When Doctors Make House Calls, Modern-Style!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
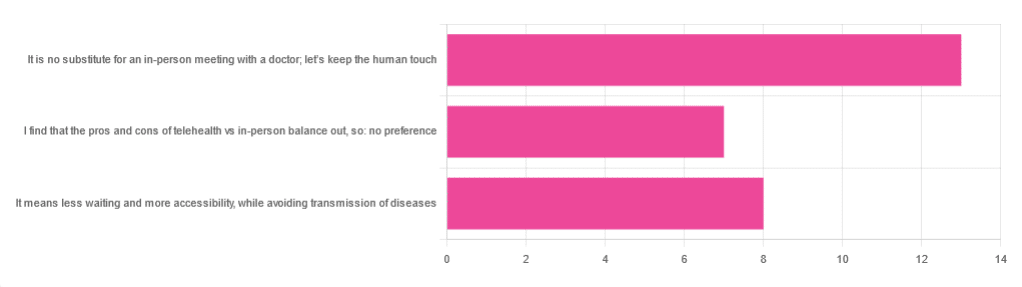
In Tuesday’s newsletter, we asked you foryour opinion of telehealth for primary care consultations*, and got the above-depicted, below-described, set of responses:
- About 46% said “It is no substitute for an in-person meeting with a doctor; let’s keep the human touch”
- About 29% said “It means less waiting and more accessibility, while avoiding transmission of diseases”
- And 25 % said “I find that the pros and cons of telehealth vs in-person balance out, so: no preference”
*We specified that by “primary care” we mean the initial consultation with a non-specialist doctor, before receiving treatment or being referred to a specialist. By “telehealth” we mean by videocall or phonecall.
So, what does the science say?
A quick note first
Because telehealth was barely a thing (statistically speaking) before the first stages of the COVID pandemic, compared to how it is now, most of the science for this is young, and a lot of the science simply hasn’t been done yet, and/or has not been published yet, because the process can take years.
Because of this, some studies we do have aren’t specifically about primary care, and are sometimes about specialists. We think this should not affect the results much, but it bears highlighting.
Nevertheless, we’ll do what we can with the science we have!
Telehealth is more accessible than in-person consultations: True or False?
True, for most people. For example…
❝Data was found from a variety of emergency and non-emergency departments of primary, secondary, and specialised healthcare.
Satisfaction was high among recipients of healthcare, scoring 9-10 on a scale of 0-10 or ranging from 73.3% to 100%.
Convenience was rated high in every specialty examined. Satisfaction of clinicians was high throughout the specialities despite connection failure and concerns about confidentiality of information.❞
whereas…
❝Nonetheless, studies reported perception of increased barriers to accessing care and inequalities for vulnerable patients especially in older people❞
~ Ibid.
Source: Satisfaction with telemedicine use during COVID-19 pandemic in the UK: a systematic review
Now, perception of those things does necessarily equate to an actual increased barrier, but it is reasonable that someone who thinks something is inaccessible will be less inclined to try to access it.
The quality of care provided via telehealth is as good as in-person: True or False?
True, ostensibly, with caveats. The caveats are:
- We’re going offreported patient satisfaction, not objective patient health outcomes (we found little* science as yet for the relative incidence of misdiagnosis, for example—which kind of thing will take time to be revealed).
- We’re also therefore speaking (as statistics do) for the significant majority of people. However, if we happen to be (statistically speaking) an insignificant minority, well, that just sucks for us personally.
*we did find some, but it wasn’t very helpful yet. For example:
An electronic trigger to detect telemedicine-related diagnostic errors
this one does look at the incidence of diagnostic errors, but provides no control group (i.e. otherwise-comparable in-person consultations) for comparison.
While most oft-considered demographic groups reported comparable patient satisfaction (per race, gender, and socioeconomic status, for example), there was one outlier variable, which was age (as we quoted from that first study above).
However!
Looking under the hood of these stats, it seems that age is not the real culprit, so much as technological illiteracy, which is heavily correlated with age:
❝Lower eHealth literacy is associated with more negative attitudes towards I/C technology in healthcare. This trend is consistent across diverse demographics and regions. ❞
Source: Meta-analysis: eHealth literacy and attitudes towards internet/computer technology
There are things that can be done at an in-person consultation that can’t be done by telehealth: True or False?
True, of course. It is incredibly rare that we will cite “common sense”, (as sometimes “common sense” is actually “common mistakes” and is simply and verifiably wrong), but in this case, as one 10almonds subscriber put it:
❝The doctor uses his five senses to assess. This cannot be attained over the phone❞
~ 10almonds subscriber
A quick note first: if your doctor is using their sense of taste to diagnose you, please get a different doctor, because they should definitely not be doing that!
Not in this century, anyway… Once upon a time, diabetes was diagnosed by urine-tasting (and yes, that was a fairly reliable method).
However, nowadays indeed a doctor will use sight, sound, touch, and sometimes even smell.
In a videocall we’re down to two of those senses (sight and sound), and in a phonecall, down to one (sound) and even that is hampered. Your doctor cannot, for example, use a stethoscope over the phone.
With this in mind, it really comes down to what you need from your doctor in that consultation.
- If you’re 99% sure that what you need is to be prescribed an antidepressant, that probably doesn’t need a full physical.
- If you’re 99% sure that what you need is a referral, chances are that’ll be fine by telehealth too.
- If your doctor is 99% sure that what you need is a verbal check-up (e.g. “How’s it been going for you, with the medication that I prescribed for you a month ago?”, then again, a call is probably fine.
If you have a worrying lump, or an unhappy bodily discharge, or an unexplained mysterious pain? These things, more likely an in-person check-up is in order.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
In Plain English…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Time!
This is the bit whereby each week, we respond to subscriber questions/requests/etc
Have something you’d like to ask us, or ask us to look into? Hit reply to any of our emails, or use the feedback widget at the bottom, and a Real Human™ will be glad to read it!
Q: Love to have someone research all the additives in our medicines, (risk of birth control and breast cancer) and what goes in all of our food and beverages. So much info out there, but there are so many variations, you never know who to believe.
That’s a great idea! There are a lot of medicines and food and beverages out there, so that’s quite a broad brief, but! We could well do a breakdown of very common additives, and demystify them, sorting them into good/bad/neutral, e.g:
- Ascorbic acid—Good! This is Vitamin C
- Acetic acid—Neutral! This is vinegar
- Acetylsalicylic acid—Good or Bad! This is aspirin (a painkiller and blood-thinning agent, can be good for you or can cause more problems than it solves, depending on your personal medical situation. If in doubt, check with your doctor)
- Acesulfame K—Generally Neutral! This is a sweetener that the body can’t metabolize, so it’s also not a source of potassium (despite containing potassium) and will generally do nothing. Unless you have an allergy to it, which is rare but is a thing.
- Sucralose—Neutral! This is technically a sugar (as is anything ending in -ose), but the body can’t metabolize it and processes it as a dietary fiber instead. We’d list it as good for that reason, but honestly, we doubt you’re eating enough sucralose to make a noticeable difference to your daily fiber intake.
- Sucrose—Bad! This is just plain sugar
Sometimes words that sound the same can ring alarm bells when they need not, for example there’s a big difference between:
- Potassium iodide (a good source of potassium and iodine)
- Potassium cyanide (the famous poison; 300mg will kill you; half that dose will probably kill you)
- Cyanocobalamine (Vitamin B12)
Let us know if there are particular additives (or particular medications) you’d like us to look at!
While for legal reasons we cannot give medical advice, talking about common contraindications (e.g., it’s generally advised to not take this with that, as one will stop the other from working, etc) is definitely something we could do.
For example! St. John’s Wort, very popular as a herbal mood-brightener, is on the list of contraindications for so many medications, including:
- Antidepressants
- Birth control pills
- Cyclosporine, which prevents the body from rejecting transplanted organs
- Some heart medications, including digoxin and ivabradine
- Some HIV drugs, including indinavir and nevirapine
- Some cancer medications, including irinotecan and imatinib
- Warfarin, an anticoagulant (blood thinner)
- Certain statins, including simvastatin
Q: As I am a retired nurse, I am always interested in new medical technology and new ways of diagnosing. I have recently heard of using the eyes to diagnose Alzheimer’s. When I did some research I didn’t find too much. I am thinking the information may be too new or I wasn’t on the right sites.
(this is in response to last week’s piece on lutein, eyes, and brain health)
We’d readily bet that the diagnostic criteria has to do with recording low levels of lutein in the eye (discernible by a visual examination of macular pigment optical density), and relying on the correlation between this and incidence of Alzheimer’s, but we’ve not seen it as a hard diagnostic tool as yet either—we’ll do some digging and let you know what we find! In the meantime, we note that the Journal of Alzheimer’s Disease (which may be of interest to you, if you’re not already subscribed) is onto this:
See also:
- Journal of Alzheimer’s Disease (mixture of free and paid content)
- Journal of Alzheimer’s Disease Reports (open access—all content is free)
Q: As to specific health topics, I would love to see someone address all these Instagram ads targeted to women that claim “You only need to ‘balance your hormones’ to lose weight, get ripped, etc.” What does this mean? Which hormones are they all talking about? They all seem to be selling a workout program and/or supplements or something similar, as they are ads, after all. Is there any science behind this stuff or is it mostly hot air, as I suspect?
Thank you for asking this, as your question prompted yesterday’s main feature, What Does “Balancing Your Hormones” Even Mean?
That’s a great suggestion also about addressing ads (and goes for health-related things in general, not just hormonal stuff) and examining their claims, what they mean, how they work (if they work!), and what’s “technically true but may
be misleading* cause confusion”*We don’t want companies to sue us, of course.
Only, we’re going to need your help for this one, subscribers!
See, here at 10almonds we practice what we preach. We limit screen time, we focus on our work when working, and simply put, we don’t see as many ads as our thousands of subscribers do. Also, ads tend to be targeted to the individual, and often vary from country to country, so chances are good that we’re not seeing the same ads that you’re seeing.
So, how about we pull together as a bit of a 10almonds community project?
- Step 1: add our email address to your contacts list, if you haven’t already
- Step 2: When you see an ad you’re curious about, select “share” (there is usually an option to share ads, but if not, feel free to screenshot or such)
- Step 3: Send the ad to us by email
We’ll do the rest! Whenever we have enough ads to review, we’ll do a special on the topic.
We will categorically not be able to do this without you, so please do join in—Many thanks in advance!
Share This Post
-
Eyes for Alzheimer’s Diagnosis: New?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Time!
This is the bit whereby each week, we respond to subscriber questions/requests/etc
Have something you’d like to ask us, or ask us to look into? Hit reply to any of our emails, or use the feedback widget at the bottom, and a Real Human™ will be glad to read it!
Q: As I am a retired nurse, I am always interested in new medical technology and new ways of diagnosing. I have recently heard of using the eyes to diagnose Alzheimer’s. When I did some research I didn’t find too much. I am thinking the information may be too new or I wasn’t on the right sites.
(this is in response to last week’s piece on lutein, eyes, and brain health)
We’d readily bet that the diagnostic criteria has to do with recording low levels of lutein in the eye (discernible by a visual examination of macular pigment optical density), and relying on the correlation between this and incidence of Alzheimer’s, but we’ve not seen it as a hard diagnostic tool as yet either—we’ll do some digging and let you know what we find! In the meantime, we note that the Journal of Alzheimer’s Disease (which may be of interest to you, if you’re not already subscribed) is onto this:
See also:
- Journal of Alzheimer’s Disease (mixture of free and paid content)
- Journal of Alzheimer’s Disease Reports (open access—all content is free)
Share This Post
-
Easing Lower Back Pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Lower back pain often originates from an unexpected culprit: your pelvis. Similar to how your psoas can contribute to lower back pain, when your pelvis tilts forward due to tight hip flexors, it can misalign your spine, leading to discomfort and pain. As WeShape shows us in the below video, one simple stretch can help realign your pelvis and significantly ease lower back pain.
Why Your Pelvis Matters
Sitting for long periods causes your hip flexors to shorten, leading to an anterior pelvic tilt. This forward tilt puts pressure on your spine and SI joint, causing pain and discomfort in the lower back. To help resolve this, you can work on correcting your pelvic alignment, helping to significantly reduce this pressure and alleviate related pain. And no, this doesn’t require any spinal cord stimulation.
Easy Variations for All
A lot of you recognise the stretch in this video; it’s quite a well-known kneeling stretch. But, unlike other guides, WeShape also provides a fantastic variation for those who aren’t mobile enough for the kneeling variation
So, if you can’t comfortably get down on the ground, WeShape outlines a brilliant standing variation. So, regardless of your mobility, there’s an option for you!
See both variations here:
Excited to reduce your lower back pain? We hope so! Let us know if you have any tips that you’d like to share with us.
Share This Post
Related Posts
-
Beyond Supplements: The Real Immune-Boosters!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Real Immune-Boosters
What comes to your mind when we say “immune support”? Vitamin C and maybe zinc? Those have their place, but there are things we can do that are a lot more important!
It’s just, these things are not talked about as much, because stores can’t sell them to you
Sleep
One of the biggest difference-makers. Get good sleep! Getting at least 7 hours decent sleep (not lying in bed, not counting interruptions to sleep as part of the sleep duration) can improve your immune system by three or four times.
Put another way, people are 3–4 times more likely to get sick if they get less sleep than that on average.
Check it out: Behaviorally Assessed Sleep and Susceptibility to the Common Cold
Eat an anti-inflammatory diet
In short, for most of us this means lots of whole plant foods (lots of fiber), and limited sugar, flour, alcohol.
For more details, you can see our main feature on this: Keep Inflammation At Bay!
You may wonder why eating to reduce inflammation (inflammation is a form of immune response) will help improve immune response. Put it this way:
If your town’s fire service is called out eleventy-two times per day to deal with things that are not, in fact, fires, then when there is a fire, they will be already exhausted, and will not do their job so well.
Look after your gut microbiota
Additionally, healthy gut microbiota (fostered by the same diet we just described) help keep your body pathogen-free, by avoiding “leaky gut syndrome” that occurs when, for example, C. albicans (you do not want this in your gut, and it thrives on the things we just told you to avoid) puts its roots through your intestinal walls, making holes in them. And through those holes? You definitely do not want bacteria from your intestines going into the rest of your body.
See also: Gut Health 101
Actually get that moderate exercise
There’s definitely a sweet-spot here, because too much exercise will also exhaust you and deplete your body’s resources. However, the famous “150 minutes per week” (so, a little over 20 minutes per day, or 25 minutes per day with one day off) will make a big difference.
See: Exercise and the Regulation of Immune Functions
Manage your stress levels (good and bad!)
This one swings both ways:
- Acute stress (like a cold shower) is good for immune response. Think of it like a fire drill for your body.
- Chronic stress (“the general everything” persistently stressful in life) is bad for immune response. This is the fire drill that never ends. Your body’s going to know what to do really well, but it’s going to be exhausted already by the time an actual threat hits.
Read more: Effects of Stress on Immune Function: the Good, the Bad, and the Beautiful
Supplement, yes.
These are far less critical than the above things, but are also helpful. Good things to take include:
Enjoy, and stay well!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
5 Ways To Beat Afternoon Energy Slumps
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Nisha Vora, of Rainbow Plant Life fame. After graduating from Harvard Law School, she realized she hated being a lawyer, and pivoted completely to become what she now is 12 years later, a chef and health coach.
