatonin: melatonin production declines after age 55–60, making low-dose supplementation (0.5–1 mg) beneficial. He recommends, however, avoiding high doses (3–10mg), and he recommends to take it 90 minutes before bedtime. Melatonin interacts with some medications (including some meds for blood pressure or depression), so consult a pharmacist before use to avoid risks like serotonin syndrome.
- Going to bed too early: going to bed too early disrupts circadian rhythms and reduces sleep drive, causing earlier waking. Now, being an “early bird” is a generally healthy thing, but if you’re already getting up at 5am, say, you probably want your schedule to not continue to creep further forwards until you become nocturnal. Set a consistent wake-up time and count 7.5 hours backward (plus a set time to fall asleep, e.g. 20 minutes, but you’ll know what it is for you) to determine bedtime.
- Excessive caffeine consumption: from the heading, it may seem like a no-brainer, but older adults metabolize caffeine 33% slower on average, prolonging its effects. Dr. Breus recommends to reduce intake with “caffeine fading,” switching to half-caffeinated coffee for a while and then considering transitioning to decaf. He also suggests enjoying increasingly lower-caffeine teas, like black tea in the morning, matcha in the afternoon, and herbal tea at night to reduce caffeine’s impact on sleep.
- Falling foul of serotonin: avoid taking 5-HTP supplements with SSRI antidepressants like Prozac or Zoloft due to the risk of serotonin syndrome.
- Consider checking for physical problems: if you regularly wake up tired and/or groggy (despite having ostensibly had enough sleep, and there not being a pharmaceutical explanation for your grogginess), consider screening for sleep apnea. Home sleep tests are a convenient way to identify and treat this common but often undiagnosed condition.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
How to Fall Asleep Faster: CBT-Insomnia Treatment
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Knitting helps Tom Daley switch off. Its mental health benefits are not just for Olympians
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Olympian Tom Daley is the most decorated diver in Britain’s history. He is also an avid knitter. At the Paris 2024 Olympics Daley added a fifth medal to his collection – and caught the world’s attention knitting a bright blue “Paris 24” jumper while travelling to the games and in the stands.
At the Tokyo Olympics, where Daley was first spotted knitting, he explained its positive impact on his mental health.
It just turned into my mindfulness, my meditation, my calm and my way to escape the stresses of everyday life and, in particular, going to an Olympics.
The mental health benefits of knitting are well established. So why is someone famous like Daley knitting in public still so surprising?
Africa Voice/Shutterstock Knitting is gendered
Knitting is usually associated with women – especially older women – as a hobby done at home. In a large international survey of knitting, 99% of respondents identified as female.
But the history of yarn crafts and gender is more tangled. In Europe in the middle ages, knitting guilds were exclusive and reserved for men. They were part of a respected Europe-wide trade addressing a demand for knitted products that could not be satisfied by domestic workers alone.
The industrial revolution made the production of clothed goods cheaper and faster than hand-knitting. Knitting and other needle crafts became a leisure activity for women, done in the private sphere of the home.
World Wars I and II turned the spotlight back on knitting as a “patriotic duty”, but it was still largely taken up by women.
During COVID lockdowns, knitting saw another resurgence. But knitting still most often makes headlines when men – especially famous men like Daley or actor Ryan Gosling – do it.
Men who knit are often seen as subverting the stereotype it’s an activity for older women.
Knitting the stress away
Knitting can produce a sense of pride and accomplishment. But for an elite sportsperson like Daley – whose accomplishments already include four gold medals and one silver – its benefits lie elsewhere.
Olympics-level sport relies on perfect scores and world records. When it comes to knitting, many of the mental health benefits are associated with the process, rather than the end result.
Daley says knitting is the “one thing” that allows him to switch off completely, describing it as “my therapy”. https://www.youtube.com/embed/6wwXGOki–c?wmode=transparent&start=0
The Olympian says he could
knit for hours on end, honestly. There’s something that’s so satisfying to me about just having that rhythm and that little “click-clack” of the knitting needles. There is not a day that goes by where I don’t knit.
Knitting can create a “flow” state through rhythmic, repetitive movements of the yarn and needle. Flow offers us a balance between challenge, accessibility and a sense of control.
It’s been shown to have benefits relieving stress in high-pressure jobs beyond elite sport. Among surgeons, knitting has been found to improve wellbeing as well as manual dexterity, crucial to their role.
For other health professionals – including oncology nurses and mental health workers – knitting has helped to reduce “compassion fatigue” and burnout. Participants described the soothing noise of their knitting needles. They developed and strengthened team bonds through collective knitting practices. https://www.youtube.com/embed/dTTJjD_q2Ik?wmode=transparent&start=0 A Swiss psychiatrist says for those with trauma, knitting yarn can be like “knitting the two halves” of the brain “back together”.
Another study showed knitting in primary school may boost children’s executive function. That includes the ability to pay attention, remember relevant details and block out distractions.
As a regular creative practice, it has also been used in the treatment of grief, depression and subduing intrusive thoughts, as well countering chronic pain and cognitive decline.
Knitting is a community
The evidence for the benefits of knitting is often based on self-reporting. These studies tend to produce consistent results and involve large population samples.
This may point to another benefit of knitting: its social aspect.
Knitting and other yarn crafts can be done alone, and usually require simple materials. But they also provide a chance to socialise by bringing people together around a common interest, which can help reduce loneliness.
The free needle craft database and social network Ravelry contains more than one million patterns, contributed by users. “Yarn bombing” projects aim to engage the community and beautify public places by covering objects such as benches and stop signs with wool.
The interest in Daley’s knitting online videos have formed a community of their own.
In them he shows the process of making the jumper, not just the finished product. That includes where he “went wrong” and had to unwind his work.
His pride in the finished product – a little bit wonky, but “made with love” – can be a refreshing antidote to the flawless achievements often on display at the Olympics.
Michelle O’Shea, Senior Lecturer, School of Business, Western Sydney University and Gabrielle Weidemann, Associate Professor in Psychological Science, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dangers Of Root Canals And Crowns, & What To Do Instead
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Michelle Jorgensen, a dentist, tells us that it’s a lot rarer than people think to actually need a crown or a root canal; there are ways of avoiding such:
The tooth, the whole tooth, and nothing but the tooth?
First, some of the problems with the treatments that are most popular, especially in the US:
Problems with root canals:
- Involves cleaning and filling the tooth’s main canal but leaves microtubules that can harbor dead tissue and attract bacteria.
- This can lead to infections, often undetected for a long time due to the nerve removal, potentially harming overall health and weakening the tooth.
- Root canals often result in brittle teeth that can break, necessitating crowns.
And then…
Problems with crowns:
- A crown requires significant removal of tooth structure (up to 1.5 mm of enamel), making the tooth more vulnerable and sensitive.
- Crowns can also lead to new cavities underneath due to weak bonding to dentin.
- The cycle often leads from a healthy tooth to fillings, crowns, root canals, and eventual extraction (and then, perhaps, an implant in its place). That’s great for the dentist, but not so great for you.
Biomimetic dentistry the exciting name currently being used for what has been more prosaically called “conservative restorative dentistry”, which in turn has also been known by other names in recent decades, and its goal is to strengthen and preserve natural teeth as much as possible.
Methods it uses:
- Treats affected but still living teeth with non-invasive procedures.
- Uses ozone treatment to kill bacteria in deep cavities, avoiding direct nerve exposure.
- Applies conservative partial restorations like onlays instead of full crowns.
Benefits of this approach:
- Preserves enamel, minimizes trauma, and reduces the risk of tooth death.
- Maintains long-term tooth structure and health.
- 95% success rate in saving affected teeth without resorting to root canals.
In short, Dr. Jorgensen says that 60–80% of traditional crowns and root canals can be avoided. Which is surely a good thing.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Tooth Remineralization: How To Heal Your Teeth Naturally
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: