Using the”Task Zero” approach
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Jonathan Frakes Asks You Things” Voice:
- Do you ever find yourself in a room and wonder what you’re doing there?
- Or set about a to-do list, but get quickly distracted by side-quests?
- Finally get through to a person in a call center, they ask how they can help, and your mind goes blank?
- Go to the supermarket and come out with six things, none of which were the one you came for?
This is a “working memory” thing and you’re not alone. There’s a trick that can help keep you on track more often than not:
Don’t try to overburden your working memory. It is very limited (this goes for everyone to a greater or lesser degree). Instead, hold only two tasks at once:
- Task zero (what you are doing right now)
- Task one (your next task)
When you’ve completed task zero, task one becomes the new task zero, and you can populate a new task one from your to-do list.
This way, you will always know what you’re doing right now, and what you’re doing next, and your focus will be so intent on task zero, that you will not get sidetracked by task seventeen!
Happy focusing
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ozempic vs Five Natural Supplements
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Semaglutide (GLP-1 agonist) drugs Ozempic and Wegovy really do work for losing weight, provided one then remains on these expensive drugs for life. Dr. Jin Sung recommends a supplements-based approach, instead.
Natural Alternatives
Dr. Sung recommends:
- Berberine, which increases production and secretion of GLP-1.
- Probiotics, which increase GLP-1 secretion. In particular he recommends Akkermansia municiphila which secretes P9, and this protein stimulates GLP-1 production and secretion.
- Psyllium, a soluble dietary fiber which will increase short-chain fatty acids which then help with increasing GLP-1.
- Curcumin, which enhances L-cell numbers, in turn promoting and increasing GLP-1 secretion. Also, curcumin may prolong gastric emptying, and increase insulin sensitivity.
- Ginseng, of which the bioactive compound stimulates secretion of GLP-1, and also has anti-diabetic effects.
Dr. Sung explains more about each of these in his video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to know more?
You might enjoy our previous main feature looking at some of the pros and cons:
Take care!
Share This Post
-
What is childhood dementia? And how could new research help?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Childhood” and “dementia” are two words we wish we didn’t have to use together. But sadly, around 1,400 Australian children and young people live with currently untreatable childhood dementia.
Broadly speaking, childhood dementia is caused by any one of more than 100 rare genetic disorders. Although the causes differ from dementia acquired later in life, the progressive nature of the illness is the same.
Half of infants and children diagnosed with childhood dementia will not reach their tenth birthday, and most will die before turning 18.
Yet this devastating condition has lacked awareness, and importantly, the research attention needed to work towards treatments and a cure.
More about the causes
Most types of childhood dementia are caused by mutations (or mistakes) in our DNA. These mistakes lead to a range of rare genetic disorders, which in turn cause childhood dementia.
Two-thirds of childhood dementia disorders are caused by “inborn errors of metabolism”. This means the metabolic pathways involved in the breakdown of carbohydrates, lipids, fatty acids and proteins in the body fail.
As a result, nerve pathways fail to function, neurons (nerve cells that send messages around the body) die, and progressive cognitive decline occurs.
Childhood dementia is linked to rare genetic disorders. maxim ibragimov/Shutterstock What happens to children with childhood dementia?
Most children initially appear unaffected. But after a period of apparently normal development, children with childhood dementia progressively lose all previously acquired skills and abilities, such as talking, walking, learning, remembering and reasoning.
Childhood dementia also leads to significant changes in behaviour, such as aggression and hyperactivity. Severe sleep disturbance is common and vision and hearing can also be affected. Many children have seizures.
The age when symptoms start can vary, depending partly on the particular genetic disorder causing the dementia, but the average is around two years old. The symptoms are caused by significant, progressive brain damage.
Are there any treatments available?
Childhood dementia treatments currently under evaluation or approved are for a very limited number of disorders, and are only available in some parts of the world. These include gene replacement, gene-modified cell therapy and protein or enzyme replacement therapy. Enzyme replacement therapy is available in Australia for one form of childhood dementia. These therapies attempt to “fix” the problems causing the disease, and have shown promising results.
Other experimental therapies include ones that target faulty protein production or reduce inflammation in the brain.
Research attention is lacking
Death rates for Australian children with cancer nearly halved between 1997 and 2017 thanks to research that has enabled the development of multiple treatments. But over recent decades, nothing has changed for children with dementia.
In 2017–2023, research for childhood cancer received over four times more funding per patient compared to funding for childhood dementia. This is despite childhood dementia causing a similar number of deaths each year as childhood cancer.
The success for childhood cancer sufferers in recent decades demonstrates how adequately funding medical research can lead to improvements in patient outcomes.
Dementia is not just a disease of older people. Miljan Zivkovic/Shutterstock Another bottleneck for childhood dementia patients in Australia is the lack of access to clinical trials. An analysis published in March this year showed that in December 2023, only two clinical trials were recruiting patients with childhood dementia in Australia.
Worldwide however, 54 trials were recruiting, meaning Australian patients and their families are left watching patients in other parts of the world receive potentially lifesaving treatments, with no recourse themselves.
That said, we’ve seen a slowing in the establishment of clinical trials for childhood dementia across the world in recent years.
In addition, we know from consultation with families that current care and support systems are not meeting the needs of children with dementia and their families.
New research
Recently, we were awarded new funding for our research on childhood dementia. This will help us continue and expand studies that seek to develop lifesaving treatments.
More broadly, we need to see increased funding in Australia and around the world for research to develop and translate treatments for the broad spectrum of childhood dementia conditions.
Dr Kristina Elvidge, head of research at the Childhood Dementia Initiative, and Megan Maack, director and CEO, contributed to this article.
Kim Hemsley, Head, Childhood Dementia Research Group, Flinders Health and Medical Research Institute, College of Medicine and Public Health, Flinders University; Nicholas Smith, Head, Paediatric Neurodegenerative Diseases Research Group, University of Adelaide, and Siti Mubarokah, Research Associate, Childhood Dementia Research Group, Flinders Health and Medical Research Institute, College of Medicine and Public Health, Flinders University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
From banning junk food ads to a sugar tax: with diabetes on the rise, we can’t afford to ignore the evidence any longer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are renewed calls this week for the Australian government to implement a range of measures aimed at improving our diets. These include restrictions on junk food advertising, improvements to food labelling, and a levy on sugary drinks.
This time the recommendations come from a parliamentary inquiry into diabetes in Australia. Its final report, tabled in parliament on Wednesday, was prepared by a parliamentary committee comprising members from across the political spectrum.
The release of this report could be an indication that Australia is finally going to implement the evidence-based healthy eating policies public health experts have been recommending for years.
But we know Australian governments have historically been unwilling to introduce policies the powerful food industry opposes. The question is whether the current government will put the health of Australians above the profits of companies selling unhealthy food.
benjamas11/Shutterstock Diabetes in Australia
Diabetes is one of the fastest growing chronic health conditions in the nation, with more than 1.3 million people affected. Projections show the number of Australians diagnosed with the condition is set to rise rapidly in coming decades.
Type 2 diabetes accounts for the vast majority of cases of diabetes. It’s largely preventable, with obesity among the strongest risk factors.
This latest report makes it clear we need an urgent focus on obesity prevention to reduce the burden of diabetes. Type 2 diabetes and obesity cost the Australian economy billions of dollars each year and preventive solutions are highly cost-effective.
This means the money spent on preventing obesity and diabetes would save the government huge amounts in health care costs. Prevention is also essential to avoid our health systems being overwhelmed in the future.
What does the report recommend?
The report puts forward 23 recommendations for addressing diabetes and obesity. These include:
- restrictions on the marketing of unhealthy foods to children, including on TV and online
- improvements to food labelling that would make it easier for people to understand products’ added sugar content
- a levy on sugary drinks, where products with higher sugar content would be taxed at a higher rate (commonly called a sugar tax).
These key recommendations echo those prioritised in a range of reports on obesity prevention over the past decade. There’s compelling evidence they’re likely to work.