Here are her tips for boosting energy through the day:
Caffeine timing
If you don’t do caffeine at all, no need to change that, but if you do, Vora advises that midday is the best time for it, with a very good rationale:
- of course it should not be too late in the day, because the elimination half-life of caffeine (4–8 hours to eliminate just half of the caffeine, depending on genes, call it 6 hours as an average though honestly for most people it will either be 4 or 8, not 6) is such that it can easily interfere with sleep for most people
- because caffeine is an adenosine blocker, not an adenosine inhibitor, taking caffeine in the morning means either there’s no adenosine to block, or it’ll just “save” that adenosine for later, i.e. when the caffeine is eliminated, then the adenosine will kick in, meaning that your morning sleepiness has now been deferred to the afternoon, rather than eliminated.
Another reminder that caffeine is the “payday loan” of energy. So, midday it is. No morning sleepiness to defer, and yet also not so late as to interfere with sleep.
See also: Calculate (And Enjoy) The Perfect Night’s Sleep
Simplify what can be simplified
This one’s not from a physiological basis, but rather, that a lot of the time most of us have much of our energy being taken by constant task-switching (what gets called multitasking, but as our brain is a single processor, it really means switching rapidly between different kinds of cognition, which is not efficient). In order to avoid that energy drain, try to streamline things and make a particular effort to not only single-task, but to do so without distractions.
Counterpoint: if you have unmedicated ADHD, then chances are you’ll do better with a single small distraction chosen by you, than trying to go without distractions, because your brain will find distractions anyway, so you might as well choose one (for many people it is background music, or a podcast or TV show that one doesn’t may attention to but it’s there) as a matter of harm reduction, and that way you’ll do better at focusing on your primary task than if your brain were reaching out for every and any possible distraction.
Manage your blood sugars
In particular, she advocates for avoiding sugary breakfasts, opting instead for protein, fat, and fiber-rich options. For more in this regard, see:
10 Ways To Balance Your Blood Sugars
Walk after meals
You don’t have to don hiking boots and “I am just going outside and may be some time“; rather, even a 2–5 minute walk after a meal helps regulate digestion and glucose levels, avoiding postprandial energy slumps.
So,
- if you have a treadmill, after eating is a great time to use it for a few minutes
- if you have stairs, now’s a great time to go up and down them a few times
One last technique for when everything else fails
We’ll quote her directly on this one:
❝Despite my best efforts, soemtimes I just have one of those days. Maybe I didn’t sleep well or I’m distracted by my never ending thoughts. If I need to be productive or energized on those days, I will do something that I absolutely hate:
I will take a cold shower.
And I hate it because I’m already always cold all the time, so why would I want to get a cold shower?
Well, it’s because cold water immersion has been shown to dramatically boost your dopamine levels, which gives you more energy and motivation.
In the moment though, it’s mostly painful and I hate everything and everyone around me.
But I know that if I can suffer through two minutes of a cold shower, I will feel so refreshed.❞
There are more benefits than just that, though, see:
A Cold Shower A Day Keeps The Doctor Away?
Want more from Nisha Vora?
We reviewed one of her books a while back:
The Vegan Instant Pot Cookbook – by Nisha Vora
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Felt Time – by Dr. Marc Wittmann
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book goes far beyond the obvious “time flies when you’re having fun / passes slowly when bored”, or “time seems quicker as we get older”. It does address those topics too, but even in doing so, unravels deeper intricacies within.
The author, a research psychologist, includes plenty of reference to actual hard science here, and even beyond subjective self-reports. For example, you know how time seems to slow down upon immediate apparent threat of violent death (e.g. while crashing, while falling, or other more “violent human” options)? We learn of an experiment conducted in an amusement park, where during a fear-inducing (but actually safe) plummet, subjective time slows down yes, but measures of objective perception and cognition remained the same. So much for adrenal superpowers when it comes to the brain!
We also learn about what we can change, to change our perception of time—in either direction, which is a neat collection of tricks to know.
The style is on the dryer end of pop-sci; we suspect that being translated from German didn’t help its levity. That said, it’s not scientifically dense either (i.e. not a lot of jargon), though it does have many references (which we like to see).
Bottom line: if you’ve ever wished time could go more quickly or more slowly, this book can help with that.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: