The 7 Known Risk Factors For Dementia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A recent UK-based survey found that…
- while nearly half of adults say dementia is the disease they fear most,
- only a third of those thought you could do anything to avoid it, and
- just 1% could name the 7 known risk factors.
Quick test
Can you name the 7 known risk factors?
Please take a moment to actually try (this kind of mental stimulation is good in any case), and count them out on your fingers (or write them down), and then…
Answer (no peeking if you haven’t listed them yet)
The 7 known risk factors are:
*drumroll please*
- Smoking
- High blood pressure
- Diabetes
- Obesity
- Depression
- Lack of mental stimulation
- Lack of physical activity
How many did you get? If you got them all, well done. If not, then well, now you know, so that’s good.
Did you come here from our “Future-Proof Your Brain” article? If so, you can get back to it here ← and if you didn’t, you should check it out anyway; it’s worth it😉
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hummus vs Guacamole – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing hummus to guacamole, we picked the guacamole.
Why?
First up, let’s assume that the standards are comparable, for example that both have been made with simple whole foods. The hummus is mostly chickpeas with tahini and a little olive oil and some seasoning; the guacamole is mostly avocado with a little lime juice and some seasoning.
In terms of macronutrients, hummus has slightly more protein and fiber, 2x the carbohydrates (but they are healthy carbs), and usually slightly less fat (but the fats are healthy in both cases).
In terms of micronutrients, the hummus is rich in iron and B vitamins, and the guacamole is rich in potassium, magnesium, vitamins C, E, and K.
So far, it’s pretty much tied. What else is there to consider?
We picked the guacamole because some of its nutrients (especially the potassium, magnesium, and vitamin K) are more common deficiencies in most people’s diets than iron and B vitamins. So, on average, it’s probably the one with the nutrients that you need more of at any given time.
So, it was very very close, and it came down to the above as the deciding factor.
However!
- If you like one and not the other? Eat that one; it’s good.
- If you like both but feel like eating one of them in particular? Eat that one; your body is probably needing those nutrients more right now.
- If you are catering for a group of people? Serve both!
- If you are catering for just yourself and would enjoy both? Serve both! There’s nobody to stop you!
Want to read more?
You might like: Avocado Oil vs Olive Oil – Which is Healthier?
Enjoy!
Share This Post
-
Build Strong Feet: Exercises To Strengthen Your Foot & Ankle
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot depends on the health of our feet, especially when it comes to their strength and stability. But they often get quite neglected, when it comes to maintenance. Here’s how to help your feet keep the rest of your body in good condition:
On a good footing
The foot-specific exercises recommended here include:
- Active toe flexion/extension: curl and extend your toes
- Active toe adduction/abduction: use a towel for feedback this time as you spread your toes
- “Short foot” exercise: create an arch by bringing the base of your big toe towards your heel
- Resisted big toe flexion: use resistance bands; flex your big toe while controlling the others.
- Standing big toe flexion (isometric): press your big toe against an inclined surface as forcefully as you can
- Foot bridge exercise: hold your position with the front part of your feet on an elevated surface, to strengthen the arch.
- Heel raises: which can be progressed from basic to more advanced variations, increasing difficulty
- Ankle movements: dorsiflexion, inversion, etc, to increase mobility
It’s important to also look after your general lower body strength and stability, including (for example) single-leg deadlifts, step-downs, and lunges
Balance and proprioceptive exercises are good too, such as a static or dynamic one-leg balances, progressing to doing them with your eyes closed and/or on unstable surfaces (be careful, of course, and progress to this only when confident).
For more on all of these, an explanation of the anatomy, some other exercises too, and visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Steps For Keeping Your Feet A Healthy Foundation
Take care!
Share This Post
-
What Your Mucus Says About Your Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s not a sexy topic (unless perhaps you have a fetish), but it is a useful topic to know about.
So, let’s get down to business with this much-maligned bodily fluid:
What is mucus? And why?
Sometimes, it can seem that mucus only exists to be an inconvenience, and to convey disease.
And… Actually, that’s mostly true.
While some kinds of mucus have other jobs beyond the scope of today’s article (did you know semen is mostly mucus? If not, now you do), the primary job of most of our mucus is to stop things (especially pathogens) going where they shouldn’t.
So, in essence, it really does exist to be an inconvenience—to pathogens. And to convey those pathogens to where they can be disposed of safely, either outside of the body, or to be an easy meal (what with being stuck in mucus, and thus at least moderately immobilized) for our various active immune cells. To make matters worse for the pathogens, there are (usually) enzymes in our mucus that have antimicrobial properties, too.
Some of mucus’s protective role can be in other ways too, such as by lining our stomach. You know, the stomach that contains the acid that can dissolve meat, despite us also being made of meat.
The slimiest rainbow
Ok, maybe not the slimiest rainbow—there’s probably a YouTube slime channel producing more colors. But, our noses are capable of dispensing astonishing quantities of mucus sometimes, and the color can vary widely, so here’s what we can know from that:
Clear
This is as it should be, in good health. If you’re getting lots of it but it’s clear, then it’s usually allergies, but watch out in case it changes color, heralding an infection. This “clear is how it looks when in ideal health”, by the way, is why when someone is sobbing in abject grief, any mucus that shows up to add to that picture will generally be clear.
White
As above, but now inflamed. Inflammation is usually something we don’t want, but in the case of a threat from a pathogen, we actually do want acute inflammation like this—the body is assembling its armies, of which, the most visible (when they appear in mass) are white blood cells. Because of their abundant presence at this stage, the mucus will also become thicker.
Yellow
As above, but the battle is now truly underway, and the yellow color comes from dead white blood cells. This does not, however, mean the battle is necessarily going badly—the body treats its white blood cells as very disposable fighters, and their deaths in large numbers are expected and normal when doing battle.
Green
As above, but neutrophils (a specific kind of white blood cell) have joined the party. They release an enzyme that colors the mucus green—and kills a lot of pathogens. Popular lore says that green mucus means a bacterial infection, but it’s not always so; these can be deployed against viruses too, depending on various factors beyond the scope of this article (but generally pertaining to severity). In any case, this too does not mean the battle is necessarily going badly, but it does express that your body is taking it very seriously—and you should, too.
Red
Nothing to do with infections, usually—it’s just a little blood (the red kind, this time). Usually it got into the mucus because the mucus membrane got damaged, usually due to some kind of physical trauma (e.g. very vigorous nose-blowing, poking things up the nose, etc) or sometimes if the air is very dry (then the mucus itself can dry out, and become stabby inside the nose; when more mucus is produced, it gets infused with blood from the injury).
Pink
As above, but combined with the “white” stage of infection response.
Orange
As above, but combined with the “yellow” stage of infection response.
Brown
As above, but the blood has oxidized—or, as a completely alterative possibility, it could mean you have been breathing a lot of pollutants. Smoke of various kinds (from fires, from smoking, etc) can cause this.
Black
There are various possible explanations here and all of them are bad. Get thee to a doctor. Superficial examples include:
- Fungal infection (you thought toxic black mold was bad when it was on the wall of the house, wait until it’s on the walls of your respiratory system)
- Blood, in abundance, oxidized (which begs the question of what caused that, but certainly: something wrong is not right)
- Pollutants again, but this time at absurd levels of exposure
That last one might sound very transient and self-correcting, but it’s not, and it comes with many increased short- and long-term health risks.
Want to know more?
Knowledge is power, so read up, and stay well:
- Beyond Supplements: The Real Immune-Boosters!
- The Cold Truth About Respiratory Infections
- Why Some People Get Sick More (And How To Not Be One Of Them)
Take care!
Share This Post
Related Posts
-
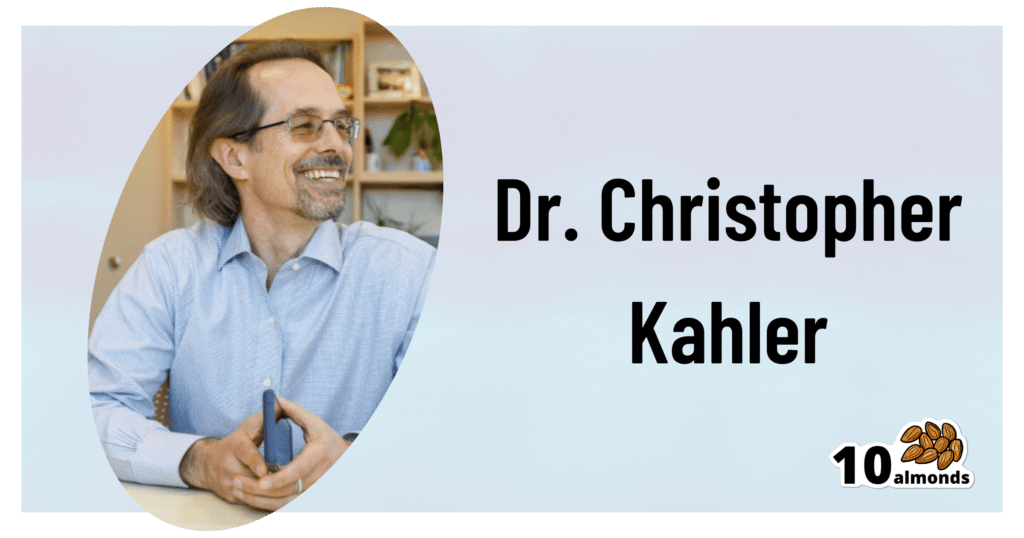
An Addiction Expert’s Insights On Festive Drinking
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Christopher Kahler. He’s Professor of Behavioral and Social Sciences, Director of Alcohol and Addiction Studies, Professor of Psychiatry and Human Behavior, all at Brown University.
What does he want us to know?
It’s the trickiest time of the year
Per stats, alcohol sales peak in December, with the heaviest drinking being from mid-December (getting an early start on the Christmas cheer) to New Year’s Eve. As for why, there’s a collection of reasons, as he notes:
❝The main challenge is there’s an extra layer of stress, with a lot of obligations and expectations from friends and family. We’re around people who maybe we’re not usually around, and in larger groups. It’s also a time of heightened emotion and, for some people, loneliness.
On top of that, alcohol use is built into a lot of our winter holiday traditions. It’s often marketed as part of the “good life.” We’re expected to have alcohol when we celebrate.❞
As for how much alcohol is safe to drink… According to the World Health Organization, the only safe amount of alcohol is zero:
Dr. Kahler acknowledges, however, that many people will wish to imbibe anyway, and indeed, he himself does drink a little, but endeavours to do so mindfully, and as such, he recommends that we…
HALT!
Dr. Kahler counsels us against making decisions (including the decision to drink alcohol), on occasions when we are one or more of the following:
- Hungry
- Angry
- Lonely
- Tired
He also notes that around this time of year, often our normal schedules and habits are disrupted, which introduces more microdecisions to our daily lives, which in turn means more “decision fatigue”, and the greater chance of making bad decisions.
We share some practical tips on how to reduce the chances of thusly erring, here:
Set your intentions now
He bids us figure out what our goal is, and really think it through, including not just “how many drinks to have” if we’re drinking, but also such things as “what feelings are likely to come up”. Because, if we’ve historically used alcohol as a maladaptive coping mechanism, we’re going to need a different, better, healthier coping mechanism (we talked more about that in our above-linked article about reducing or quitting alcohol, too, with some examples).
He also suggests that we memorize our social responses—exactly what we’re going to say if offered a drink, for example:
❝It’s important to know what you’re going to say about your alcohol use. If someone asks if they can get you a drink, good responses could be: “A glass of water would be great” or “Do you have any non-alcoholic cider?” You don’t have to explain yourself. Just ask for what you want, because saying no to someone can be difficult.❞
See also:
December’s Traps To Plan Around
Mix it up and slow it down
No, that doesn’t mean mix yourself a sloe gin cocktail. But rather, it’s about alternating alcoholic and non-alcoholic drinks, to give your body half a chance to process the alcohol, and also to rehydrate a little along the way.
We talk about this and other damage-limitation methods, here:
How To Reduce The Harm Of Festive Drinking (Without Abstaining)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Blind Spots – by Dr. Marty Makary
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From the time the US recommended not giving peanuts to infants for the first three years of life “in order to avoid peanut allergies” (whereupon non-exposure to peanuts early in life led to, instead, an increase in peanut allergies and anaphylactic incidents), to the time the US recommended not taking HRT on the strength of the claim that “HRT causes breast cancer” (whereupon the reduced popularity of HRT led to, instead, an increase in breast cancer incidence and mortality), to many other such incidents of very bad public advice being given on the strength of a single badly-misrepresented study (for each respective thing), Dr. Makary puts the spotlight on what went wrong.
This is important, because this is not just a book of outrage, exclaiming “how could this happen?!”, but rather instead, is a book of inquisition, asking “how did this happen?”, in such a way that we the reader can spot similar patterns going forwards.
Oftentimes, this is a simple matter of having a basic understanding of statistics, and checking sources to see if the dataset really supports what the headlines are claiming—and indeed, whether sometimes it suggests rather the opposite.
The style is a little on the sensationalist side, but it’s well-supported with sound arguments, good science, and clear mathematics.
Bottom line: if you’d like to improve your scientific literacy, this book is an excellent illustrative guide.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Reduce Knee Pain After Sitting
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sitting is bad for the health, and doubly so if you have arthritis, as a lack of regular movement can cause joints to “seize up”. So, what to do about it if you have to sit for an extended time?
Dr. Alyssa Kuhn, arthritis specialist, explains:
Movement remains key
The trick is to continue periodically moving, notwithstanding that you may need to remain seated. So…
- Heel slides
- Straighten and bend your leg by sliding or lifting your heel.
- Promotes blood flow and reduces fluid buildup in the knee.
- Helps lubricate the joint, making standing up easier.
- Heel lifts
- Lift your heels up and down while keeping feet on the ground.
- This one’s ideal for tight spaces, such as when riding in a car or airplane.
- Improves blood circulation and can reduce ankle swelling and leg heaviness.
Do 20–30 repetitions every now and again, to keep your joints moving.
Note: if you are a wheelchair user whose legs lack the strength and/or motor function to do this, in this case it’s the movement of the leg that counts, not where that movement originated from. So, if you use one hand to lift your leg slightly and the other to push it like a swing, that will also be sufficient to give the joint the periodic movement it needs.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Stand Up For Your Health (Or Don’t) ← our main feature on this also includes more things you can do if you must sit, to make sitting less bad!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Heel slides