Restrictions on unhealthy food marketing
There was universal support from the committee for the government to consider regulating marketing of unhealthy food to children.
Public health groups have consistently called for comprehensive mandatory legislation to protect children from exposure to marketing of unhealthy foods and related brands.
An increasing number of countries, including Chile and the United Kingdom, have legislated unhealthy food marketing restrictions across a range of settings including on TV, online and in supermarkets. There’s evidence comprehensive policies like these are having positive results.
In Australia, the food industry has made voluntary commitments to reduce some unhealthy food ads directly targeting children. But these promises are widely viewed as ineffective.
The government is currently conducting a feasibility study on additional options to limit unhealthy food marketing to children.
But the effectiveness of any new policies will depend on how comprehensive they are. Food companies are likely to rapidly shift their marketing techniques to maximise their impact. If any new government restrictions do not include all marketing channels (such as TV, online and on packaging) and techniques (including both product and brand marketing), they’re likely to fail to adequately protect children.
Food labelling
Food regulatory authorities are currently considering a range of improvements to food labelling in Australia.
For example, food ministers in Australia and New Zealand are soon set to consider mandating the health star rating front-of-pack labelling scheme.
Public health groups have consistently recommended mandatory implementation of health star ratings as a priority for improving Australian diets. Such changes are likely to result in meaningful improvements to the healthiness of what we eat.
Regulators are also reviewing potential changes to how added sugar is labelled on product packages. The recommendation from the committee to include added sugar labelling on the front of product packaging is likely to support this ongoing work.
But changes to food labelling laws are notoriously slow in Australia. And food companies are known to oppose and delay any policy changes that might hurt their profits.
Health star ratings are not compulsory in Australia. BLACKDAY/Shutterstock A sugary drinks tax
Of the report’s 23 recommendations, the sugary drinks levy was the only one that wasn’t universally supported by the committee. The four Liberal and National party members of the committee opposed implementation of this policy.
As part of their rationale, the dissenting members cited submissions from food industry groups that argued against the measure. This follows a long history of the Liberal party siding with the sugary drinks industry to oppose a levy on their products.
The dissenting members didn’t acknowledge the strong evidence that a sugary drinks levy has worked as intended in a wide range of countries.
In the UK, for example, a levy on sugary drinks implemented in 2018 has successfully lowered the sugar content in UK soft drinks and reduced sugar consumption.
The dissenting committee members argued a sugary drinks levy would hurt families on lower incomes. But previous Australian modelling has shown the two most disadvantaged quintiles would reap the greatest health benefits from such a levy, and accrue the highest savings in health-care costs.
What happens now?
Improvements to population diets and prevention of obesity will require a comprehensive and coordinated package of policy reforms.
Globally, a range of countries facing rising epidemics of obesity and diabetes are starting to take such strong preventive action.
In Australia, after years of inaction, this week’s report is the latest sign that long-awaited policy change may be near.
But meaningful and effective policy change will require politicians to listen to the public health evidence rather than the protestations of food companies concerned about their bottom line.
Gary Sacks, Professor of Public Health Policy, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
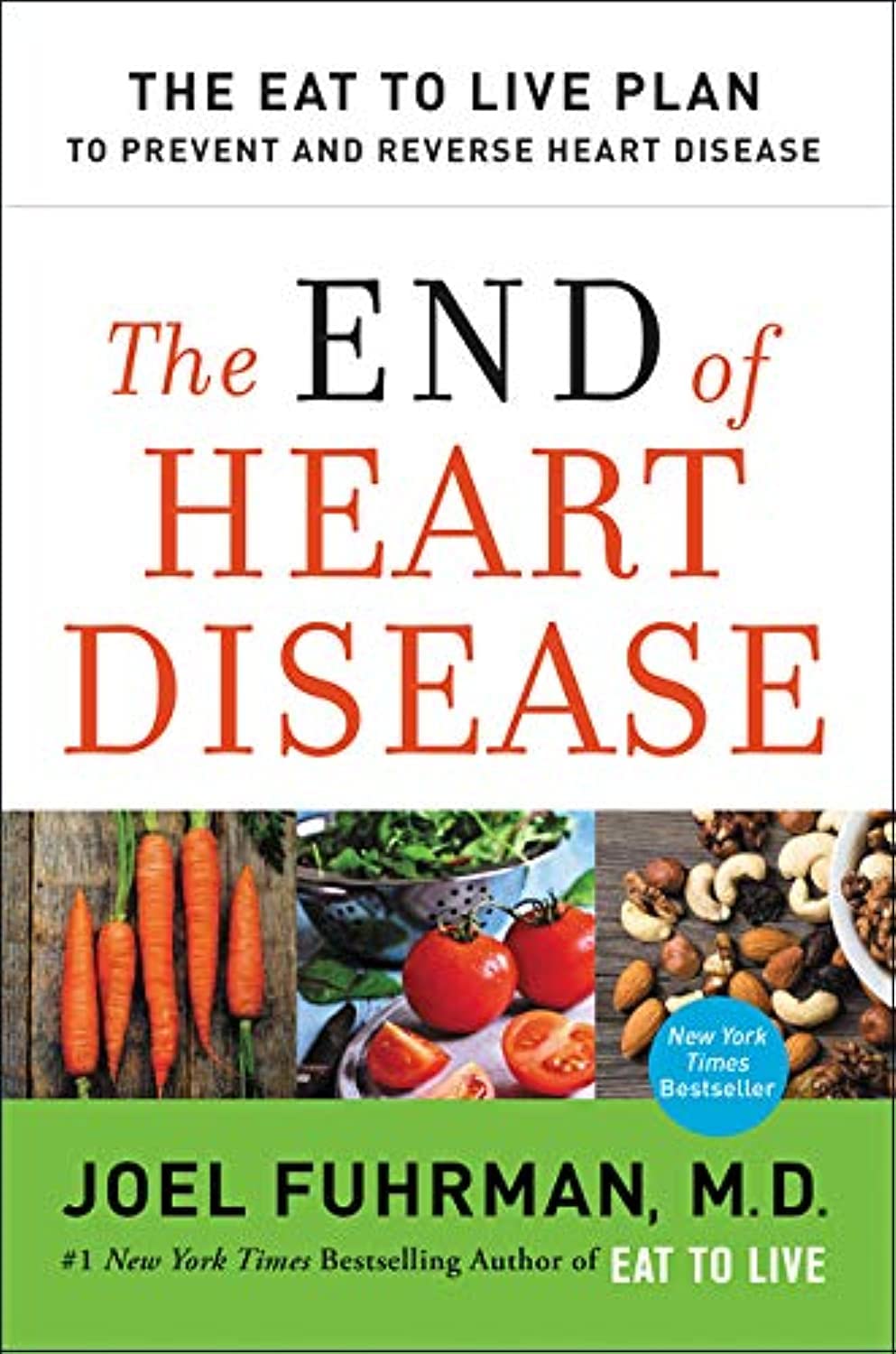
The End of Heart Disease – by Dr. Joel Fuhrman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed another of Dr. Fuhrman’s books, “Eat To Live”, and this time, he’s focusing specifically on preventing/reversing heart disease.
Dr. Fuhrman takes the stance that our food can either kill or heal us, and we get to choose which. As such, nutrition is central to his heart-healthy plan; he mostly leaves matters of exercise, sleep, etc to other sources.
His dietary approach is mostly uncontroversial: for example, advices include: enjoy nutritionally dense foods, skip processed foods, eat at least mostly plants, skip the added salt. A slightly more controversial aspect is that he advocates for avoiding cooking oils, including the healthiest oils, including olive and avocado, which are by current scientific consensus considered heart-healthy in moderation. As in, not even just heart-neutral, but rather, they actively improve triglycerides.
He compares different cardioprotective diets, and while he’s not unbiased, he does provide 40 pages of scholarly references, so we may understand that at the very least, his approach is sound.
There are also recipes—94 pages of them—for any who might wonder “how do I cook without…?” and some ingredient he would rather you omit.
The style is information-dense (and this is a 448-page book) but still very readable.
Bottom line: if you’re serious about improving your heart health, this book can help a lot with that.
Click here to check out The End Of Heart Disease, and end heart disease for yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Longans vs Lychees – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing longans to lychees, we picked the lychees.
Why?
These two fruits are more closely related than they look from the outside, both being members of the soapberry family. However, there are some differences:
In terms of macros, longans have more protein while lychees have more carbs, and they are equal on fiber, giving longans the lower glycemic index. They’re both good, but longans nominally take the win on this one.
When it comes to vitamins, longans have more of vitamins B1, B2, and C, while lychees have more of vitamins B3, B6, B9, E, K, and choline, making for a respectable win for lychees in this category.
In the category of minerals, longans have more copper and potassium, while lychees have more calcium, iron, manganese phosphorus, and zinc. Thus, a win for lychees here too.
It’s worth looking at polyphenols too—lychees have around 10x more, which is notable.
Adding up the categories makes for an overall win for lychees, but by all means enjoy either or both! Diversity is good.
Want to learn more?
You might like to read:
Replacing Sugar: Top 10 Anti-Inflammatory Sweet Foods ← longans and lychees both make the list
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cows’ Milk, Bird Flu, & You
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to dairy products, generally speaking, fermented ones (such as most cheeses and yogurts) are considered healthy in moderation, and unfermented ones have their pros and cons that can be argued and quibbled “until the cows come home”. We gave a broad overview, here:
Furthermore, you may recall that there’s some controversy/dissent about when human babies can have cows’ milk:
When can my baby drink cow’s milk? It’s sooner than you think
So, what about bird flu now?
Earlier this year, the information from the dairy industry was that it was nothing to be worried about for the time being:
Bird Flu Is Bad for Poultry and Dairy Cows. It’s Not a Dire Threat for Most of Us — Yet.
More recently, the latest science has found:
❝We found a first-order decay rate constant of −2.05 day–1 equivalent to a T99 of 2.3 days. Viral RNA remained detectable for at least 57 days with no degradation. Pasteurization (63 °C for 30 min) reduced infectious virus to undetectable levels and reduced viral RNA concentrations, but reduction was less than 1 log10.
The prolonged persistence of viral RNA in both raw and pasteurized milk has implications for food safety assessments and environmental surveillance❞
You can find the study here:
Infectivity and Persistence of Influenza A Virus in Raw Milk
In short: raw milk keeps the infectious virus; pasteurization appears to render it uninfectious, though viral RNA remains present.
This is relevant, because of the bird flu virus being found in milk:
World Health Organization | H5N1 strain of bird flu found in milk
To this end, a moratorium has been placed on the sale of raw milk, first by the California Dept of Public Health (following an outbreak in California):
California halts sales of raw milk due to bird flu virus contamination
And then, functionally, by the USDA, though rather than an outright ban, it’s requiring testing for the virus:
USDA orders testing of milk supply for presence of bird flu virus
So, is pasteurized milk safe?
The official answer to this, per the FDA, is… Honestly, a lot of hand-wringing and shrugging. What we do know is:
- the bird flu virus has been found in pasteurized milk too
- the test for this is very sensitive, and has the extra strength/weakness that viral fragments will flag it as a positive
- it is assumed that the virus was inactivated by the pasteurization process
- it could, however, have been the entire virus, the test simply does not tell us which
In the FDA’s own words:
❝The pasteurization process has served public health well for more than 100 years. Even if the virus is detected in raw milk, pasteurization is generally expected to eliminate pathogens to a level that does not pose a risk to consumer health❞
So, there we have it: the FDA does not have a reassurance exactly, but it does have a general expectation.
Source: US Officials: Bird flu viral fragments found in pasteurized milk
Want to know more?
You might like this mythbusting edition we did a little while back:
Pasteurization: What It Does And Doesn’t Do ← this is about its effect on risks and nutrients
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: